Hair Transplantation and Alopecia Reduction: Introduction
|
Background
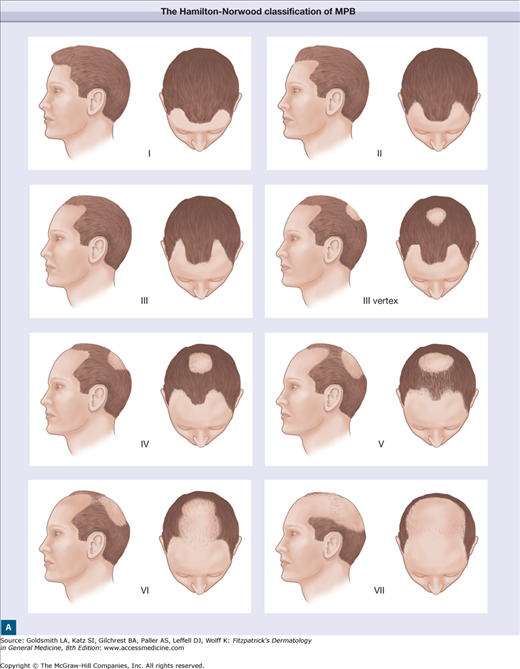
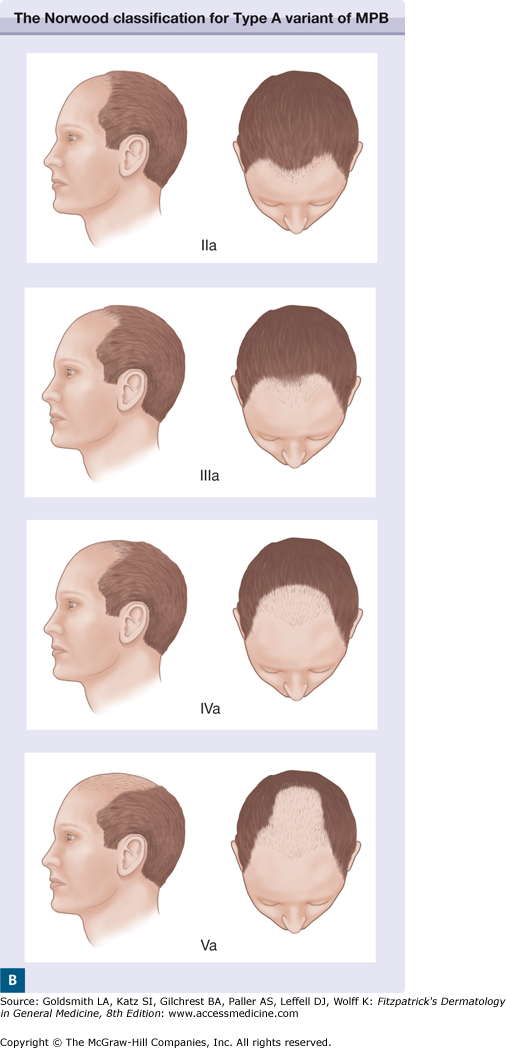
Hamilton and Norwood described the degrees of severity of MPB from a mild Type I to a severe Type VII3,4 (Fig. 256-2). Fortunately, a large majority of male patients do not progress past Types VI: Norwood found that at age 79 only 11% of men have Type VII MPB (Table 256-1), and Unger found that among men older than 65 only 13.7% have Type VII MPB5 (Table 256-2). Thus, if one treats all or most patients as if they will develop Type VI MPB, one is being reasonably cautious. An exception is for cases with a family history of Type VII MPB, in which case it is wiser to assume an evolution to Type VII MPB.
Age (years) | |||||||
|---|---|---|---|---|---|---|---|
18–29 | 30–39 | 40–49 | 50–59 | 60–69 | 70–79 | ≥80 | |
Type I | 110 (60%) | 60 (36%) | 55 (33%) | 45 (28%) | 29 (19%) | 18 (17%) | 12 (16%) |
Type II | 52 (28%) | 43 (26%) | 38 (22%) | 32 (20%) | 24 (16%) | 20 (19%) | 11 (14%) |
Type III | 14 (6%) | 30 (18%) (3V)a | 37 (20%) (15V)a | 34 (23%) (15V)a | 22 (15%) (10V)a | 16 (16%) (7V)a | 12 (16%) (8V)a |
Type IV | 4 (3%) | 16 (10%) | 15 (10%) | 21 (9%) | 17 (12%) | 13 (13%) | 9 (12%) |
Type V | 3 (2%) | 10 (6%) | 13 (8%) | 15 (10%) | 22 (15%) | 13 (13%) | 9 (12%) |
Type VI | 2 (1%) | 4 (3%) | 7 (4%) | 10 (7%) | 19 (13%) | 11 (11%) | 10 (13%) |
Type VII | 0 | 2 (1%) | 5 (3%) | 4 (3%) | 16 (10%) | 11 (11%) | 14 (17%) |
Total | 185 (100%) | 165 (100%) | 165 (100%) | 156 (100%) | 149 (100%) | 102 (100%) | 77 (100%) |
Type | Age (years) | |||
|---|---|---|---|---|
65–69 | 70–74 | 75–79 | 80+ | |
I | 2 (3.6%) | 5 (6.2%) | 4 (5.5%) | 2 (1.7%) |
II | 9 (16.4%) | 7 (8.6%) | 7 (9.6%) | 12 (10.1%) |
III | 4 (7.3%) | 15 (18.5%) | 18 (24.7%) | 11 (9.2%) |
IV | 10 (18.2%) | 16 (19.8%) | 8 (11.0%) | 10 (8.4%) |
V | 6 (10.9%) | 7 (8.6%) | 10 (13.7%) | 16 (13.4%) |
VI | 13 (23.6%) | 19 (23.5%) | 16 (21.9%) | 37 (31.1%) |
VII | 11 (20.0%) | 12 (14.8%) | 10 (13.7%) | 31 (26.1%) |
Total | 55 (100%) | 81 (100%) | 73 (100%) | 119 (100%) |
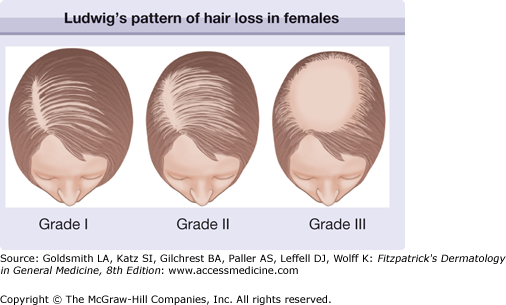
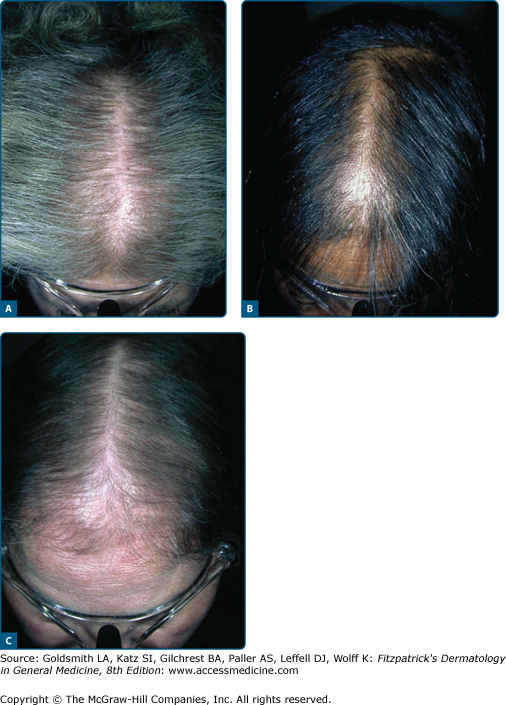
Ludwig described three degrees of FPHL6 (Fig. 256-3), while Olsen developed a distinct classification system based on her observation of a “Christmas-tree” pattern of hair loss7 (Fig. 256-4). According to Hamilton’s study, 79% of postpubertal females develop at least a mild Hamilton/Norwood pattern of hair loss.3 Most female patients do not have a sufficiently high density donor rim to surgically treat all of the affected alopecic areas. For this reason, some practitioners believe that women are rarely candidates for hair restoration surgery (HRS)—a view shared by the general public. In the authors’ experience, however, the opposite is true.8 A poor donor/recipient ratio does not preclude surgery, but does require a treatment plan that focuses on cosmetically strategic areas. In women, this corresponds to the frontal area and the part-line, which is usually a 5-mm-wide anteroposterior corridor (Fig. 256-5). The thickened hair in these areas can then be styled in a way that camouflages untreated areas. When this is done, the cosmetic improvement is significant, and patient satisfaction is high.
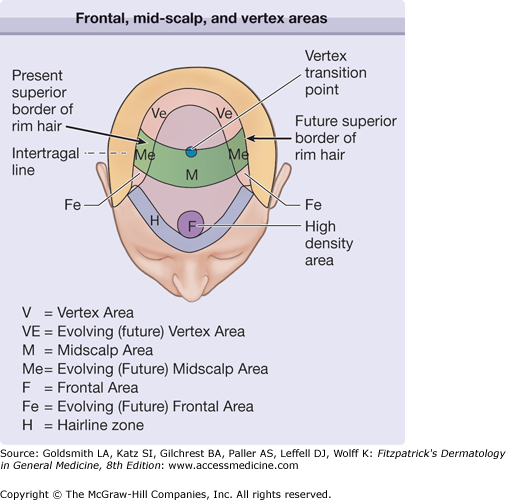
In men, the transplantation of areas of MPB should be conceptualized as consisting of four areas: (1) a frontal area extending from the proposed hairline to a coronal line drawn perpendicularly between the tragus of each ear; (2) a midscalp area extending from the posterior border of the frontal area to a point where the caudal scalp changes its orientation from parallel to the ground to more or less vertical; (3) a vertex area that consists of the remainder of the alopecic regions; and finally (4) evolving areas of alopecia adjacent to the aforementioned three major areas, which on close inspection contain relatively sparse hair (Figs. 256-6, 256-7, and 256-8). Commonly, each transplant session treats one of the three major areas, plus adjacent evolving areas. Occasionally, the treatment of evolving areas of hair loss is deferred to later sessions in order to transplant a larger proportion of obvious areas of hair loss. In such cases, sufficient numbers of grafts must be left in reserve to permit the future treatment of these areas, unless an isolated frontal forelock is the ultimate goal.
Figure 256-6
A schematic showing frontal, midscalp, and vertex areas, as well as evolving areas of MPB in a patient with Type VI MPB. Ideally, each of the three major areas is treated at the same time as the evolving areas of MPB lateral to them. Typically, only one major area and evolving area are treated during each session, though “touch-up” thickening of previously transplanted sites may also be carried out concomitantly.
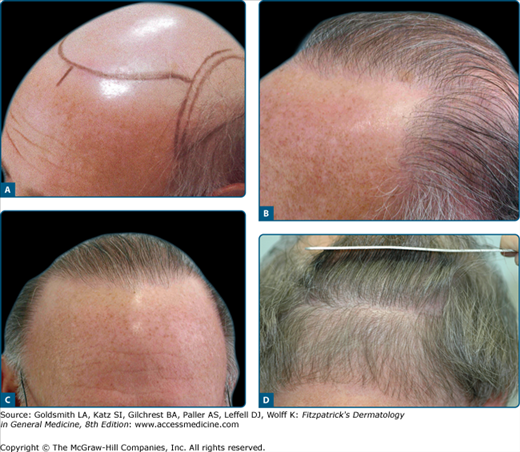
Figure 256-7
A. A patient with early MPB. The grease pencil line outlines the areas to be treated, including the supratemporal humps that are currently hair bearing, but can be reasonably expected to lose hair with the passage of time. Designing and transplanting these regions has the advantage of allowing the lateral points of the new hairline to be placed more superiorly than they otherwise could be. This is because if the supratemporal humps were not transplanted and proceeded to lose their hair, the new hairline would eventually end in alopecic areas. B. The same patient six months after being transplanted 2,137 FU. The hairline in this patient intersected the temporal humps relatively inferiorly. His family history and examination suggested that he would ultimately develop Type V or, at worst, Type VI MPB, and he had relatively dense hair in his donor area.
Figure 256-8
A. A 67-year-old patient, with Type VII MPB and a relatively sparse donor area before treatment. The black crayon lines outline the areas to be treated. Reconstruction of the supra-temporal humps permits a more superior position for the new hairline. This decreases the anteroposterior length of the frontal area, resulting in the consumption of fewer grafts. This hairline runs parallel to the ground when viewed laterally, despite its more superior positioning. B. A side view of the same patient 11 months after his second hair transplant and a total of 3,211 FU (one session was to the frontal area and one was further posterior). The advantages of recreating the supratemporal humps are more obvious for patients with Type VII MPB than for patients who have, or will, develop less severe MPB. C. A frontal view of the same patient. D. The donor area scar 9 months after the third transplant in this patient.
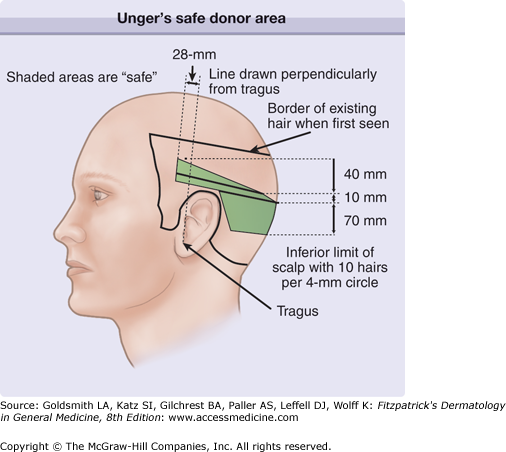
In Unger’s study of 328 males over the age of 65 years, he delineated an area within the zone of rim hair that contained 8 or more hairs per 4-mm circle5 (Fig. 256-9). He referred to this as the safe donor area (SDA). For most patients, the equivalent of 3–5 strips, each of which is 10 mm, can be excised from the SDA during their lifetime. Each of those strips produces 1,500–2,750 FU, depending on the density of the donor hair.
Figure 256-9
Unger’s safe donor area for 80% of patients under the age of 80 years, as determined from studies of 328 men aged 65 years or older.5
Patient Selection
During the initial consultation, surgeons must clarify whether the hair loss is temporary or responsive to medical treatment. A comprehensive discussion of this subject is available elsewhere in this textbook. Provided this is not the case, the first step in the surgical evaluation of a patient is to assess the current and expected size of the donor and recipient areas. An accurate assessment of the donor/recipient ratio depends on professional experience, the family history of patterned hair loss and most importantly the patient’s age. The second step is to evaluate hair characteristics. Box 256-1 lists the hair characteristics of the best hair transplant candidates. Not all of these characteristics are necessary for a satisfactory result, but each one improves the final cosmetic appearance (Fig. 256-10).
The authors do not follow any strict rules on patient selection with respect to the stage of hair loss, age, or gender. In regards to the stage of hair loss, it is important to note that the recipient area does not need to be completely alopecic in order to successfully operate. In fact, there are important advantages to transplanting at an earlier stage of MPB, although treating such areas demands a high degree of skill. Similarly, there are no definite age requirements, although younger patients, especially those under the age of 25, should have more conservative treatment plans. As part of this planning, such patients are encouraged to use medical treatment to delay or partially reverse the progression of MPB. In addition, surgeons should leave enough hair in the safe donor area to permit at least one future surgery in the event of unexpected areas of hair loss.
With respect to gender, it is worth mentioning again that women are more often than generally thought, excellent candidates for hair restoration surgery, despite the strong disagreement of a few surgeons. In an effort to discern the consensus opinion, the authors informally polled a group of leading experts in the field. From among this group, a majority (13 out of 22) felt that more than 50% of women had enough donor hair to permit at least one transplant.9 In the authors’ opinion, the percentage is even higher provided that the patient’s expectations are commensurate with what is realistically possible given their donor/recipient ratio and hair characteristics. A strategically planned surgery, with a focus on transplanting the frontal zone and part-line, usually produces a cosmetically significant improvement, and leaves female patients very satisfied (Fig. 256-11).