Chapter 6
Skin and Photosensitivity
OVERVIEW
- Ultraviolet radiation is a recognised carcinogen and the paler someone’s skin the more susceptible they are to ‘sun-damage’.
- Genetically inherited disorders such as albinism and xeroderma pigmentosum leave the skin and eyes vulnerable to UV light.
- Photosensitive eruptions have a typical appearance on sun exposed sites and can occur in any skin type.
- Photoprotection with clothing and sunscreen is important for vulnerable individuals.
The term photosensitive is used to describe patients with cutaneous disorders that result from exposure to normal levels of ultraviolet (UV) light. Sun-exposed skin is predominately affected in acquired photosensitivity, particularly of the face, neck, dorsi of the arms/hands and lower legs. There is marked sparing of sun-protected sites, particularly the buttocks, behind the ears and under the chin, which can provide useful diagnostic clues.
Skin tolerance of UV light will depend on a number of factors including the intensity of UV light, skin type (Fitzpatrick skin types classified according to inherited levels of skin pigmentation), genetic disorders (sun-damage repair mechanisms may be defective), acquired allergic conditions and photosensitising medications.
Taking a thorough history of sun exposure and reactions to it is important in patients with suspected photosensitivity. Patients may not develop symptoms unless they are exposed to high intensity sunlight whereas others will be affected throughout the year with low intensity UV exposure. The time to onset of symptoms following UV exposure is an important part of the history as are the course of any skin eruption (frequency and duration) and whether any scarring or marks are left behind on the skin following the acute phase. Symptoms of itching, burning and even pain can be reported.
This chapter considers cutaneous disorders related to UV light; however, precancerous and cancerous skin lesions are discussed elsewhere (Chapters 21 and 22).
Ultraviolet radiation
UV A and B radiation penetrate the earth’s atmosphere and are known to play a role in sun-induced skin damage (Figure 6.1). UV intensity is greatest near the equator and at high altitudes. Environmental factors such as the season, time of day and reflective surfaces (water, snow and sand) can influence the intensity of UV light. There is evidence that holes in the ozone layer have led to pockets of high intensity UV.
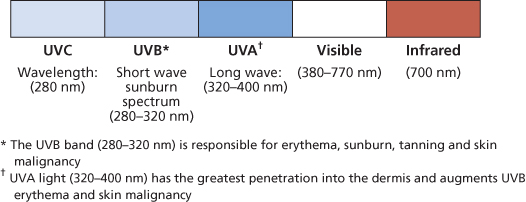
Figure 6.1 Light spectrum.
UVB has a short wavelength and varies according to the season. UVB levels are at their highest in the summer months and during the middle of the day. UVB is important in both sunburn and the development of skin cancer. UVA has a longer wavelength and is present all year round and throughout the day at fairly constant levels. UVA can pass through glass and is known to induce immediate and persistent pigment darkening, delayed tanning and skin ageing. There is increasing evidence that UVA also plays a role in skin cancer development.
UV light can cause immediate effects on the skin in the form of photosensitivity and sunburn, and long-term effects such as skin ageing (wrinkling and solar keratoses) and skin cancer.
Fitzpatrick skin type classification
Natural skin pigmentation is formed by melanin which is synthesised by melanocytes. The quantity of melanin in the skin determines its ability to withstand UV radiation. In healthy skin, the number of melanocytes remains constant; however, the amount of melanin they synthesise is genetically determined, leading to different levels of skin pigmentation. Fitzpatrick devised a classification based on skin type according to inherited pigmentation and the skin’s response to UV light. Patients with type I skin are likely to burn even if the UV intensity is low, whereas patients with type VI skin will not usually suffer sun-damage. An assessment of a patient’s skin type will help the physician determine the patient’s susceptibility to UV as well as in guiding certain therapies, such as phototherapy and laser treatments. Fitzpatrick skin type can be used to determine the starting doses and increments of UVA/TL-01 during phototherapy.
- Type I (very fair skin/freckled/red hair)—always burns, never tans.
- Type II (fair skin)—usually burns, tans eventually.
- Type III (fair to olive skin)—occasionally burns, tans easily.
- Type IV (brown skin)—rarely burns, tans easily.
- Type V (dark brown skin)—very rarely burns, tans easily.
- Type VI (black skin)—never burns, tans easily.
Genetic disorders causing photosensitivity
Oculocutaneous albinism
Genetic mutations that control melanin synthesis, distribution and degradation result in a group of inherited disorders that lead to loss of skin/hair/eye pigment. Oculocutaneous albinism is an autosomal recessive condition characterised by little or absent melanin pigment at birth (Figure 6.2). Oculocutaneous albinism affects skin, hair and ocular pigmentation, resulting in sun-induced skin changes, photophobia, nystagmus and reduced visual acuity.

Figure 6.2 Oculocutaneous albinism.
Oculocutaneous albinism is traditionally classified into two groups—tyrosinase positive or negative—depending on whether the enzyme is absent or dysfunctional; however, there are numerous subtypes depending on the specific genetic mutation.
Affected individuals should be assessed in the neonatal period by a dermatologist and an ophthalmologist. The family may wish to consult a geneticist. A sunscreen blocking UVA and UVB light (broad-spectrum) should be applied to the skin on a daily basis and reapplied as necessary. Protective clothing and sun avoidance behaviour should be encouraged. Skin checks for any evidence of sun-damage or skin cancer should be undertaken regularly. Corrective spectacles may improve visual acuity.
Other genetic conditions associated with loss of skin pigment include piebaldism, phenylketonuria, tuberous sclerosis and Waardenburg and Apert syndromes.
Xeroderma pigmentosum
A group of autosomal recessive conditions result from deficient cutaneous nucleotide excision repair mechanisms which lead to defective DNA repair. Patients have accelerated UV-associated changes in the skin characterised by photosensitivity, pigmentary changes, premature skin ageing and tumour formation during the first decade of life. Ocular damage also results from photosensitivity. The diagnosis is usually apparent between the ages of 1 and 2 years. Early signs of the disorder include excessive persistent sunburn, freckling, mottled pigmentation (poikiloderma), telangiectasia and skin thinning. Later, patients develop multiple skin cancers including melanoma and squamous and basal cell carcinomas. Early ocular signs include photosensitivity and conjunctivitis and later fibrosis and malignancies. Patients may also suffer from neurological problems including deafness and mental retardation. Strict sun avoidance (skin and eyes) is paramount for these patients. Photoprotective clothing, broad-rimmed hats, sunglasses and physical sunscreen should be regularly used. Oral retinoids can help reduce the rate and number of skin cancers. The use of imiquimod and 5-fluorouricil to treat the sun-damaged skin has been shown to help reduce skin tumour development. In the future, it may be possible to correct DNA damage by delivering topical liposomal DNA repair enzymes. Ultimately, gene therapy may be utilised to manage this disease.
Metabolic disorders of photosensitivity
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








