CONDITION |
DESCRIPTION |
MANAGEMENT |
IMAGE |
|---|
Superficial hemangioma (formerly called “strawberry” or capillary hemangioma) |
Benign proliferation of endothelial cells that starts as macule and grows into dome-shaped papule or nodule
Most often followed by spontaneous involution (“graying”) |
Observation or treatment with intralesional or systemic steroids, or laser ablation, especially if lesions compromise function |
 |
Deep hemangioma (formerly called “cavernous” hemangioma) |
Deep dermal and subcutaneous red to violaceous nodule; regression often incomplete |
Observation or treatment with intralesional, systemic steroids, or laser ablation, especially if lesions compromise function |
 |
Macular stains (“angel’s kisses,” “salmon patches”) |
Red macules located on forehead, eyelids, nose, or upper lip
Most often regress by 2 years of age |
None indicated |
 |
Stork bites |
Red macules on back of neck
Persist in 25% of adults |
None indicated |
 |
Nevus flammeus (port-wine stain) |
Congenital malformation of blood vessels
Usually appears at birth |
Laser therapy |
 |
Nevus spilus (speckled lentiginous nevus) |
Tan patches characterized by numerous darker macules or papules |
Surgical excision for cosmetic reasons only |
 |
Becker’s nevus (pigmented hairy nevus) |
Pigmented hairy nevus that is located over chest, shoulder, or back
Often appears at puberty |
None; surgical excision or laser ablation for cosmetic reasons only |
 |
Nevus sebaceous |
Congenital hamartoma, with plaques on head or neck
Thickens at puberty
Small risk of malignant degeneration, mainly to basal cell carcinoma |
Excision |
 |
Nevus lipomatosis |
Solitary or grouped proliferation of fatty tissue
Lesions are asymptomatic, soft, skin-colored to yellow papules, nodules, or plaques, with predilection for upper thighs, pelvic, lumbar, and buttock areas |
Surgical excision for cosmetic reasons only |
 |
Epidermal nevi |
Congenital hamartomas with various presentations: verrucous, inflammatory, linear, multiple, or comedonal |
Excision, observation, or cryotherapy, with topical steroids for inflammatory type, topical retinoids for comedonal type |
 |
Mongolian spots |
Macular, flat, blue or blue-gray skin markings that appear at birth or shortly thereafter on the sacral area and back
Most prevalent among Asians and African Americans
Often fade spontaneously |
None |
 |
Nevus of Ota |
Gray-blue melanin pigmentation of sclera of the eye
Seen in Japanese, as well as in Africans, African Americans, and East Indians |
Laser therapy |
 |
Acropustulosis of infancy |
Recurrent crops of small pruritic vesicles that evolve into pustules
Involves the palms and soles, most often in black newborns and infants
Remits spontaneously |
Topical steroids |
 |
Gianotti-Crosti syndrome (acrodermatitis papulosa) |
Self-limited, sometimes pruritic exanthem associated with many viral agents and immunizations
Pale, pink to flesh-colored papules (sometimes flat-topped) in symmetric distribution on extremities |
None |
 |
Urticaria pigmentosum |
Multiple red-brown macules, usually on the trunk |
Antihistamines and/or topical steroids, if symptomatic |
 |
Solitary mastocytoma (the mastocytosis syndrome can involve multiple organs and become chronic; it is not discussed here) |
Lesions become a wheal (urticate) when rubbed or stroked; this change is referred to as Darier’s sign, which is explainable on the basis of mast cell degranulation induced by physical stimulation
Most cases resolve spontaneously
Usually yellow-brown rubbery plaque that urticates or blisters (bullous urticaria pigmentosum) after rubbing
Resolves spontaneously |
No treatment necessary |
 |
Tinea amiantacea |
Thick, adherent scale on scalp and in hair |
Keratolytics, followed by topical steroids when scale is cleared |
 |
Talon noir (tennis heel) |
Self-limited, multiple, black petechiae of heel after minor trauma |
Paring, protective heel pad |
 |
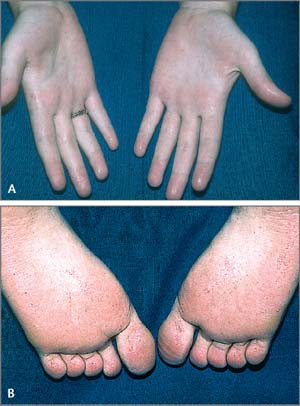
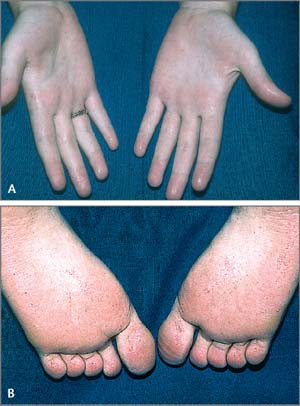
Pitted keratolysis |
Pits in stratum corneum of soles; caused by prolonged occlusion, hyperhidrosis, and bacterial proteinase proliferation
Malodorous |
Topical erythromycin, clindamycin, or oral erythromycin
Wearing cotton socks to prevent moisture buildup |
 |
Lichen striatus |
Idiopathic linear inflammatory eruption
Consists of papules that coalesce into linear, unilateral plaques that appear most often on extremities
Resolves spontaneously |
Topical steroids |
 |
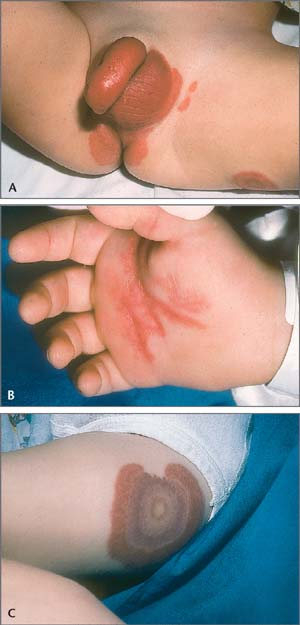
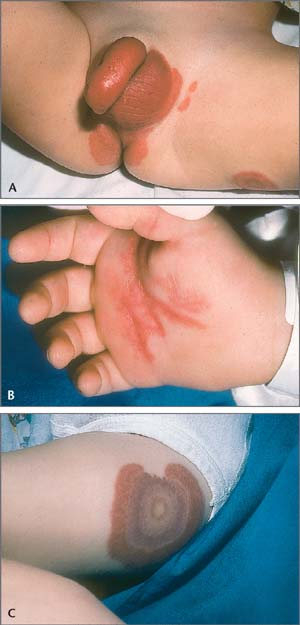
Perianal streptococcal dermatitis (perianal cellulitis) |
Affects children 3 to 4 years of age
Caused by group A beta-hemolytic streptococci
Bright pink to red erythema that extends 2 to 3 cm from anus; infrequently accompanied by itching, fissuring, pain, and mucoid discharge
May become more of a cellulitis, with possible pain on defecation |
Penicillin V combined with topical Bactroban (mupirocin) ointment or cream twice a day |
 |
Juvenile xanthogranuloma |
Occurs in infancy and early childhood
Lesions composed of histiocytic cells; benign, smooth, firm, red-brown papules and nodules that change to yellow
Resolves spontaneously |
None necessary |
 |
Lichen nitidus |
Occurs on thighs, arms, trunk, and genitalia
Idiopathic, asymptomatic, small (1 to 2 mm), flat-topped, shiny, skin-colored papules |
Topical steroids, if necessary |
 |
Hyperhidrosis |
Usually starts in early teen years
Excessive sweating, particularly axillae, palms, and soles |
Topical:
Aluminum and zirconium antiperspirants
Topical 20% aluminum chloride hexahydrate in absolute alcohol, anticholinergics, aldehydes, and tannic acid
Iontophoresis
Systemic:
Oral anticholinergic medications
Injection: botulinum toxin
Surgical:
Liposuction
Sympathectomy |
 |
Subcutaneous fat necrosis of newborn |
Firm, erythematous nodules and plaques on trunk, arms, buttocks, thighs, and cheeks in otherwise healthy infants
Self-limited |
None necessary |
 |
Lymphangioma circumscriptum |
Congenital hamartoma of lymphatics
Consists of small clusters of vesicles (“frog spawn”) |
Surgical excision, laser ablation, cryosurgery, electrocautery, or sclerotherapy |
 |
Acute hemorrhagic edema of infancy (Finkelstein’s disease) |
Large, urticarial or annular, targetoid, purpuric plaques found primarily on face, ears, and extremities; presumably immune complex–mediated
Self-limited |
None necessary |
 |
Staphylococcal scalded skin syndrome (SSSS) |
Occurs mostly in neo-nates in neonatal or day care nurseries
Toxin-mediated type of exfoliative dermatitis caused by toxigenic strains of Staphylococcus aureus Lesions range from localized bullous impetigo to extensive blistering and exfoliation |
Dicloxacillin |
 |