Rhinoplasty remains one of the most challenging plastic surgery procedures for cleft patients. These patients present years after the initial cleft repair to correct residual nasal deformities.
The nature of the procedure varies from patient to patient depending on the nasal deformities. Systematic reorientation of distorted nasal architecture and creation of a balanced platform for the lower lateral cartilages constitute some of the cardinal principles for correcting the cleft lip nose deformities.
Radix is the depth of the nasal root at the nasofrontal angle. This angle connects the brow and the dorsum through a soft concave curve. Although this angle can vary from 128 to 140 degrees, it is ideally 134 degrees in females and 130 degrees in males.
Nasal dorsum is assessed using the curvilinear dorsal aesthetic lines traced from the supraorbital ridge to the tipdefining points. Ideally, the width of the dorsal aesthetic lines should match the width of either the tip-defining points or the interphiltral distance.
Nasal deviation is evaluated by drawing a line from the midglabellar area to the menton, bisecting the nasal ridge, upper lip, and Cupid bow. Deviation of the nose from this line would most likely require septal surgery for correction.
The upper lateral cartilage (ULC) overlaps the nasal bones, septum, and the lower lateral cartilages (LLCs). The internal valve is the angle formed by intersection of the nasal septum and the caudal margin of the ULC.
LLCs comprise medial, middle, and lateral crura, which are connected to each other, the ULCs, and the septum by fibrous tissue and ligaments. Modification in any of these structures alters tip projection.
The nasolabial angle is used to determine the degree of tip rotation. This angle is obtained by measuring the angle between a line coursing through the most anterior and posterior edges of the nostril and a line dropped perpendicular to the natural horizontal facial plane. This angle should be between 103 to 105 degrees in women and 95 to 100 degrees in men.
The septum, turbinates, and nasal valves (internal and external) serve as the anatomic functional foundation for the nose, by contributing to respiration, filtration, humidification, temperature regulation, and protection.
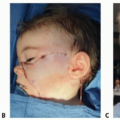
Although nasal deformities are partially corrected during cleft lip surgery, patients often present years after the initial cleft repair to correct residual nasal deformities.
Efforts to correct nasal deformity in patients between the ages of 4 and 14 years may have a significant chance of supratip deformity and loss of tip definition, with widening and thickening of the skin.
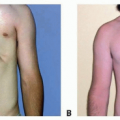
Many patients with bilateral and complete cleft lip deformities have other craniofacial abnormalities, particularly deformities of the maxilla. Correction of the skeletal deformity sets the stage for a more successful correction of the nasal deformity.
Approximately 60% of patients with cleft lip nasal deformity have difficulty breathing through the nose. Correction of physiologic function of the nose should be addressed at the time of correction of the nasal deformity.
Many of the patients may have asymmetry involving parts other than the nose and the lip. Therefore, it is important to assess the entire face and note asymmetry before analyzing the nose in detail (Table 1).1
Table 1 Detailed Nasal Analysis
Structure
Assessment
Skin
Thickness
Quality of the tissue for reconstruction
Nasal bone
Symmetry
Length
Distance from the midline
Depth of radix
Presence or absence of a dorsal hump
Midvault
Upper lateral cartilage collapse
Vertical symmetry
Nasal tip
Shape—bulbous, boxy, narrow, or parenthesis deformity?
Symmetry
Fullness
Projection
Infratip lobule size
Nasolabial angle
Direction of the columella
Alar base
Comparison of thickness of the ala
Vertical position
Configuration of nasal sill
Nostrils
Symmetry
Internal nose
Stenosis of the internal and external valve
Presence or absence of a deviated septum
Size and shape of the turbinates
Synechiae
Septal perforation
Table 2 Features of Unilateral Cleft Lip Nasal Deformity
The columella is shorter on the cleft side.
The base of the columella is deviated to the noncleft side.
The lateral crus of the lower lateral cartilage is longer on the cleft side.
The nasal tip is displaced in both the frontal and the horizontal planes.
The nasal tip is asymmetric.
The ala is flattened, resulting in horizontal orientation of the nostril.
The nostrils are asymmetric.
The entire nostril is retropositioned because of the deficiency in the underlying frame.
The base of the ala is displaced laterally and/or posteriorly and sometimes inferiorly.
The nasal floor is caudal on the cleft side.
A nasolabial fistula could be present.
The septum and anterior nasal spine are shifted toward the noncleft vestibule.
The nasal septum is deviated, resulting in a varying degree of nasal obstruction.
The inferior turbinate on the cleft side is hypertrophic.
The maxilla is hypoplastic on the cleft side.
The premaxilla and the maxillary segments are displaced.
From Guyuron B. MOC-PS(SME) CME article: late cleft lip nasal deformity. Plast Reconstr Surg. 2008:121(4):1-11, with permission.
Table 3 Features of Bilateral Cleft Lip Nasal Deformity | ||
|---|---|---|
|
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree