Skin Problems in Ostomates: Introduction
|
Skin Problems in Patients with Abdominal Stomas (Ostomates)
A stoma is a surgically created opening onto the skin of part of the gastrointestinal or urinary tract in order to drain the effluent from that viscus. The most frequently performed stomas are ileostomies, colostomies, and ileal conduits (urostomies or urinary diversion). The commonest indications for stoma surgery are inflammatory bowel disease, malignancy and neurological problems. A patient with a stoma is usually termed an “ostomist” or “ostomate.”
There are estimated to be more than 1.4 million ostomates in the United States and 100,000 in the United Kingdom and Ireland. Some stomas are temporary, with surgical anastomosis delayed, pending resolution of the acute disorder. Temporary stomas are often “loop stomas” where a loop of bowel is brought to the skin surface and part of the wall removed to allow preferential drainage into a stoma pouch in order to relieve a distal problem, for example, perianal ulceration. Such stomas are more frequently associated with skin problems secondary to leaks.1 Many stomas formed for malignant indications can be seen as palliative procedures.
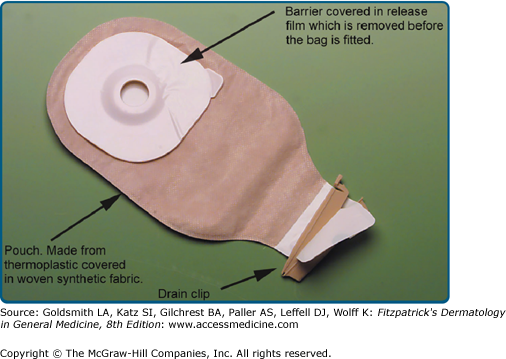
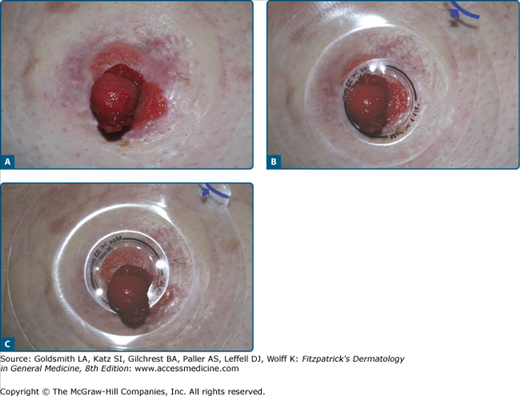
A stoma appliance is essentially a device for collecting stoma effluent with a high degree of comfort and security until it can be disposed of. There continues to be promising advances in the design of stoma bags. Essentially, the device is a pouch or bag held in place over the stoma by an adhesive skin barrier made solely or partly from hydrocolloid. Many ileostomists and urostomists use two-piece appliances where the barrier remains on the skin for 2–4 days and is detachable; disposable bags are changed as necessary. Appliances with convexity on the surface next to the skin are available for patients with short or buried stomas (Fig. 97-1). Useful recent innovations include softer convex appliance that apply less pressure on the skin and collars or sleeves that fit snugly around the stoma before applying the bag thereby reducing the chance of leaks of effluent or intestinal mucus under the barrier.
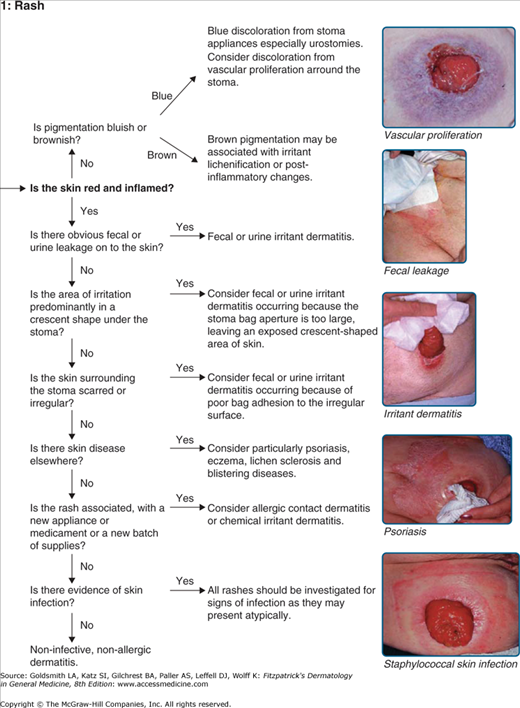
As many as two-thirds of ostomates experience skin problems that interfere with the normal use of their stoma appliance,2,3 and such dermatoses are the commonest reasons for a visit to outpatient stoma services.4,5 The majority of these problems are irritant reactions, usually dermatitis secondary to leaks from the stoma; however, there are also a number of other well-defined irritant reactions. Common coincidental dermatoses, particularly psoriasis and constitutional eczema, account for around 15% of the diseases seen.2,6 An approach to diagnosing peristomal dermatoses is given in eFigure 97-1.1.
Dermatitis most frequently results from the chronic leakage of effluent onto the skin because the patient is using an inappropriately shaped appliance or one with too large a hole for their stoma. The most common cause is the remodeling of the stoma and abdominal wall that occurs in the months after surgery, whereby a stoma usually becomes a little shorter and thinner, resulting in leaks unless a correctly fitting appliance is selected (Figs. 97-2, 97-3, 97-4, 97-5, and 97-6). Leaks will also occur when patients gain a lot of weight after surgery and the effective length of their stoma diminishes because it becomes buried by subcutaneous fat.7 Irregular scarring after surgery or retraction of the stoma, may also be associated with chronic leakage. Such irregularities can be corrected with topically applied pastes. One effective alternative is to use collagen fillers (Porcine collagen Permacol™)8 to recontour the skin surface. Short stomas (<2 cm long), loop ileostomies and stomas formed as emergency procedures are more likely to be associated with skin problems.1,9 Chronically irritated skin can become markedly hyperkeratotic and acanthotic (Fig. 97-7). These problems can be prevented and resolved by careful postsurgical follow-up by the enterostomal therapist (ET; stoma nurse specialist) to ensure that the correct appliance is being used. Severe, acute irritant dermatitis can be effectively treated with a short course of topical corticosteroid while longer term appliance modifications are being undertaken (Table 97-1).
Figure 97-6
Irritant contact dermatitis from leaks occurring when reclining at night resulting in a cycle of poor bag adhesion and further leaks. Patient was unable to sleep sitting up and the rash did not respond to barriers or steroid tape. It eventually responded to applications of beclomethasone via a metered dose inhaler allowing proper bag adhesion and less leakage.
|
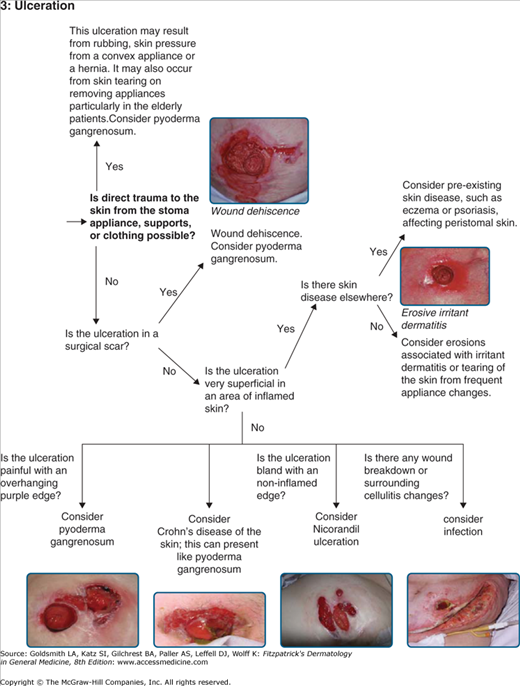
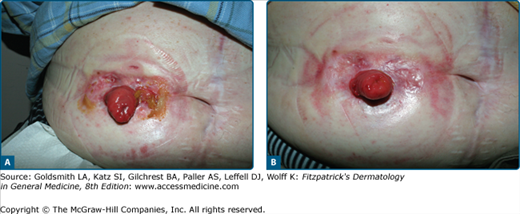
Anxieties about possible leaks and odors can lead to excessively frequent bag changing, which may cause an irritant dermatitis by stripping the skin. Patients may, for the same reasons, wear waist belts too tightly thereby causing pressure damage even ulcers (eFig. 97-7.1) and occasionally necrosis. Whatever the cause of skin inflammation, a vicious cycle can develop when the damaged skin prevents proper bag adhesion necessitating more frequent bag changes.12 Careful counseling is usually necessary in order to reassure the patient regarding leaks.
eFigure 97-7.1
Pressure-induced ulcers in a middle-aged man with inflammatory bowel disease. This patient with a long-standing ileostomy became concerned about leaks and wore a belt tightly (imprint seen). Furthermore, the lugs on the belt were worn downwards onto the skin rather than away from the skin. A. This has resulted in pressure necrosis, ulceration and subsequent leaks and dermatitis. B. The problem resolved one month after wearing the belt the correct way round and more loosely.
Approximately 15% of ostomates with skin problems suffer from a chronic or recurrent dermatitis for which no irritant, allergic, or infective cause can be found, and where primary skin disease is ruled out.2 In the absence of a primary treatable cause, the use of topical corticosteroid lotions is appropriate. Most patients require only occasional short courses for a maximum of 4 weeks’ duration (Table 97-1). A small number of patients require intermittent applications longer term. Provided that the frequency of application is no more than once every 10 days, steroid atrophy of the skin appears to be unusual.
In ileostomy patients with short bowel, the output may be very high and corrosive due to the enzyme and bile salt content. In this situation, some leaks are inevitable, despite the use of proprietary barrier preparations or soothing lotions. Where the irritation has resulted in an eroded dermatitis, sucralfate powder applied at every stoma bag change can be very effective. In addition to forming a sticky barrier, the preparation is thought to promote healing.13 Surgical scars and even large striae (eFig. 97-7.2) can lead to ulcerations and bag failures, which may respond to topical carmellose sodium or sucralfate powders. Wound dehiscence can cause severe difficulties for bag adhesion (eFig. 97-7.3) and presents particular challenges for nursing management where the dermatologist may be called upon for advice as part of the multidisciplinary team.14
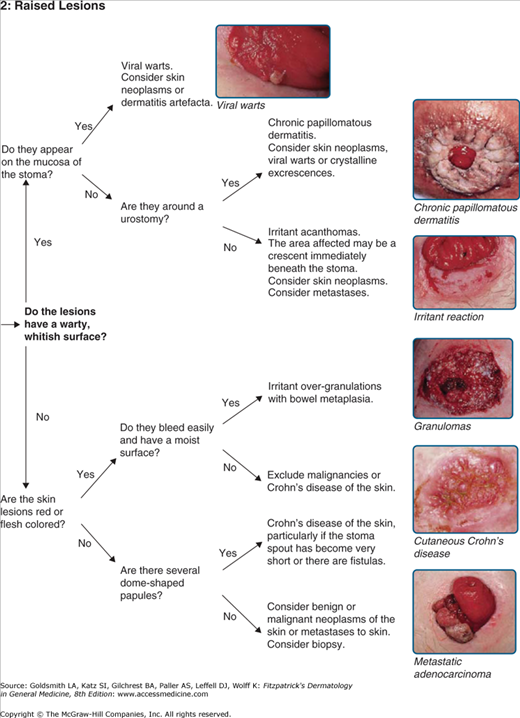
This term refers to clinical appearance of warty excrescences around urostomies resulting from leaks and pooling of urine on the peristomal skin (eFig. 97-7.4). Recurrent urinary tract infections appear to increase the likelihood of chronic papillomatous dermatitis (CPD) probably due to the presence of ammonia from urea-splitting bacteria. Histologically, there is massive hyperkeratosis and acanthosis. Pseudoepitheliomatous hyperplasia may also be a feature but is not universal. The histology is therefore not specific and comparable to that of other irritant reactions. Verrucous lesions with similar appearances are occasionally seen affecting ileostomies15 (Fig. 97-5). In severe cases, the lesions can encroach on the stoma and cause stenosis (Fig. 97-8). When the leaking of urine is caused by a receding stoma, CPD will resolve rapidly if a convex-backed appliance is used to increase the effective length of the urostomy and thereby stop leaks. Acetic acid soaks (10% domestic vinegar in water)16 at each bag change are effective in some cases (eFig. 97-8.1). Larger excrescences may be shaved off under local anesthetic to allow a bag with a smaller aperture to be used. In severe cases, surgical revision of the stoma may be required.
Figure 97-8
Chronic papillomatous dermatitis affecting a urostomy in a patient who is using a bag with too large an aperture. The red area is stoma and is becoming stenosed by the warty papules. The brown pigmentation is a typical finding in long-standing urostomies in all races. (Courtesy of Anita Eriksson, Karolinska Institute, Stockholm, Sweden.)