Secondary Reconstruction: Reduction Mammoplasty, Mastopexy, and Breast Augmentation
Nolan Karp
When choosing a method of breast reconstruction, it is often possible to select a technique that will closely match the contralateral breast in size and shape. Other times, the method chosen will require alteration of the contralateral breast to achieve symmetry. Some patients may even request surgery on the normal breast for either cosmetic or functional reasons. In patients with very large breasts, mammograms following breast reduction surgery will be easier to interpret. The timing of the symmetry procedure and the technique chosen should not interfere with either the patient’s cancer treatment or future monitoring of the contralateral breast.
Available techniques include breast reduction, mastopexy, augmentation, or a combination of these techniques. Not only is the selection of technique important but also its timing is critical to achieving the best cosmetic results.
Breast Reduction
Breast reduction is most often required when patients have breasts larger than a C cup. It is extremely difficult to achieve symmetry in these large, usually ptotic, breasts by any reconstructive technique. When tissue expansion is chosen, the degree of expansion required would often result in extreme thinning of the overlying skin and sufficient ptosis is usually impossible to attain. In the ptotic patient, autologous tissue reconstructive techniques are preferable, assuming there is adequate donor site tissue available. Breast reduction is best performed as a secondary procedure after flap reconstruction or at the time of permanent implant placement after tissue expander reconstruction. Breast reduction techniques all result in some internal breast scarring postoperatively. These mammographic changes are well understood and do not interfere
with interpretation. When breast reduction is performed, it is important to choose a technique that has a low risk for fat necrosis. When fat necrosis occurs within the breast, it can pose diagnostic problems, usually requiring biopsy. Liposuction is avoided in breast reduction due to potential distortion of the internal architecture of the breast, which may make future mammographic interpretation more difficult. This is particularly important in the group of patients who have had cancer in the other breast.
with interpretation. When breast reduction is performed, it is important to choose a technique that has a low risk for fat necrosis. When fat necrosis occurs within the breast, it can pose diagnostic problems, usually requiring biopsy. Liposuction is avoided in breast reduction due to potential distortion of the internal architecture of the breast, which may make future mammographic interpretation more difficult. This is particularly important in the group of patients who have had cancer in the other breast.
Mastopexy
Mastopexy is often required when significant ptosis exists in the contralateral breast since breast symmetry is the goal of reconstruction. Mastopexy, similar to breast reduction, is best performed as a secondary procedure. Available mastopexy procedures either reshape the skin or internally reshape the breast mound. Internal architectural distortion should be minimized in these patients if possible. It is best to avoid mastopexy techniques that extensively reshape the breast gland. In general, long-term results have been very similar for both internal reshaping procedures and dermal procedures.
Breast Augmentation
Usually breast augmentation is useful in small-breasted women who have undergone implant reconstruction and need additional upper breast fullness in the normal breast to achieve symmetry. Augmentation will always interfere with future mammograms, making it difficult to visualize all of the breast tissue when an underlying implant is present. When the implant is small, placed subpectorally, and remains soft, the degree of mammographic distortion is minimal. The use of saline implants placed underneath the pectoralis muscle has significantly reduced the incidence of capsular contracture and subsequent firmness of the breast. When augmentation is being considered, carefully documented consultations with the oncologic surgeon and mammographer are important. Augmentation is best performed at the time of final implant placement to achieve best symmetry.
When symmetry procedures are necessary, all issues must be discussed with the patient and other treating physicians before deciding on the method of breast reconstruction. The need for contralateral breast surgery may alter the choice of technique chosen for the breast reconstruction.
Breast Reduction
The vast majority of the breast reductions performed for symmetry after contralateral breast reconstruction can be done with the short scar vertical technique. Occasionally, in patients with very large or very ptotic breasts Wise-pattern or anchor-type scar (inverted-T) reductions are required.
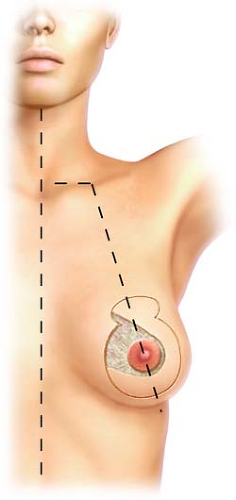
Our method of short scar breast reduction is based in part on the technique described by Hall-Findlay with some modifications as previously described by the author. Briefly, the patient is marked in the standing position, with the new nipple position marked at the level of the inframammary fold, matching the location of the nipple of the reconstructed breast. The outline of the future nipple–areolar complex is designed by utilizing a mosque pattern, and the medial and lateral extent of resection are marked with a breast displacement technique. These lines are curved gently and connected to a point 2 to 4 cm above the inframammary fold, depending on the size of the breast. The medially based pedicle is designed from 6 to 10 cm in width, again depending on the size of the breast, with part of the pedicle within the mosque pattern. The nipple–areolar circumference is usually marked with a 42-mm diameter cookie cutter (Fig. 32.1).
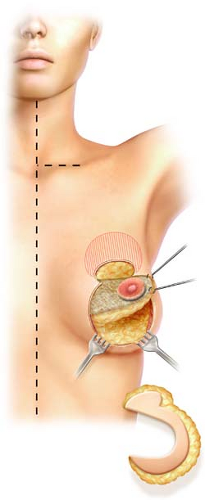
The operation begins by deepithelializing the pedicle, followed by elevation of a thin inferior flap to the chest wall fascia and subsequent resection of the inferior pole of the
breast from just deep to the subcutaneous plane to the level of the pectoralis fascia. Breast tissue is resected laterally and medially according to the desired breast size and to allow rotation of the medially based dermoglandular pedicle. Care is taken to leave the inferior pole “empty” while leaving the superior pole largely intact. This is especially important when matching an implant reconstruction on the other side (Fig. 32.2).
breast from just deep to the subcutaneous plane to the level of the pectoralis fascia. Breast tissue is resected laterally and medially according to the desired breast size and to allow rotation of the medially based dermoglandular pedicle. Care is taken to leave the inferior pole “empty” while leaving the superior pole largely intact. This is especially important when matching an implant reconstruction on the other side (Fig. 32.2).
 Figure 32.3 Pedicle in position and pillar sutures being placed. The entire bottom of the breast is empty. |
After insetting the areola, the parenchyma of the medial pedicle is sutured to the tissue of the lateral “pillar” (Fig. 32.3). These pillar sutures are critical for setting the ultimate breast shape. The patient is then placed in a sitting position, and the breasts are assessed for size, shape, and symmetry. The patient is returned to the supine position and adjustments to the pillar sutures and additional resection performed as necessary. At this point, liposuction may be used as an adjunctive contouring technique; it is especially useful for removal of axillary breast tissue in obese patients. Hemostasis is then obtained and closed suction drains are placed. Finally, the skin incisions are closed in layers. The patients are usually sent home the same day without any external breast support.
Mastopexy
The type of mastopexy procedure performed is dictated by the nature of the deformity. Patients with minor degrees of ptosis are frequently treated with periareolar (concentric) mastopexy procedures. Periareolar mastopexy is also often the procedure of choice when breast augmentation is combined with mastopexy. As the volume of the breast is increased by the implant, the need and degree of the mastopexy procedure becomes less. As the ptosis worsens, vertical mastopexy with a lollipop-type incision or conventional mastopexy with inverted-T incision might be indicated.
Periareolar (Concentric) Mastopexy
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree