Skin Flaps for Extensive Soft Tissue and Skin Resection
Jorge I. de la Torre
Luis O. Vásconez
Reconstruction following mastectomy was initially described for soft tissue coverage of the chest wall defect. During the 1940s, Meier described techniques to reconstruct the chest wall with local cutaneous flaps. Refinement of the reconstructive techniques and the implementation of multistaged procedures followed. Over the subsequent 60 years, chest wall and breast reconstruction has undergone tremendous change with regard to the variety and complexity of flaps employed to maximize efficacy and aesthetics.
Currently, chest wall defects in breast cancer patients can be divided into two sub-categories—those defects that are secondary to surgical resection of the tumor and those changes that occur later as a result of radiation therapy. Before considering any option for chest wall or breast reconstruction, it is important to understand the extent to which the soft tissue is affected.
The local skin flaps are indicated when skin coverage is required for coverage of extensive resection of the skin of the chest wall or to facilitate delayed reconstruction with an implant. It is particularly well suited in patients who have a skin deficit and who are not candidates for autologous breast reconstruction. This flap can be harvested and inset very simply and in a single stage. The thoracoepigastric flap can be combined with breast reconstruction by using an expander/implant. The donor site morbidity is limited to an area along the inframammary fold, which can be hidden within the inframammary fold and under the bra. It can be particularly useful when the patient does have excess skin in the upper abdominal region. Typically, healthy patients, with few comorbidities, are candidates for more extensive breast reconstructive options. Currently, the latissimus dorsi myocutaneous flap, with an implant or one of the variants of the rectus abdominus flaps, is preferable to local skin flaps as it offers soft tissue coverage for the chest wall and soft tissue to facilitate recreation of the breast mound. Local skin, soft tissue flaps are not indicated for patients who are candidates for immediate reconstruction.
Patients who have had prior surgical incisions in the upper abdomen may not be candidates for the medially based thoracoepigastric flap. If the scars traverse the planned flap, perfusion to the distal segment will be compromised and can result in flap loss. Similarly, patients who have undergone prior radiation therapy affecting the intended flap have a higher risk of poor perfusion and flap necrosis. In these situations, alternate local flap options would include the delayed deltopectoral flap or the contralateral upper rectus abdominus myocutaneous flap.
Preoperatively, the quality of the remaining tissue and the amount of skin and soft tissue required must be considered in flap selection and design. The actual markings and measurements should be conducted with the patient in an upright position. The location of the inframammary fold is delineated on both the affected and contralateral side for comparison.
The thoracoepigastric flap is designed with either medially based or laterally based pedicles. These local skin flaps do not have a discrete vascular pedicle and depend on the distribution of the angiosome for blood supply. Therefore, it is critical to maintain the appropriate width to length ratio of 1 to 3. The width of the flap is limited by the amount of upper abdominal skin that can be mobilized to permit primary closure of the donor site.
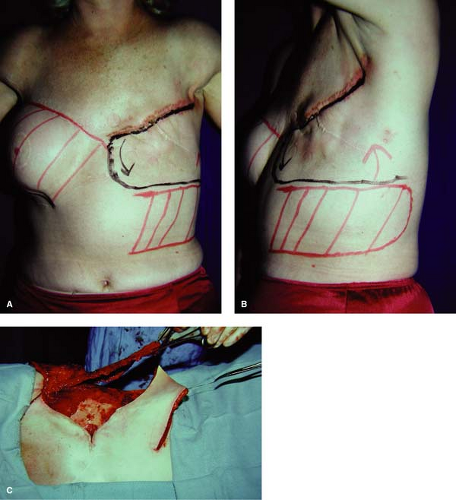
The medially based flap is designed as a horizontal flap extending laterally to the midaxillary line. (See Fig. 22.1A and B—preoperative marking of the flap is outlined in red on the patient’s left side. The red area on the patient’s right side indicates a prior thoracoepigastric flap for reconstruction of a previous contralateral mastectomy.) If a longer flap is required, the flap should be delayed; incising around the planned flap and elevating the edges but leaving it in place for 2 weeks before mobilizing and insetting it.
The laterally based flap is designed as an oblique flap extending inferiorly and medially, permitting rotation without excessive kinking of the rotation point of the pedicle. It is based on the skin perforators from the external oblique muscle. The more of these perforators that are captured, the more robust the blood supply to the distal flap. Unfortunately, it may limit the length of the flap and the degree of rotation. It can be difficult to primarily close the donor defect by mobilizing the inferior skin and soft tissue; skin grafts are often used to close the remaining donor defect.
Relevant Anatomy
Positioning
Under general anesthesia, the patient is positioned in the supine position, with a bump or slight elevation of the surgical side. Local anesthesia (0.5% lidocaine with epinephrine) is injected along the planned incision site.
Steps of the Procedure
Elevation of Flaps
The flap is elevated from lateral to medial in a plane deep to the fascia (see Fig. 22.1C to indicate the extent of elevation obtained with the thoracoepigastric flap). Dissection proceeds medially to the lateral border of the rectus sheath, preserving the perforators from the rectus muscle to the skin paddle. As the flap is elevated medially, additional perforators from the intercostal vessels will be encountered and should be preserved if possible to augment perfusion of the flap.