Abstract
Fractures of the nasoethmoid region with displacement of the medial canthal-bearing segment of the medial orbital wall remain some of the most difficult surgical repairs in facial trauma. Nasoethmoid injuries are often misdiagnosed or inadequately treated because of the complex anatomy and technical challenges associated with this region. This results in secondary nasoethmoid deformity. While the avoidance of delayed nasoethmoid deformities by optimal primary management remains the best treatment of secondary nasoethmoid orbital fractures, patients continue to present in a delayed fashion somewhat commonly. The treatment of secondary nasoethmoid fractures is more complicated due to posttraumatic soft tissue scarring, chronic contour irregularities, and bony resorption. Patients may present with a variety of orbital, nasal, and lacrimal signs and symptoms of inadequate primary repair. Keys to the repair of secondary nasoethmoid fractures include: careful anchoring of the medial canthal tendon to the central bone fragment, meticulous debulking, and redraping of the soft tissue of the naso-orbital valley, accurate transnasal wire and soft tissue buttress placement, and reconstruction of nasal and internal orbital deformities. The chapter presents the senior author’s approach to secondary nasoethmoid fracture repair, including case examples that illustrate the surgical management of these complex deformities.
Keywords
secondary nasoethmoid fracture, posttraumatic deformity, maxillofacial trauma reconstruction
Background
High-energy midfacial trauma commonly results in naso-orbito-ethmoid (NOE) fractures, which present some of the greatest diagnostic and therapeutic challenges in facial trauma reconstruction. Fractures of the nasoethmoid region are defined as a midface fracture resulting in lateral displacement of the medial canthal-bearing segment of the medial orbital wall. These fractures may be isolated but frequently occur as part of more extensive “panfacial” fractures. The degree of comminution is proportional to the amount of trauma to the nasoethmoid skeleton, which also determines the degree of difficulty for reduction and primary repair. Nasoethmoid injuries are often misdiagnosed and inadequately treated because of the complex anatomy and technical challenges associated with this region. Failed management of nasoethmoid fractures in the primary setting can result in functional and cosmetic deformities that are difficult to correct secondarily. The pitfalls leading to secondary deformities are summarized in Box 3.5.1 .
Missed diagnosis
Inadequate operative exposure
Poor reduction and stabilization of bone fragments
Reduction plating placement in the medical canthal region
Undetected loss of normal nasal contours
Missed orbital defects
Failure to adequately reduce soft tissues in the naso-orbital valley
While nasoethmoid fracture management presents a challenge to even experienced surgeons, the best treatment of secondary nasoethmoid deformity remains its avoidance by the early diagnosis and appropriate treatment of the primary injury. Soft tissue swelling may obscure the severity of nasoethmoid fractures, so a high degree of suspicion is required to diagnose their initial presentation. The missed diagnosis and failed surgical treatment of nasoethmoid fractures can be best avoided with detailed knowledge of the surgical anatomy of this region, a thorough understand of the clinical presentation and management of such fractures, and a high degree of clinical suspicion. Once diagnosed, the treatment of nasoethmoid fractures remains one of the most difficult surgical repairs in facial trauma. It therefore remains somewhat common that patients present in a delayed fashion for both primary repair and secondary surgical revision ( Fig. 3.5.1 ).
The treatment of secondary nasoethmoid fractures is more complicated and often results in inferior outcomes compared to optimal primary management. Posttraumatic tissue scarring and contour irregularities add complexity to delayed repair. The surgeon must widely expose the deformity, recreate the injury with selective osteotomies, and then reduce the tissue to its premorbid state with rigid bony fixation and soft tissue stabilization. The possibility of lost bone stock due to resorption of comminuted fragments increases the need for autogenous bone grafts, but this is rarely needed in the medial orbital wall. Soft tissue scarring and contracture result in the loss of elasticity and limit redraping the soft tissues with an optimal recreation of the subtle soft tissue contours that distinguish the nasoethmoid region. This chapter presents the senior author’s approach to secondary nasoethmoid fracture repair, including case examples that illustrate the surgical management of these complex deformities ( Fig. 3.5.2 ).
Surgical Anatomy
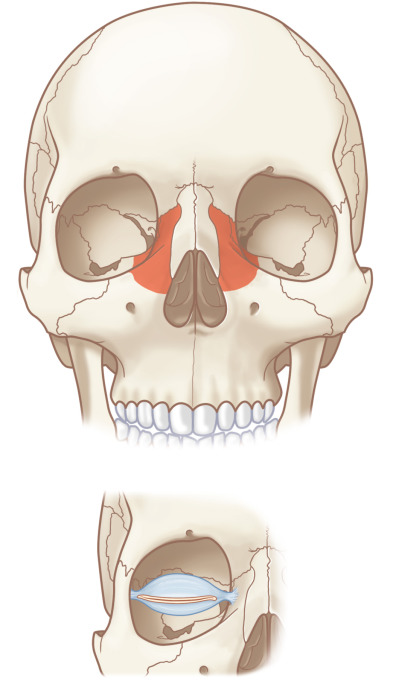
Nasoethmoid Region ( Fig. 3.5.3 )
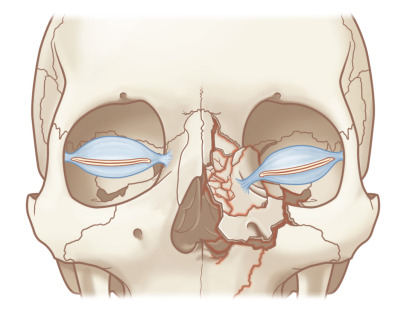
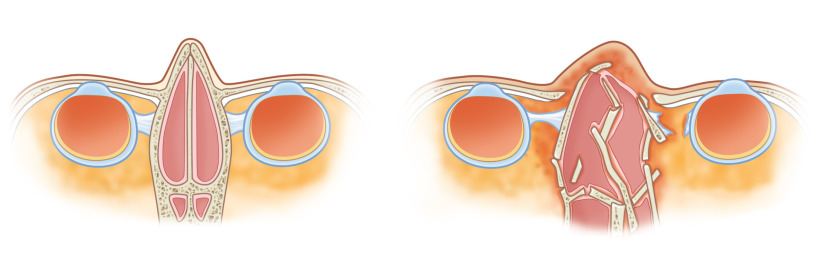
The nasoethmoid skeleton consists of the confluence of orbital, nasal, maxillary, and cranial bones. Multiple facial buttresses support the nasoethmoid region, including the frontal process of the maxilla vertically and the supraorbital and infraorbital rims horizontally. Together these buttresses create a relatively stable anterior framework. Weakness exists posteriorly in the form of the thinner lacrimal and ethmoid bones of the internal medial orbital walls, which are prone to blow-out fracture and comminution. The inadequate reduction of displaced medial orbital rim and wall fragments results in a loss of definition of the naso-orbital valley. This may require wide scar release during delayed or revision surgery while taking care to avoid iatrogenic injury to the medial canthal tendon. Soft tissue buttressing may then be required for recontouring in secondary nasoethmoid fracture repair ( Fig. 3.5.4 ).

Interorbital Space
Between the two medial orbital walls and below the floor of the anterior cranial fossa lies the interorbital space, which consists of two ethmoidal labyrinths divided by the perpendicular plate of the ethmoid and nasal septum. Anterior to this region are the nasal bones, and care must be taken to avoid confusing fractures of these bones with those of the nasoethmoid region. The cribriform plate is found in the posterior roof of the interorbital space, which explains the occasional occurrence of persistent cerebrospinal fluid rhinorrhea or dysosmia with delayed nasoethmoid fractures. The interorbital space is both vulnerable to fracture from central midface trauma and adds complexity to the accurate diagnosis of nasoethmoid fractures, which may contribute to delays in presentation.
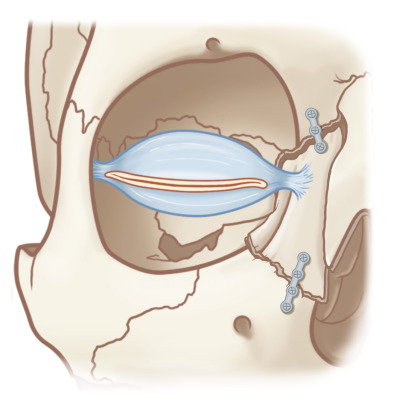
Medial Canthal Tendon and Central Bone Fragment ( Fig. 3.5.5 )
The single most important region of the medial orbital rim to optimal surgical repair of complex nasoethmoid fractures in both the acute and delayed setting is the “central bone fragment,” into which the medial canthal tendon inserts. There are three limbs of the medial canthal tendon. The anterior limb is distributed over the frontal process of the maxilla onto the posterolateral nasal bones. The superior limb inserts at the junction of the frontal process of the maxilla and the internal angular process of the frontal bone. The thin posterior portion inserts behind the lacrimal sac into the posterior portion of the lacrimal fossa. Nasoethmoid orbital fracture lines may extend through the frontal process of the maxilla, the medial orbital wall, inferior orbital rim, and lateral nasal bones, resulting in a mobile central medial orbital rim fragment. This can result in a mobile canthal-bearing segment, which can compromise the integrity of eyelid support ligaments and the contour of the palpebral fissure. The degree of displacement is often proportional to the extent of comminution, which varies greatly between injuries. An intimate knowledge of these anatomical relationships is essential to appropriately manage secondary nasoethmoid fractures, whose premorbid anatomy must be reapproximated despite being altered at the time of presentation ( Fig. 3.5.6 ).
Clinical Presentation
Patient History
The delayed presentation of nasoethmoid fractures may occur after missed diagnosis or inadequate treatment of an acute injury, so the presentation may share certain elements of the original trauma setting with some important distinctions. The astute clinician should be mindful of the varied manner in which delayed nasoethmoid fractures may present in order to avoid repeating its misdiagnosis or inadequate treatment. A recent history of blunt trauma to the central midface is the typical presentation of the acute nasoethmoid fracture, but initial injury sequelae may not prompt presentation for weeks to months. Ideally, details of the original mechanism of injury and initial surgery would be obtained prior to any remote operative intervention. Without adequate primary nasoethmoid fracture repair, patients present with a variety of deformities, which are summarized in Box 3.5.2 .
General
Soft tissue scarring and contraction
Chronic central midface pain
Nasal
Widened nasal bridge
Foreshortened nose
Lack of nasal tip support or projection
Saddle nose deformity
Orbital
Traumatic telecanthus
Canthal asymmetry
Enophthalmos
Vertical orbital dystopia
Persistent diplopia
Orbital rim step-off
Grossly enlarged orbit
Strabismus
Lacrimal dysfunction
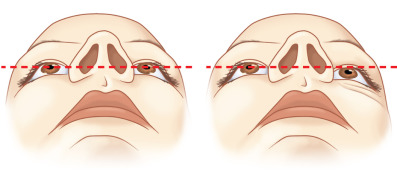
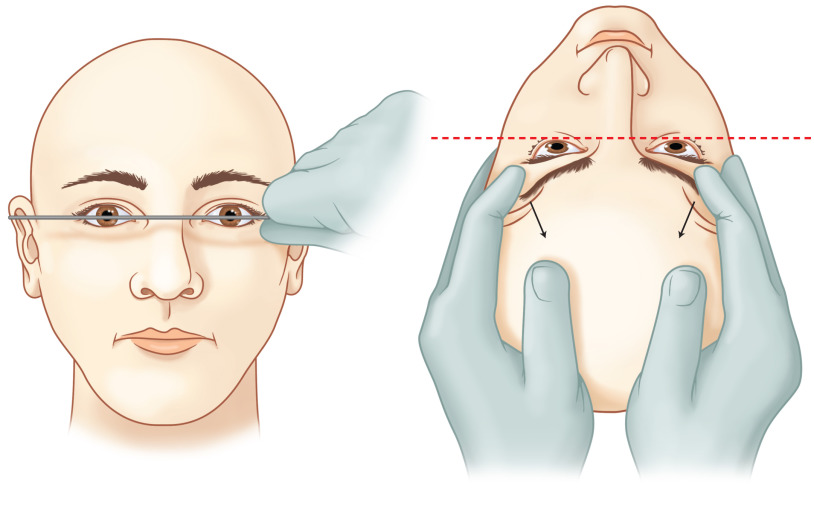
Physical Examination ( Fig. 3.5.7 )
Physical examination findings of medial orbital rim step-off, mobile medial orbital bone segments, a “telescoped” nasal radix, or telecanthus may be obscured by central midface scar tissue or chronic edema. Common orbital findings in the representation of patients with nasoethmoid fractures include: an asymmetric corneal light reflex, displaced and misshapen bony fragments creating step-offs, enophthalmos, or periorbital soft tissue scarring and contracture. Due to lost nasal and septal support, the nose may appear flat and foreshortened with a wide nasal dorsum and upturned tip. Nasal deformity as a result of healed nasal bone fractures must be distinguished from the nasoethmoid deformity. Lacrimal dysfunction from a traumatized nasolacrimal duct may manifest with epiphora. The physical exam findings may reflect displaced bone fragments ( Fig. 3.5.8 ).
Radiological Evaluation
A high-quality CT scan with no more than 1.5 mm thickness axial and coronal cuts confirms the diagnosis of secondary nasoethmoid fracture. Two-dimensional axial and coronal images provide a blueprint for the surgical plan, including planning the incision, use of bone grafts, location of osteotomies, and avoidance of adjacent structures. After cross-sectional imaging has been evaluated, three-dimensional reconstructions may be utilized to refine and improve the assessment. Care should be taken not to rely on 3-dimensional reconstructions in isolation to avoid underestimation of the details of the fracture . The surgeon should be mindful that abnormal bony and soft tissue densities from scarring or edema may be present and obfuscate anatomic boundaries in secondary nasoethmoid fractures. This may complicate the determination of the fracture pattern, degree of comminution, and displacement, which must be considered in the development of an adaptable surgical plan.
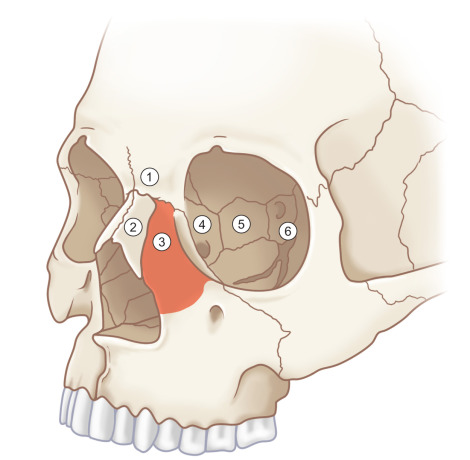
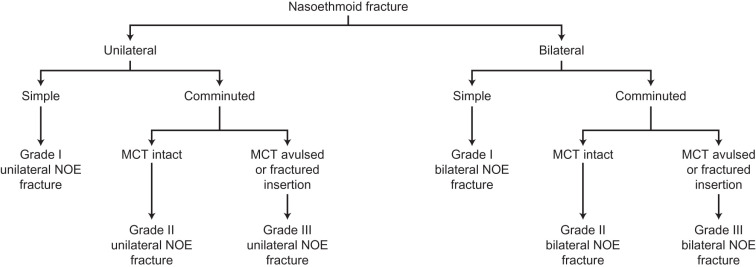
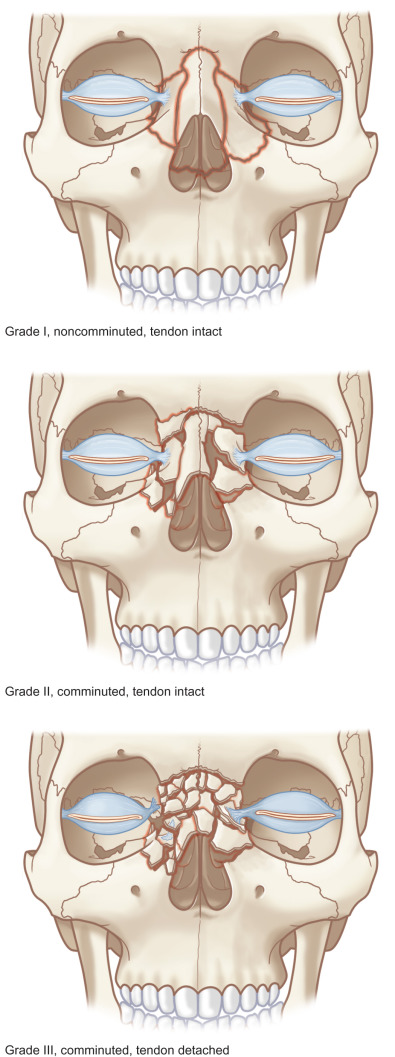
Classification ( Fig. 3.5.9 )
Secondary nasoethmoid fracture classification mirrors that of acute fractures and is useful in formulating a treatment plan. Many alternative systems exist in the literature, but basic distinctions begin with categorizing the fracture(s) as unilateral or bilateral and simple or comminuted. A straightforward classification system previously described by the author is based on the degree of comminution of the medial orbital bone fragment and integrity of the medial canthal tendon. Type I fractures are characterized as large medial orbital rim fragments bearing an intact medial canthal tendon. Type II fractures feature comminuted central bone fragments without extension under the canthal insertion site. The medial canthus is thereby attached to a relatively large piece of intact medial orbital rim. Type III fractures display severe comminution with fracture lines extending under the medial canthal tendon insertion site. The medial canthal tendon is either avulsed or attached to small, nonusable bone fragments. Asymmetry usually exists with higher-grade injuries on one side and lower-grade or absent fractures on the other. The treatment plan is primarily dictated by the higher-grade injury, but an individualized surgical plan for each side is essential ( Fig. 3.5.10 ).
Surgical Indications
Individualized Operative Planning
Once secondary nasoethmoid deformities have been detected, an individualized treatment plan must be made to address each patient’s specific problem while omitting unnecessary surgical interventions. For example, inadequate nasal projection may require cantilever bone grafting, while a foreshortened nose may call for lengthening of the nasal lining, and each of these conditions may or may not be accompanied by an overlying soft tissue derangement that may require its own specific intervention. Enophthalmos requires orbital reconstruction, while a blunted canthal region may require medial canthopexy. Increased interorbital distance often requires medial orbital osteotomy prior to repositioning of bone fragments, perhaps even with slight overcorrection to compensate for expansion due to scarring. The role of the nasoethmoid region in determining orbital relationships cannot be overestimated. Whether due to displacement of the medial orbit or medial canthal tendon or due to an abnormal relationship between orbits from inadequate bony or soft tissue reduction, special attention must be paid to orbital symmetry during secondary nasoethmoid reconstruction.
Traumatic Telecanthus
The assessment and measurement of traumatic telecanthus is a skill that must be honed to ensure the accurate treatment of secondary nasoethmoid fractures. Telecanthus refers to an abnormally increased distance between the medial canthi and differs from orbital hypertelorism, which refers instead to an increased interpupillary distance or bony interorbital distance (dacryon to dacryon). Calipers may be used to measure intercanthal and interpupillary distances, which average 30–31 mm and 60–62 mm in a typical adult, respectively. Telecanthus becomes noticeable at varying distances, since the interpretation is relative to other facial structures, but distances greater than 40 mm are typically an indication for operative intervention.
Enophthalmos
Subtle variations in the degree of ocular projection may go unnoticed and do not require intervention when asymptomatic. Enophthalmos becomes noticeable when greater than 3–4 mm, which indicates the possibility of improvement by surgical management. Enophthalmos is measured from the lateral orbital rim to the anterior border of the cornea with a Hertel exophthalmometer. If the lateral orbital rim is also malpositioned, then a Naugle exophthalmometer may be used, which uses reference points above and below the superior and inferior orbital rims, respectively.
The preoperative consultation should include a discussion of reasonable expectations for outcome. Photographs predating the original injury may help guide the reconstruction, although they must be viewed in the context of the delayed nasoethmoid repair setting. An anticipation of a restored perfect premorbid appearance must be tempered to the actual goals of symmetry, correction of any obvious deformity, and relief of the patient’s symptoms.
Virtual Surgical Planning
Three-dimensional computerized planning may be employed in the virtual environment or physical models may be generated for operative planning and visualization prior to repair of secondary nasoethmoid fractures. However, unlike other secondary craniomaxillofacial deformities, which might feature larger bony structures amenable to individualized custom implant reconstruction or custom cutting guides, the fine anatomy of the nasoethmoid region requires meticulous repair of native tissue. Therefore, the benefit of virtual planning is largely for the surgeon’s preoperative visualization of the intended reconstruction. However, 3D models are beneficial in analyzing the displaced or deformed medial orbital wall segments as well as planning osteotomies.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree