Abstract
Pain or nerve dysfunction following craniofacial trauma or surgery is often treated with medical regimes or close observation. Facial pain or dysfunction lasting longer than 6 months to 1 year can be defined as chronic facial pain. In traumatic situations, it is often the nerve foramina in the craniofacial skeleton that are areas of weakness. This often leads to nerve injury in craniofacial trauma. Dentoalveolar surgery and orthognathic surgery encompass many of the cases of injury to the inferior alveolar and lingual nerves. Appropriate surgical history and physical examination are paramount in the proper management and diagnosis of craniofacial nerve dysfunction. Surgical management is often a fine balance between managing pain and patient functional expectations. Often the goal of surgical treatment is anesthesia over dysesthesia. The techniques and principles of nerve repair are similar to those of peripheral nerve repair throughout the rest of the body. Primary tension-free nerve repair is the gold standard. There is no consensus agreement on the use of nerve grafts or conduits for secondary nerve repair in the craniofacial region. Outcomes of repair should be supplemented in a multidisciplinary fashion utilizing appropriate neuromodulating medications as well as neurosensory rehabilitation.
Keywords
craniofacial, nerve repair, facial trauma, BSSO, orthognathic surgery, lingual nerve, inferior alveolar nerve, dentoalveolar surgery
Background
Injury to the peripheral nerve branches of the craniofacial region can arise from a variety of surgical procedures. Common elective procedures such as dentoalveolar surgery, dental implant placement, endodontic treatment, orthognathic surgery, and facial esthetic surgery can result in injury to branches of the trigeminal nerve. Often overlooked in the evaluation of traumatic injury to the craniofacial skeleton or the surrounding soft tissue, is injury to the peripheral branches of the trigeminal nerve. Nerve injuries in facial trauma can be the result of direct injury to the area, traction or avulsion during repair, or aberrant scar/bone formation. Injuries can often lead to frustration and anger on the part of the patient, possibly leading to litigation.
By definition, if postoperative pain persists for greater than 6 months, the diagnosis of chronic facial pain is made. Most patients with postoperative pain can be managed nonoperatively, however those patients who qualify for surgical treatment should be managed in an algorithmic manner. In a retrospective review by Susarla et al., patient satisfaction following trigeminal nerve repair was strongly correlated with improvement in neurosensory examination. Practitioners operating on the craniofacial skeleton should be familiar with the diagnosis and treatment of acute and chronic postoperative pain and relay the appropriate goals and expectations from both nonsurgical and surgical limbs. Persistent postoperative pain in the trauma setting may be multifactorial, particularly in the patient with a history of complex craniofacial injuries. Any attempt to treat the pain must be preceded by a thorough evaluation of the possible causative agents of the patient’s problems. Malunion, nonunion, malocclusion, internal derangement of the TMJ and functional shortening of traumatized musculature can all lead to ongoing postoperative pain. The identification of a nerve injury as the causative factor may require the use of diagnostic nerve blocks, imaging and detailed examination, combined with a knowledge of the basic physiology of peripheral nerve injuries.
Trigeminal Anatomy
Due to the high volume of dentoalveolar surgery in the mandible, the inferior alveolar and lingual branches of the third trigeminal nerve are the most commonly injured. However, the incidence of injury to other branches of the trigeminal nerve in trauma patients is probably underreported. Manson et al. reported that a third of their patients with isolated traumatic Le Fort fractures complained of chronic facial pain. In addition, most of these patients showed some improvement after surgical intervention. Unfortunately, the true incidence and evaluation of chronic facial pain in the trauma patient is often difficult to study due to the fact that many of these patients are lost to follow-up.
The most common sensory nerves encountered in craniofacial trauma are the supraorbital/supratrochlear, infraorbital, zygomaticofacial, inferior alveolar, and the lingual nerves.
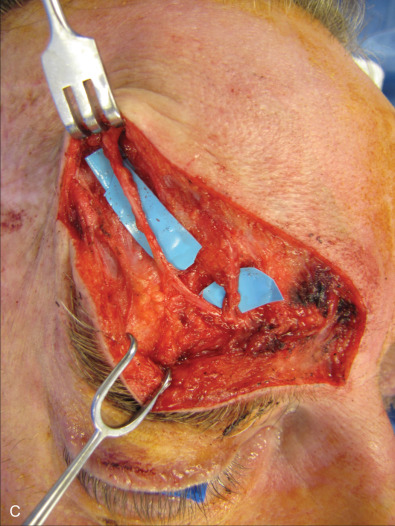
The three branches of the trigeminal nerve, ophthalmic, maxillary, and mandibular nerves, exit the skull through separate foramina: superior orbital fissure, foramen rotundum, and foramen ovale respectively ( Fig. 3.16.1 ). The largest branch of the ophthalmic nerve is the frontal branch. This branch will divide within the orbit to give the terminal branches of the supraorbital and supratrochlear nerves. These nerves give sensation to the upper eyelid as well as the central or lateral forehead. Classically, these nerves can be released from their bony foramina or notch to gain release of the forehead soft tissue to facilitate access to the upper facial skeleton via a coronal approach ( Fig. 3.16.2 ).
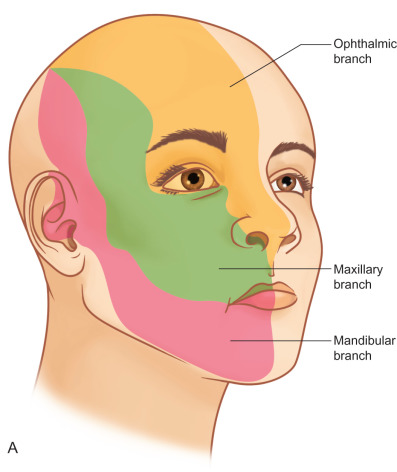
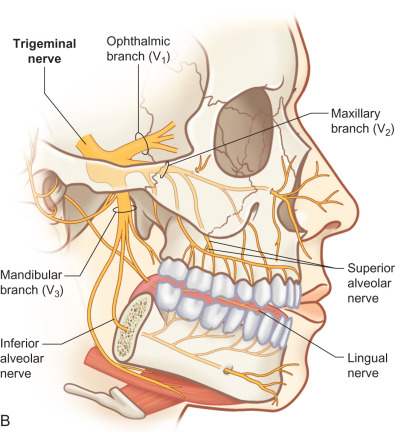



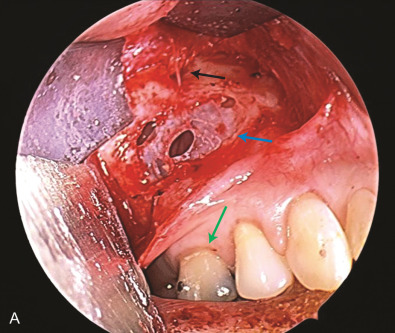
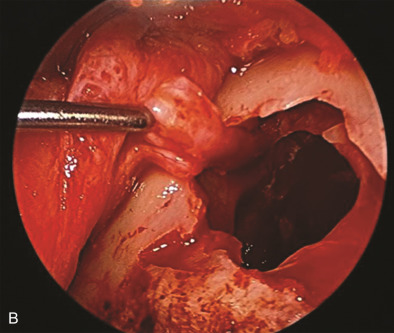
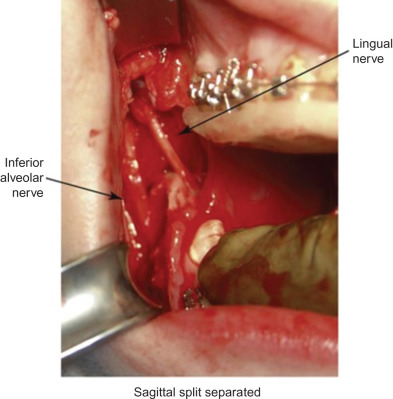
The maxillary division carries sensory information from the lower eyelid, cheek, upper lip, upper teeth, and associated mucosa. The zygomatic nerve gives its terminal branch as the zygomaticofacial nerve that supplies sensation to the lateral cheek and portions of the forehead. The terminal branch of the maxillary nerve exits the facial skeleton as the infraorbital nerve. This nerve is encountered regularly in midface injuries as well as orbital floor fractures ( Fig. 3.16.3 ). The mandibular division is the largest branch of the trigeminal nerve. Before the mandibular nerve enters the medial mandible at the lingula, it will bifurcate and the lingual branch will course within the soft tissue of the floor of the mouth, where it will be in intimate association with the submandibular duct. The terminal branch of the mandibular nerve will enter the medial mandible within the inferior alveolar canal and exit at the mental foramen to give sensation to the mandibular dentition, mucosa, and lower lip. Both of these nerves can be encountered in mandibular fractures as well as soft tissue injuries to the submandibular region ( Fig. 3.16.4 ).
Peripheral Nerve Injury and Histopathology
Peripheral nerve injuries were historically first classified by Sir Herbert Seddon in 1943. This was based on gross and histological changes rather than the actual mechanism of injury. He initially described three types of nerve injuries.
Neurapraxia is a discrete area of local conduction block along the course of the nerve. The nerve is in continuity and there is no Wallerian degeneration. Recovery is generally expected within 12 weeks. There will be no Tinel sign at the site of the lesion. This injury is associated with localized pressure such as a tourniquet or a retractor. Axonotmesis indicates direct axonal damage, and finally neurotmesis would involve transection of the peripheral nerve. Wallerian degeneration occurs in both axonotmesis as well as neurotmesis. The degeneration occurs distal to the site of injury with recovery in axonotmesis but not in neurotmesis. Sunderland expanded on the initial work of Seddon and emphasized five degrees of nerve injury. First- (neuropraxia) and second- (axonotmesis) degree injuries can recover spontaneously, whereas fourth- and fifth-degree nerve injuries are not expected to recover spontaneously ( Table 3.16.1 ).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree