Standard Arterial R econstruction
Matthew H. Levine
DEFINITION
Arterial reconstruction of a whole liver allograft occurs as one of the standard anastomoses in orthotopic liver transplantation; the others including the suprahepatic vena cava, the infrahepatic vena cava in caval interposition transplantation, the portal vein, and the bile duct reconstruction. The arterial inflow to the liver is of the utmost importance, as the biliary system is highly reliant on arterially delivered oxygenated blood, and hepatic artery thrombosis (HAT) in the peritransplant period is a significant cause of morbidity, mortality, and retransplantation.
PATIENT HISTORY AND PHYSICAL FINDINGS
The deceased donor procurement operation must be performed with care and precision. Both donor and recipient can have variable anatomy, which must be addressed properly at the time of procurement.
IMAGING AND OTHER DIAGNOSTIC STUDIES
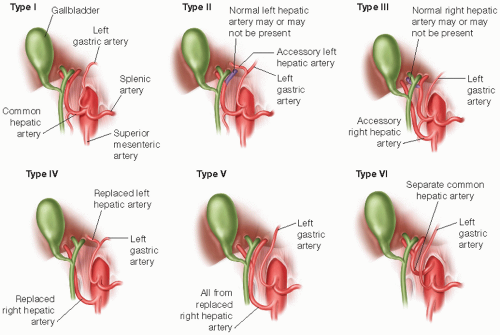
A review of the donor anatomy is possible in some cases prior to procurement if a computed tomography (CT) angiogram has been performed as part of the donor evaluation. Most liver recipients will have had contrast-enhanced cross-sectional imaging to rule out or stage hepatocellular carcinoma (HCC), which can define the recipient arterial anatomy. These studies can provide clues about possible variant arterial anatomy.
Transarterial chemoembolization (TACE) of HCC can lead to arterial thrombosis of the extrahepatic artery. In cases of prior liver resection or prior liver transplantation, a careful review of the prior operative notes can inform the approach to the hepatic arteries.
SURGICAL MANAGEMENT
Preoperative Planning
The goal is to reconstruct the arterial supply to the liver graft with as few anastomoses or conduits as necessary. Use of an arterial conduit graft is associated with a small increased risk of HAT.4
Discussion of HAT and its consequences, including the possible requirement for retransplantation, should be part of the surgical consent.
TECHNIQUES
PREPARATION OF THE RECIPIENT ARTERY
After exploring the abdomen, mobilizing the falciform ligament and taking down attachments of the left lateral segment of the liver to the diaphragm, incise the hepatogastric ligament and ligate a replaced or accessory left hepatic artery, if present. This allows retractors to be placed for ideal exposure of the porta hepatis.
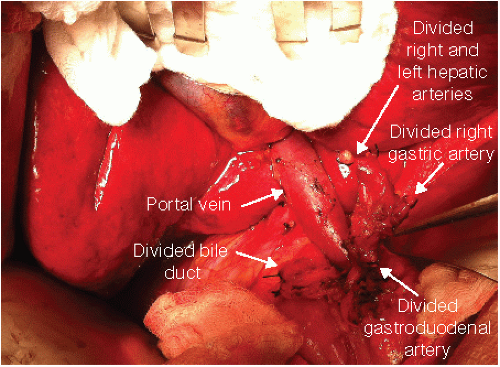
Begin the dissection of the porta hepatis as high as possible near the hilum of the liver. The right and left hepatic arteries (RHA and LHA) are generally anterior structures and are ligated and divided, preserving the RHA/LHA bifurcation as a potential arterial branch patch site on the recipient side.

FIG 2 • The standard hepatic arterial anatomy is shown from celiac origin to the hepatic hilum with all celiac branch vessels identified. Variants are common as shown in FIG 1.
Dissect in the avascular plane posterior to the proper hepatic artery (PHA), anterior to the portal vein (PV) to the gastroduodenal artery (GDA) using electrocautery or sharp dissection. Care must be taken to not apply undue traction or thermal injury to the artery that can lead to intimal damage and dissection. The right gastric artery is often encountered and should be ligated and divided during this dissection. A small supraduodenal artery may be present and ligated as well (FIG 2).
Dissect the common hepatic artery 1 to 2 cm below the GDA. This can be done at this point in the procedure or can be left just prior to implantation.
Test the celiac inflow by compressing or clamping the GDA (particularly if it is large) and assessing the pulsatility of the PHA without the contribution of the GDA. If the pulse is diminished without the GDA present, the GDA is preserved and a more distal anastomosis site is selected. If the pulse in the common hepatic artery is poor, stenosis of the celiac origin or presence of an arcuate ligament must be considered.
The fully prepared dissection of the recipient hepatic artery is shown (FIG 3).
PREPARATION OF THE DONOR ARTERY
Preparation of the donor artery begins with safe and meticulous procurement of the donor liver. Depending on the technique used, the common hepatic artery between the GDA branch and the splenic artery may be dissected during procurement. The hepatic artery more distal to the GDA is typically not dissected to prevent injury, arterial spasm, and devitalizing the bile duct.
The presence of any accessory or replaced hepatic arteries (right or left) must be noted, and these must be carefully preserved. Aberrant anatomy may be associated with a higher rate of HAT or biliary complications.5
In liver procurement without pancreas or small bowel, preserve the entire celiac axis with the donor liver. If a replaced RHA is present, include the superior mesenteric artery (SMA) origin as well. In the case of a pancreas or small bowel procurement, the celiac axis remains with the liver graft but divide the splenic artery to allow closure of the splenic stump on the liver side of the graft. Both the pancreas and small bowel grafts require the SMA and
judicious division of this artery distal to a replaced RHA origin (if present) is required.
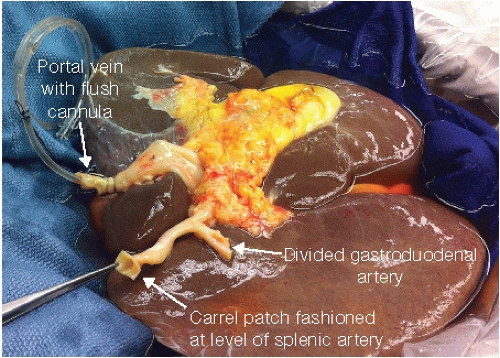
FIG 4 • The fully dissected donor hepatic artery. Here, a Carrel patch was formed at the level of the splenic artery bifurcation due to atherosclerotic disease in the donor aorta and celiac trunk.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree