Fig. 32.1
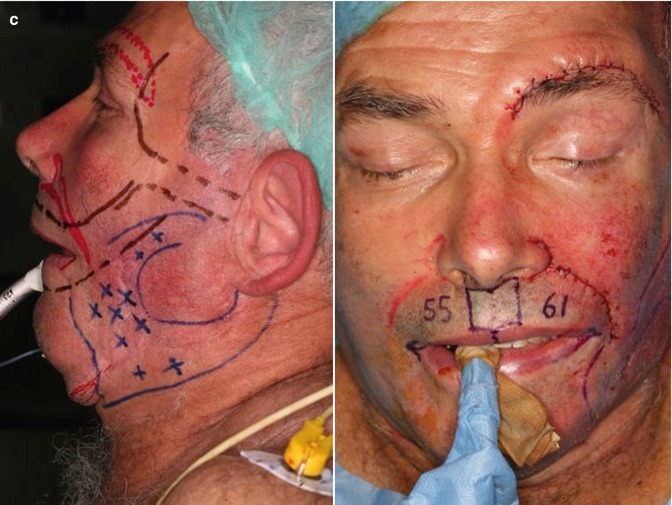
(a) Left and center: Preoperative patient. Right: Skin markings showing the volume defect of the cheek and perimandibular region. (b) First operation. Intraoperative homologous fascia lata before insetting through an extended preauricular and a nasolabial fold skin incisions. (c) Second operation. Left: Intraoperative skin markings showing the skin excess to be resected at the nasolabial fold and left brow (red lines) and the area to be injected with fat (blue lines). Right: Following direct brow lift, skin removal from the nasolabial fold, and extensive lipofilling of the superficial layers of the skin, before left commissuroplasty. (d) Eighteen months postoperative
This 64-year-old man presented with the late sequelae of a gunshot injury to the left side of his face. At the time of injury, he had his left mandible successfully reconstructed with a fibula flap. The posttraumatic left-sided facial palsy was left untreated. In a later attempt to restore the posterior height of the reconstructed mandible for prosthetic purposes, vertical bone distraction of the fibula flap was performed, which failed leaving behind a weakened bone buttress. At inspection, right-sided facial deviation, left brow ptosis, and a severely deficient lower third of the face hesitated. The skin was heavily scarred, with hypotrophic zones and areas with multiple telangiectasias. Based on the patient’s requests, static correction of the facial asymmetry was achieved in three consecutive operations. At first, facial deviation was corrected by means of static sling suspension with the use of homologous fascia lata; a 1.2 g platinum eyelid chain (Berghaus/Schrom) was inserted and a lateral canthoplasty was performed to treat lagophthalmos; Coleman’s lipostructure was performed to correct the deficient cheek volume and 50 mL of fat was deposited in layers starting from the fibular bone to the subcutaneous tissue. In the second operation, left commissuroplasty, nasolabial fold skin excision, and direct brow lift were done. Simultaneous lipofilling was performed using an 18G epidural needle to increase the volume of the cheek (20 mL), whereas subdermic infiltration of fat (5 mL) was done with a 22G epidural needle to release scarred skin. Final correction consisted of the lower eyelid ectropion correction using ear cartilage graft. Eighteen months later, acceptable symmetry of the lower face is retained; likewise, telangiectasias and skin pliability and tropism greatly improved with the time.
Case 2 (Fig. 32.2)

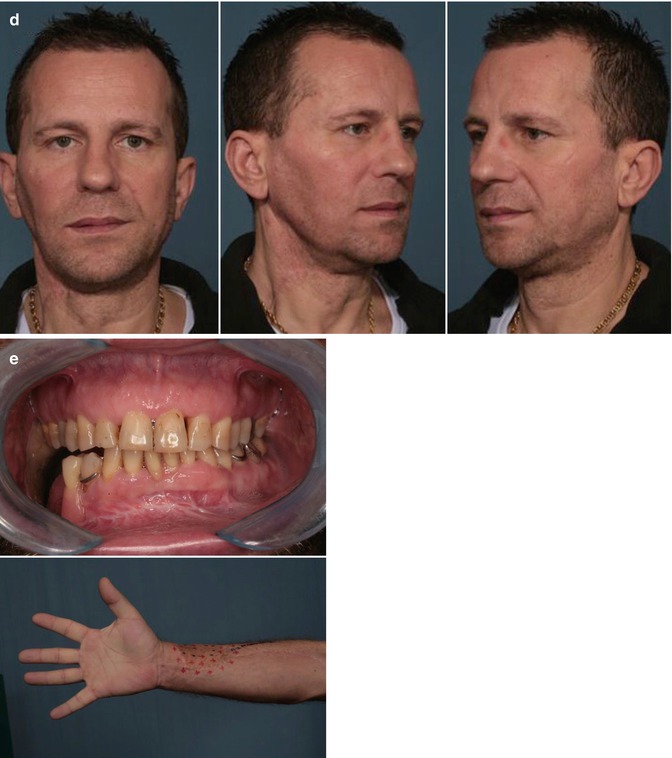
Fig. 32.2
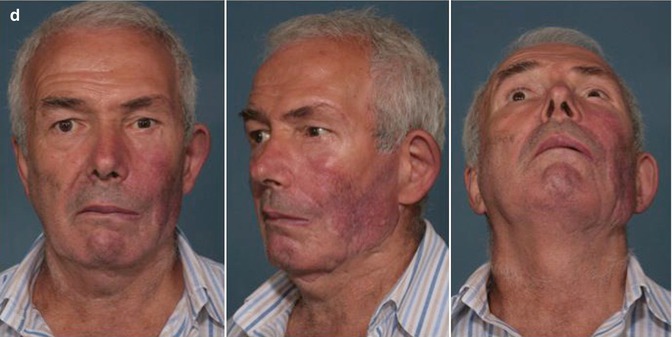
(a) Preoperative patient 1 year after oral cancer surgery. (b) Top: Preoperative 3D computed tomography (CT) reconstruction of the operated site showing inferior displacement of the reconstruction plate and the fracture of one screw at the mental region. Bottom: Patient showing malocclusion and lateral canting of the mandible. (c) Top: Skin markings of the cervicofacial areas to be grafted. Volume-deficient zones are outlined for subcutaneous injection (red solid lines), whereas surgical scars are marked for subdermic injection (green dashed line). Bottom: Skin markings of the RFF donor site areas for subcutaneous (red solid lines) and subdermal injection (dashed lines). The area of hyperesthesia at the radial side of the forearm is also demarcated for subcutaneous injection (green solid line). (d) Six months postoperative. (e) Postoperative. Top: Intraoral occlusion following replacement of the reconstruction plate. Bottom: Improved skin graft texture at the volar aspect of the forearm
A 47-year-old man presented with squamous cell carcinoma (SCC) of the retromolar trigone in autumn 2010. He underwent tumor resection, which included right mandibulectomy, ipsilateral modified radical neck dissection, and simultaneous reconstruction of the mandible, gingiva, and soft palate with a radial forearm flap (RFF) and a 2.4 locking reconstruction plate. No adjuvant therapies were necessary (pT2pN0M0G2R0). Slight facial and cervical asymmetry hesitated, which worsened 1 year later due to dislocation of the reconstruction plate. The patient also complained regarding cosmetics and dysesthesia of the forearm, although RFF was harvested in a suprafascial plane and the full-thickness skin graft used to cover the cutaneous defect took completely. In one single operation, the plate was repositioned through a transoral approach, and the lipoaspirate obtained from the lower abdomen was injected partly in the submandibular region and posterior triangle to fill up the volume defect (40 mL) and partly in the subdermic plane of the skin graft at the forearm (15 mL), using 18 and 22G epidural needles, respectively. Six months after surgery, improved facial symmetry is achieved, occlusion is repaired, and skin graft texture and sensation increased.
Case 3 (Fig. 32.3)
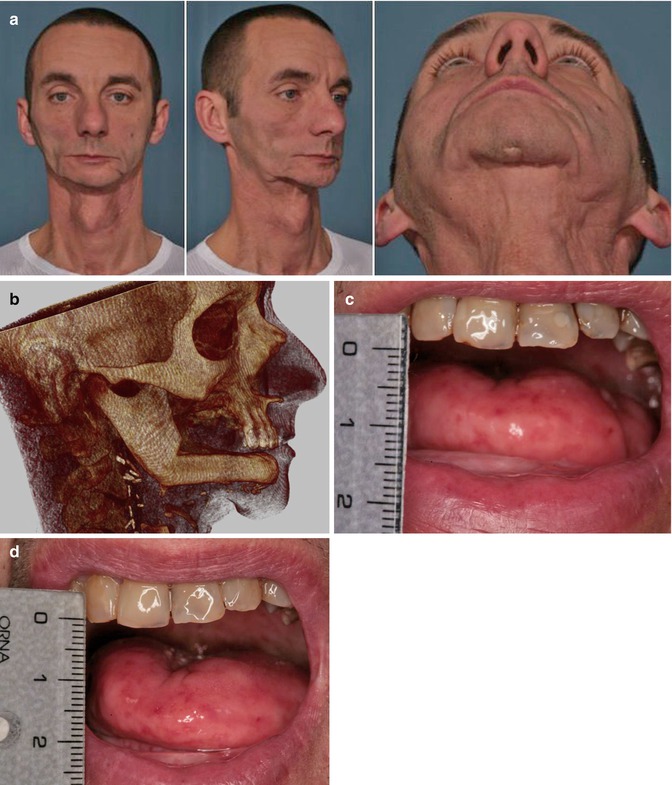
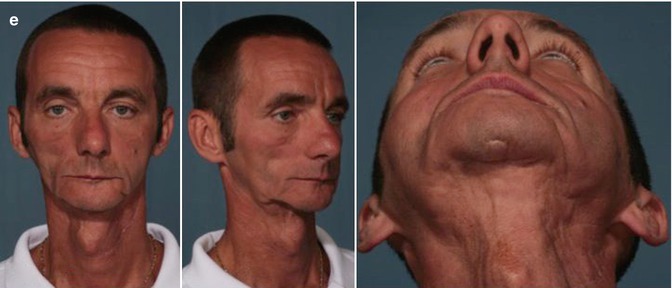
Fig. 32.3
(a) Preoperative patient 1 year after subtotal mandibular reconstruction with a vascularized fibula flap. Left: Marionette jaw deformity. Center: Irradiated mental skin stuck to the underlying bone flap. Right: Hollowing of the entire submental region. (b) Postoperative 3D-CT reconstruction of the reconstructed mandible after fixation hardware removal and completion of the first lipografting procedure. (c) Postoperative. Maximum mouth opening (15 mm), caused by progressive oral submucous fibrosis. (d) Six months postoperative, there is improved mouth opening (true 5 mm gain) obtained after a single submucosal injection of fat. (e) Six months postoperative after dental implant surgery and the second lipografting session. Left and center: Improved skin tropism and texture are noticeable. Right: Reduction of the submental chin depression
A 40-year-old man presented with late postradiation facial sequelae following nonsurgical treatment for an adenocarcinoma of the base of the tongue (70 Gy). The patient had a 4-year history of osteoradionecrosis of the mandible, with substantial skin and mucosal radiation damage. He underwent successful subtotal mandibular reconstruction with an osteomuscular fibula flap in September 2011. Postoperatively, the patient developed right-sided maxillary osteoradionecrosis. Additionally, the thin radiated skin of the lower third of his face firmly stuck to the underlying bone giving the appearance of a marionette jaw. Four months after the first operation, he underwent a right low maxillectomy and the removal of fixation hardware from the fibula through a transoral approach. A first lipofilling procedure (Coleman’s technique) was performed at that time, when the entire perimandibular region was infiltrated in layers starting from the fibular bone to the subcutaneous tissue with 23 mL of lipoaspirate harvested from the entire abdomen and flanks, using a 2 mm single-hole blunt cannula. The amount of fat ready for transfer was limited by the extreme thinness of the patient.
A restricted mouth opening hesitated afterward (15 mm), due to progressive oral submucous fibrosis. A second lipofilling procedure was planned at the time of dental implant placement. Thirty cc of lipoaspirate was harvested with a 1 mm single-hole blunt cannula and centrifuged for 1 min at 1,000 rpm. Fifteen milliliters of fat was injected in the subcutaneous plane using an 18G epidural needle, whereas 10 mL of lipoaspirate was injected in the subdermic layer of the mental region and five cc in the submucosal plane of the right cheek, using a 20G epidural needle. At the same time, six dental implants were inserted in the neo-mandible. Mouth opening increased to 20 mm within 6 weeks and maintained at 6-month follow-up. Improved skin pliability, thickness, and pigmentation were achieved, but additional lipofilling sessions would be necessary to restore the desired volume after completion of the implant-supported prosthesis.
Case 4 (Fig. 32.4)

Fig. 32.4
(a) Preoperative patient showing chronic skin ulceration and plate exposure in the mental region. Sequelae of previous flap surgery and radiotherapy are obvious, with the entire cheek and cervical skin firmly attached to the underlying bone. (b) Preoperative 3D-CT reconstruction of the reconstructed mandible reveals gross asymmetry of the inferior third of the facial skeleton and the presence of the fixation hardware extruded through the perimandibular skin. (c) Intraoperative. Injection of fine lipoaspirate with 20G epidural needle at the dermoepidermal junction of the chronic wound. (d) Postoperative showing improved skin texture and viability, with complete healing of the ulcer and coverage of bone and fixation hardware, following two consecutive lipofilling sessions
A 58-year-old man presented in 2011 with nonhealing open wound in the mental region, with bone and titanium plates exposure. Several years earlier, he had the left mandible resected and reconstructed with a vascularized iliac crest flap and received full-dose radiotherapy (65 Gy) for sarcoma treatment. The operation was successful but gross facial asymmetry hesitated. Mandibular osteotomies were then done in an attempt to restore symmetry, which got infected and required additional revision surgery. The patient eventually developed chronic osteomyelitis of the right mandible, with intraoral bone exposure of necrotic bone. The patient was scheduled for major mandibular reconstruction but first opted for sequential fat grafting procedures at 6-month intervals, trying to improve the quality of the irradiated perimandibular skin and ulcer, with the aim of preserving the facial skin as much as possible.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








