Chapter 2
Psoriasis
OVERVIEW
- Psoriasis is a chronic inflammatory condition of the skin thought to be autoimmune mediated.
- Psoriasis has been shown to be an independent risk factor for cardiovascular disease.
- Specific biological therapies are transforming the management of psoriasis and psoriatic arthropathy.
- Clinical presentations can be variable from chronic stable plaques, to pustules on the hands and feet, to unstable erythroderma.
Psoriasis is now considered to be a genetically determined inflammatory systemic autoimmune disease. It is characterised by plaques of diseased skin often at sites of minor trauma (elbows/knees), which occur next to areas of clear ‘normal’ skin. Plaques of psoriasis are clinically well-demarcated and are erythematous (dilated dermal blood vessels) with white surface scale (rapid keratinocyte proliferation). Psoriasis not only affects the skin but can also lead to seronegative arthritis in approximately 8–30% of patients. However, there is an increasing body of evidence that psoriasis is also associated with other important comorbidities such as type 2 diabetes (1.4-fold increased risk), cardiovascular disease, metabolic syndrome, obesity, depression and reduced quality of life.
The pathogenesis of psoriasis is complex; nonetheless, it is largely accepted that the disease is mediated by the dysregulation of T-helper lymphocytes (Th1/Th17). The development of psoriasis is multifactorial, with multiple potential susceptibility factors in a genetically at-risk individual. This combination of susceptibility factors and genetic predisposition results in an interactive web of immune cells/chemical cytokines impacting on skin cells and leading to disease. Increased understanding of these complex cellular changes has led to the introduction of multiple targeted biological therapies that are now used to manage severe psoriasis and psoriatic arthritis (PA).
Globally 1–2% of the population is affected by psoriasis (125 million people in UK/USA/Japan alone). A child who has one parent with psoriasis has a 1 in 4 chance of developing the disease. If one identical twin has psoriasis, there is a 70% chance that the other will also be affected; however, only a 20% chance exists in dizygotic twins. Linkage and genome-wide association studies have started identifying some of the important susceptibility factors leading to the inheritance of psoriasis and psoriatic arthropathy. The first and arguably one of the most important psoriasis susceptibility loci identified is the so-called PSORS1 found on chromosome 6p21.3. This region of the chromosome contains several genes which may be important in the inheritance of psoriasis including HLA-C (human leukocyte antigen-C), CCHCR1 (coiled-coil α-helical rod protein 1) and CDSN (corneodesmosin). Subsequently, multiple susceptibility loci on several chromosomes have now been identified including 1q21, 3q21, 4q, 7p, 8, 11, 16q, 17q, and 20p. Recently, a loss of function mutation in a gene encoding an IL-36 receptor antagonist has been shown to be associated with the development of palmo-plantar pustular psoriasis.
Plaques of psoriasis are highly infiltrated with CD3+ T-cells and CD11c+ dendritic cells which produce pro-inflammatory cytokines including tumour necrosis factor alpha (TNF-α), interferon gamma (INF-γ) and interleukin 17 (IL-17), IL-22/23/12/1β, which activate keratinocytes and other skin cells. Keratinocytes are the skin cells that predominate in the epidermis; they grow from the basal layer and slowly migrate to the surface (Figures 2.1 and 2.2). In normal skin, this process of cell turnover takes about 23 days; however, in psoriasis cell turnover is rapidly accelerated, taking only 3–5 days for cells to reach the surface and accumulate in large numbers (hyperkeratosis). Keratinocytes normally lose their nuclei as they move to the skin surface; however, in psoriasis they move so quickly that the cells retain their nuclei throughout the epidermis, seen as parakeratosis histologically. This rapid turnover and failure of proper maturation result in defective keratinocytes, which are poorly adherent and easily scraped off (‘Auspitz sign’) revealing underlying dilated blood vessels.
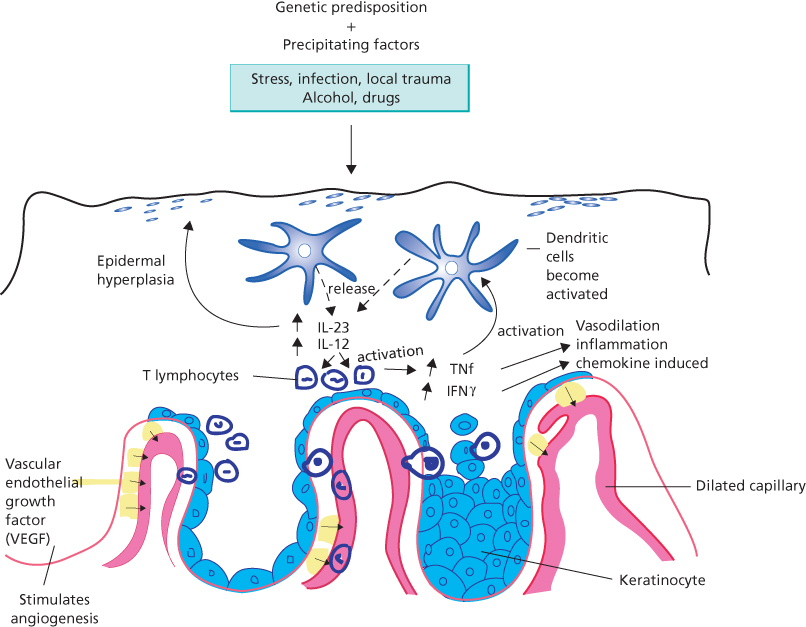
Figure 2.1 Pathophysiological mechanisms involved in the development of psoriasis.
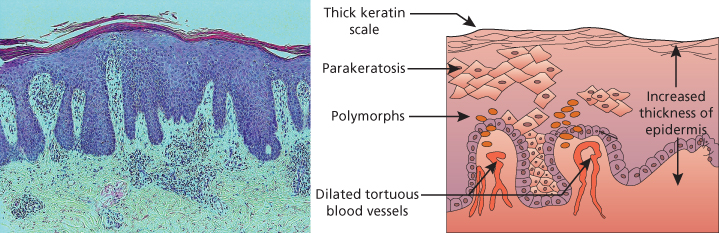
Figure 2.2 (diagram/histology composite) Increased epidermal proliferation.
In addition, inflammatory polymorphs infiltrating the epidermis lead to swelling (oedema), inflammation and erythema. These inflammatory cells may occur in such large numbers that they form collections of sterile pustules at the skin surface. These are most commonly seen in palmo-plantar pustulosis, a variant of psoriasis affecting the palms and soles.
The cellular abnormalities in the skin of patients with psoriasis can occur in the nails, and many patients will therefore have additional nail changes.
Psoriatic nail dystrophy is characterised by
- onycholysis (lifting of the nail plate off the nail bed) due to abnormal cell adhesion; this usually manifests as a white or salmon patch on the nail plate (Figure 2.3 pitting and onycholysis of nails);
- subungal hyperkeratosis (accumulation of chalky looking material under the nail) due to excessive proliferation of the nail bed that can ultimately lead to onycholysis;
- pitting (very small depressions in the nail plate) which result from parakeratotic (nucleated) cells being lost from the nail surface;
- Beau’s lines (transverse lines on the nail plate) due to intermittent inflammation of the nail bed leading to transient arrest in nail growth;
- splinter haemorrhages (which clinically look like minute longitudinal black lines) due to leakage of blood from dilated tortuous capillaries.

Figure 2.3 Pitting and onycholysis of the nails.
Clinical appearance
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








