Solar Elastosis
Todd Schlesinger
Clinton Favre
BACKGROUND
Skin aging is a complex, naturally occurring phenomenon that involves the accumulation of abnormal elastin (elastic tissue) and loss of collagen within the dermis. Skin aging may be classified as intrinsic aging and extrinsic aging. Intrinsic aging is predominantly the genetically determined loss of elastic tissue or other skin components over the passage of time.1 Extrinsic aging results from the environmental effects such as ultraviolet radiation (UVR).2 Ultraviolet rays are a part of the electromagnetic spectrum emitted by the sun and the primary cause of the damaging effects on the skin. Although cutaneous aging is inevitable, the addition of prolonged and excessive sun exposure accelerates the process of skin damage significantly, thus causing an expedited decline in skin function.2 Photoaging is the term used to describe premature aging of the skin through chronic sun exposure of UVR. Prolonged UVR exposure can lead to the development of many disorders that range in seriousness from benign to life threatening.
Solar elastosis, also known as actinic elastosis, is a condition that leads to a collection of abnormal elastin (elastic tissue) and loss of collagen in the dermis of the skin due to the harmful effects of UVR.3 Considered the most common disorder of sun damage, solar elastosis appears on areas that receive persistent sun exposure, such as face, back and sides of the neck, V area of the neck and upper chest, extensor arms, and dorsal hands. In its most common appearance, solar elastosis presents as heavily thickened, wrinkled, yellow skin, but it can
present in different forms, which cause the disease to be broad and elusive to diagnose.
present in different forms, which cause the disease to be broad and elusive to diagnose.
PRESENTATION
The common cutaneous presentations of solar elastosis include increased thickness of the skin, yellow hue, irregular pigmentation, xerosis, and fissures. Often accompanying solar elastosis is the presence of rhytids (wrinkling/furrowing), lentigines, keratoses, and telangiectasias.
DIAGNOSIS
Clinical Diagnosis
The skin appears thickened and dry, with coarse rhytids and a yellow hue. On close inspection, there is a white to yellow pebbly appearance to the skin surface. Areas that are most pronounced in their discoloration and altered texture are the upper lip, periorbital regions, malar eminences, nose, and lateral aspects of the forehead. Sites with the most sun exposure are preferentially affected. Open comedones may be present in the periorbital regions and temples. Thickened yellow plaques or papules may be present on the hands or firm nodules on the ears. Multiple translucent papules may also be found on the sun-exposed areas of the face, neck, dorsum of hands, and back. These solar elastosis subtypes have been defined and are presented in detail in the following text.
Histopathology
Solar elastosis shows basophilic degeneration of elastotic fibers in the dermis, separated from the epidermis by a narrow band of normal-appearing collagen (grenz zone) with collagen fibers arranged horizontally. This is the best evident with the help of special stains. The degree of elastosis correlates with the cumulative amount of UVR to which the skin has been exposed.4
Histologically, the dermis is the most affected by UVR. Naturally aged skin shows a decrease in types I and III collagen within the reticular dermis; however, studies have indicated that in photoaged skin, there is an accelerated decrease of collagen in areas that received chronic sun exposure.1 Increased levels of matrix metalloproteinases (MMPs) are found when the skin receives prolonged and chronic sun exposure.1 MMPs are enzymes that degrade collagen and other proteins in the dermis, and studies have shown that UVR promoted the production and increased gene expression of collagenase, a member of the MMP family, within the extracellular matrix.1,5,6 Reduction of collagen content has been considered to be a possible reason for the formation of wrinkles, which is the most prominent characteristic of solar elastosis, and is caused by the weakening of the epidermis and dermis.7
Subtypes
Cutis Rhomboidalis Nuchae
Cutis rhomboidalis is the most easily recognizable variant of solar elastosis. It is found almost exclusively on the nape of the neck, and affected areas feature heavily thickened and coarsely wrinkled skin containing a yellowish, leathery pigmentation.8 Cutis rhomboidalis is trademarked for the intersecting, profound geometrical patterns of furrows often forming rhomboidal shapes (Figure 5.2.1). In very severe cases, comedones and small cysts have been seen.
The etiology of this disease is still uncertain, but researchers hypothesized that constant muscle movement on the back of the neck in the setting of chronic sun exposure might play a crucial role in the formation of this disorder.9
Treatment choice for this variant depends on how severe the visible characteristics are represented. Laser resurfacing, such as ablative, nonablative, and fractional, is considered best for severe cases and produces
the optimal results. Chemical peels are another option that is less invasive and can produce moderate improvement.
the optimal results. Chemical peels are another option that is less invasive and can produce moderate improvement.
Milian Citrine Skin
Arguably the most common form and least distinctive of solar elastosis, Milian citrine skin, consists of 2 variants: Milian citrine skin and an atrophic variant. Milian citrine skin frequently refers to wrinkling, inelastic, erythema, telangiectasia, irregular pigmentation, and possible malignant neoplasms. In the nonatrophic variant, the most common characteristics seen in the affected area are a leathery appearance with a yellow hue dyspigmentation, furrows, and scales (Figure 5.2.2). In the atrophic version, telangiectasias and hyperplastic sebaceous glands are the most prominent feature with subtle erythema and moderate yellow hue of the skin, and unlike the nonatrophic version, deep wrinkling is not as common or prominent.3 The atrophic version of Milian citrine skin appears most often with individuals of Celtic origin featuring fair skin (Figure 5.2.3).3
The etiology for both versions of Milian citrine skin is UVR. In the atrophic version, telangiectasias are the most noticeable characteristic due to the loss of polarity of epidermal cells and the thickened, increased size of the blood vessel walls. UVR interferes with the skin’s ability to repair itself, causing the skin to lose polarity. The thickened and increased size of the blood vessel walls are due to inflammatory mediators produced by the skin in response to the UVR (UVB). The inflammatory mediators seep into the dermis, irritating the blood vessels in the dermis and causing them to swell. UVA rays also play a role by permanently dilating blood vessels and making them more prominent. Wrinkles are not as noticeable as in the telangiectasias.
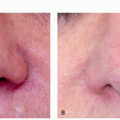
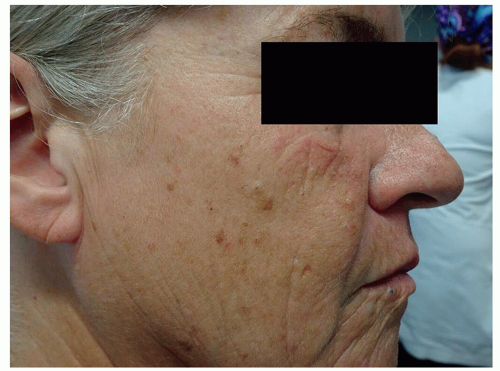 FIGURE 5.2.2 Milian citrine skin featuring rhytids, leathery appearance, and irregular pigmentation with a yellow hue. |
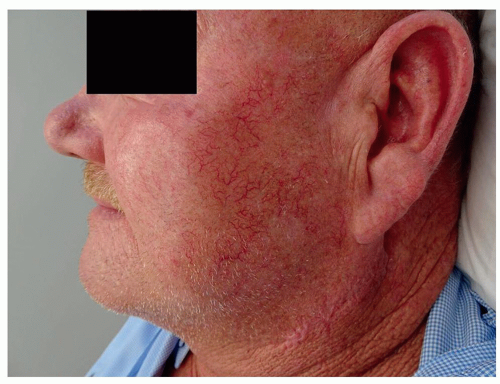 FIGURE 5.2.3 Milian citrine skin, atrophic variant consisting of well-represented telangiectasias and hypertrophic sebaceous glands. |
Both of the variants discussed are benign but can be viewed as a potential cosmetic problem. Laser resurfacing treatments offer the best results for the nonatrophic variant, but other less risky treatments that are still effective include topical retinoids, antioxidants, and chemical peels. Because of the prominent telangiectasias in the atrophic variant, intense pulsed light (IPL) laser or pulsed dye lasers (PDLs) are the best options.
Striated Beaded Lines
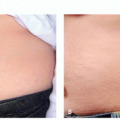
Striated beaded lines are most prominently found on the neck and the upper chest area. Striated beaded lines consist of hyperplastic sebaceous glands that appear as white to yellowish papules that form prominent parallel beaded lines (Figure 5.2.4).10 Chronic sun exposure can lead to photodamage causing the hypertrophic sebaceous gland to be visualized.11
A histopathological examination of this disorder shows epidermal thinning as well as epidermal hyperplasia. UVR is known to cause a loss of polarity and hyperplastic tendencies within the epidermis of the skin. Loss of collagen through UV exposure causes a loss of support of the follicular duct, and dilation of the follicular duct can occur creating wider follicular ostia. This can also lead to the appearance of prominent sebaceous glands.
 FIGURE 5.2.4 Striated beaded lines featuring hypertrophic sebaceous glands to be prominent and forming parallel beaded lines. |
Striated beaded lines can be a difficult disorder to treat because of the delicacy of the sebaceous glands. Aggressive treatments such as ablative laser systems can potentially be too harmful to the sebaceous gland and may cause severe scarring. Treatments with lower side-effect risks, such as nonablative fractional or IPLs, are a better option for this disorder. Both treatments offer satisfactory results with minimal risk for adverse side effects. Electrodessication is also a viable option for patients who are concerned about the potential harm produced by a laser system.
Favre-Racouchot Syndrome
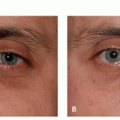
Favre-Racouchot syndrome is associated with cysts and solar comedones that can appear as open (blackheads) or closed (whiteheads) along with nodular elastosis affecting the malar and periorbital skin.12 Often this syndrome is referred to as “nodular elastosis with cysts and comedones.” In the early stages of this syndrome, yellow plaques form along with open or closed comedones, but as chronic sun exposure increases, the plaques can turn into nodules developing more comedones and epidermal cysts (Figure 5.2.5).12 The biggest difference between the comedones of acne vulgaris and the comedones of Favre-Racouchot is that the comedones in Favre-Racouchot are noninflammatory. Any area that has the possibility of prolonged sun exposure has a chance of the syndrome occurring in that location.
As previously discussed, UVR results in a loss of collagen through the upregulation of MMPs in the dermis of the skin. Collagen is the structural support of skin giving its volume and shape. Without collagen, follicular ducts are not able to stay closed, and in most cases, the ducts will open wider and expand. Keratinous debris will dilate the widened follicular ducts and become plugged, leading to the formation of open or closed comedones.13
 FIGURE 5.2.5 Favre-Racouchot syndrome represented by cysts and comedones with nodular elastosis primarily on the malar and periorbital region. |
Before various treatments for Favre-Racouchot can begin, the collected keratinous debris within the follicular duct needs to be extracted. Once completely extracted, treatments such as laser resurfacing and topicals are viable options that offer solid results.
Actinic Comedonal Plaque
Histologically, this disorder is identical to the Favre-Racouchot syndrome, but the difference between the 2 disorders is that the plaques described in the actinic comedonal disorder exhibit erythematous confluent nodules that appear pierced by numerous small holes, cribriform, with comedolike structures (Figure 5.2.6).14,15 Unlike Favre-Racouchot syndrome, actinic comedonal plaque can be found in atypical locations such as the chest or forearms.14
Researchers have proposed possible theories on why actinic comedonal plaque varies from Favre-Racouchot, but the literature is inconclusive. The only upheld theory is that UVR exposure is considered the fundamental element to their pathogenesis. The same treatments for Favre-Racouchot are used for actinic comedonal plaque.
Dubreuilh Elastoma
Dubreuilh elastoma can appear as a single lesion or multiple grouped lesions on areas of high sun exposure, particularly the neck, face, or chest. These lesions are represented by thickened, yellow plaque
usually featuring distinct margins. Dubreuilh elastoma may coexist in the same area as Favre-Racouchot syndrome.16
usually featuring distinct margins. Dubreuilh elastoma may coexist in the same area as Favre-Racouchot syndrome.16
Actinic Granuloma
Actinic granuloma appears in sites that receive chronic sun, such as the face, neck, arms, and chest. The early stages of actinic granuloma feature lesions as a flesh-colored to pink papules.17 As the disorder progresses, the papules begin to coalesce and become annular plaques that feature either a normal or atrophic center.18 Typically, the raised edges appear red, whereas the interior of the plaque is pale. Actinic granuloma can be almost indistinguishable from granuloma annulare or granulomatous disorders.
Actinic granuloma occurs due to the inflammatory response in areas of chronic sun exposure, and histological reports demonstrate these inflammatory responses within the dermis of the skin.19 For this reason, researchers suggest that actinic granuloma occurs due to the inflammatory response to degenerated elastic fibers caused by UVR.
Keratoelastoidosis Marginalis
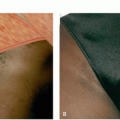
The lesions in this disorder appear in a linear arrangement featuring small fleshy to yellowish papules, almost exclusively found on the palms, web skin, and the junction of the dorsal and palmar skin of the hands.20 If left untreated, the disease can slowly progress, leading to the formation of calcified nodules and plaques.
UVR seems to play the biggest contributing factor in the growth of this disorder. However, another possible contributing component is the repeated and chronic trauma caused by the long-term use of tools often used in manual labor jobs.20 Repetitive pressure causes the epidermis to thicken as a protective measure, and UVR also causes epidermal thickening. The combination of these 2 aspects plays a role in the development of this disorder.
Treatments for keratoelastoidosis marginalis include ointments incorporating vitamin D, topical retinoids, salicylic acid, and possibly cryotherapy for severe cases.
Solar Elastotic Bands
Solar elastotic bands are a very uncommon and unusual form of solar elastosis featuring cordlike plaque bands appearing on the forearms extending around to the flexor surfaces of the forearm. These bands consist of nude to yellow nodules and papules and are often accompanied by actinic purpura with abnormal elastic fibrils.21
Elastotic Nodule of the Ear
Elastotic nodules are asymptomatic papules that first appear on the antihelix of the bilateral ears.22 Initially, the lesions arise as small, pink, and pearly, and this disorder is often confused with basal cell carcinoma or amyloid. It was later shown that these lesions may also arise on the helix of the ear, leading to the development of chondrodermatitis nodularis helicis, which can be painful.23
Adult-Onset Colloid Milium
These lesions are characterized as amber to flesh-colored papules found within sun-exposed areas, such as the face, ears, neck, and hands.
Chronic sun exposure plays an important factor in the formation of this disorder, but it has been suggested that repeated trauma and exposure to phenols could play a role in the pathogenesis. Studies have found eosinophilic colloid masses in the papillary dermis along with solar elastosis around the surrounding areas.24
Grading Scale
To understand how to treat this elusive disorder, physicians need to be able to grade the severity of solar
elastosis in individuals. Solar elastosis features numerous characteristics, such as wrinkling/furrowing, thickness of the skin, telangiectasia, irregular pigmentation, and underlying yellow hue. Alexiades-Armenakas et al have created a comprehensive grading scale, shown in Table 5.2.1, that includes individual categories for common characteristics found in photoaged skin.25 This grading scale will help physicians categorize patients with solar elastosis to help guide treatment choices.
elastosis in individuals. Solar elastosis features numerous characteristics, such as wrinkling/furrowing, thickness of the skin, telangiectasia, irregular pigmentation, and underlying yellow hue. Alexiades-Armenakas et al have created a comprehensive grading scale, shown in Table 5.2.1, that includes individual categories for common characteristics found in photoaged skin.25 This grading scale will help physicians categorize patients with solar elastosis to help guide treatment choices.
Differential Diagnosis
Pseudoxanthoma elasticum
Elastoderma
Papillary dermal elastolysis
Focal dermal elastosis
Nodular amyloidosis
Popular mucinosis
PATHOGENESIS
The etiology of solar elastosis is hypothesized to be due to the combined effect of chronic sun exposure with constant repetitive muscle movement. The chronic sun exposure creates the leathery and wrinkled appearance as stated earlier, and the constant voluntary muscle movement in the back of the neck causes deeper and more prominent wrinkles to be formed.
Constant and repeated muscle movement will cause wrinkles to be more prominent over time. When the muscle contracts, the overlying skin will stretch to be able to accommodate, and during this process, the connective tissue will begin to break. When connective tissue breaks, the skin becomes inelastic, resulting in a visible wrinkle. The combination of repetitive neck movement with chronic sun exposure (UV) accelerates the formation of these wrinkles. As stated previously, UV exposure decreases the amount of collagen and elastin found in the reticular dermis of the skin, causing the skin to become inelastic.6,9 In addition, collagen production naturally decreases with age, and with chronic UV exposure, there is a net loss of collagen and elastin within the dermoepidermal junction (DEJ), causing severe structural changes such as drooping and sagging skin. As more elastin and collagen are degraded, the DEJ continues to weaken, resulting in deeper and more prominent wrinkles. The loss of collagen also causes follicular ducts to become more open, and keratin can quickly fill in the ducts causing the formation of comedones.
The elastin quantity decreases over time; however, in areas of prolonged UV exposure, the elastin quantity increases corresponding with the amount of sun exposure.26 It remains unclear how the elastotic material is formed. However, researchers have suggested a few theories regarding this topic. UVR stimulates new elastin to be produced from fibroblasts.27 Other research suggests that new elastotic material found in solar elastosis is derived from pre-existing elastic fibers.28,29 An increase in inflammatory infiltrates, perivenular lymphohistiocytic infiltrate, has been hypothesized as a potential driver for the degradative process of elastin leading to new elastotic material to appear irregular, a condition termed chronic heliodermatitis.30 Although this hypothesis is unconfirmed, there is evidence to support this claim. Although the origin of the elastotic material is known, there is also an increase in elastotic material found in solar elastosis, and it appears that the newly formed elastin replaces the degraded collagen. Not only does the elastotic material take the place of the degraded collagen, but elastin produced from the UVR also has an abnormal, amorphous appearance compared with the original elastin found most prominently at the DEJ.30 The elastic fibers are thickened, distorted, and disorganized, forming a tangled mass in the papillary and reticular dermis, which causes a weakening of the DEJ, and thereby increasing the severity of wrinkles.
Studies have shown that in photoaged skin, there is an increase in the total population of cells, including the number of fibroblasts; however, in photodamaged skin, the affected fibroblasts appear more flattened than in nonphotoaged skin.29,31 Along with fibroblasts, the amount of Merkel cells and melanocytes seems to increase with prolonged sun exposure. Sites with chronic photodamage can see a moderate decrease in the size and total amount of blood vessels found in the upper dermis.29 The degree of severity for solar elastosis corresponds with the amount of chronic sun exposure over time.
The epidermis is also affected by chronic sun exposure. The epidermal layer is thicker in photoaged skin than in non-sun exposed skin.1 In addition, loss of polarity or atypia appears to be commonly expressed in many of the epidermal cells in photodamaged skin, which can lead to the development of skin cancers, such as basal cell carcinoma and squamous cell carcinoma.32,33 If left untreated, both cancers can be life threatening and locally destructive.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree