Following Mohs reconstruction, several options are available to improve the appearance of the resulting scars. It is critical that the patient has realistic goals before beginning any treatment because scars can be improved but never erased. The surgical and nonsurgical options aim to replace pre-existing scars with ones that are less conspicuous. This article addresses the different available options (listed in order of invasiveness) for improving scarring following Mohs reconstruction.
Key points
- •
The ideal scar is narrow, flat, level with surrounding skin, and difficult for the untrained eye to see due to incision placement and color match.
- •
Dermabrasion should extend down to the papillary dermis with careful attention not to injure the reticular dermis because additional scarring can result.
- •
Laser resurfacing is an alternative to dermabrasion, either of which can be performed early in the healing process.
- •
Some scars are best treated with surgical revision followed by the nonsurgical adjuncts to achieve the ideal result.
- •
Serial Z-plasty is often useful for trap-door deformity of a prior local flap.
Introduction
To achieve the optimal results following Mohs reconstruction, the surgeon has many available options. First, it is important to realize that, despite the surgeon’s best efforts, it is impossible to erase a scar because all wounds and incisions result in scar formation. The techniques outlined by Dr Halsted in 1929 should be applied to all wound closures. These include gentle handling of tissue, aseptic technique, sharp anatomic dissection of tissue, careful hemostasis, obliteration of dead space, avoidance of tension, and reliance on rest. Beyond these considerations, the patient’s individual factors determine the speed and effectiveness of wound healing. The wound will progress through the classic 3 stages (inflammation, proliferative, remodeling) with the final appearance being reached approximately 1 year after the initial surgery.
Several factors contribute to poor scar formation. These include, but are not limited to, tissue ischemia, traumatic tissue handling, infection, and poor flap design. Some of these factors are preventable, whereas others are not. For example, excessive tension causes widened scars. Also, inadequate wound edge eversion predisposes to depressed scars. Other technical causes include uneven approximation of wound edges, insufficient undermining, or lack of deep closure; all of which can lead to suboptimal scars. Patient factors that the surgeon cannot control include diabetes, Accutane use, radiation therapy, sun exposure, tobacco use, and poor nutritional status.
For analysis, the ideal scar is narrow, flat, level with surrounding skin, and difficult for the untrained eye to see due to incision placement and color match. Generally, surgeons wait to revise or consider alternative treatment modalities at least 6 to 8 weeks following initial reconstruction. At that time, the wound has rebuilt enough tensile strength to withstand the additional treatments. In general, the nonsurgical options can be performed at an earlier date, whereas surgical revisions are recommended after a period of 3 to 6 months.
Introduction
To achieve the optimal results following Mohs reconstruction, the surgeon has many available options. First, it is important to realize that, despite the surgeon’s best efforts, it is impossible to erase a scar because all wounds and incisions result in scar formation. The techniques outlined by Dr Halsted in 1929 should be applied to all wound closures. These include gentle handling of tissue, aseptic technique, sharp anatomic dissection of tissue, careful hemostasis, obliteration of dead space, avoidance of tension, and reliance on rest. Beyond these considerations, the patient’s individual factors determine the speed and effectiveness of wound healing. The wound will progress through the classic 3 stages (inflammation, proliferative, remodeling) with the final appearance being reached approximately 1 year after the initial surgery.
Several factors contribute to poor scar formation. These include, but are not limited to, tissue ischemia, traumatic tissue handling, infection, and poor flap design. Some of these factors are preventable, whereas others are not. For example, excessive tension causes widened scars. Also, inadequate wound edge eversion predisposes to depressed scars. Other technical causes include uneven approximation of wound edges, insufficient undermining, or lack of deep closure; all of which can lead to suboptimal scars. Patient factors that the surgeon cannot control include diabetes, Accutane use, radiation therapy, sun exposure, tobacco use, and poor nutritional status.
For analysis, the ideal scar is narrow, flat, level with surrounding skin, and difficult for the untrained eye to see due to incision placement and color match. Generally, surgeons wait to revise or consider alternative treatment modalities at least 6 to 8 weeks following initial reconstruction. At that time, the wound has rebuilt enough tensile strength to withstand the additional treatments. In general, the nonsurgical options can be performed at an earlier date, whereas surgical revisions are recommended after a period of 3 to 6 months.
Intralesional steroid injections
Although triamcinolone injections are commonly used for the treatment of hypertrophic scars and keloids, they are also effective adjuncts during the initial stages of wound healing to reduce tissue edema. Triamcinolone preparation comes in 2 concentrations: 10 mg/mL and 40 mg/mL. The application of these injections is extremely variable in the literature and largely depends on individual surgeon’s preferences. The senior author advocates using small amounts of triamcinolone 10 mg/mL injected intralesionally at intervals of 2 to 4 weeks. The amount injected is usually on the order of 0.05 mL to 0.5 mL, depending on the targeted area. The rationale for serial injections using small quantities of triamcinolone is to limit the side-effect profile of the treatment. Intralesional steroid injections can cause thinning of the dermis with subcutaneous fat atrophy, resulting in a skin divot. Additionally, pigmentation changes (especially in darker individuals) and the creation of surrounding telangiectasias have been described. Once these side effects occur, they can be very difficult to address; it is recommended that treatment be performed in a conservative manner.
Dermabrasion
An effective scar treatment that has been in use since 1500 BC is mechanical resurfacing, also known as dermabrasion. It is a minimally invasive procedure aimed at smoothing small surface irregularities resulting in a softer scar appearance. It has been studied extensively. Compared with laser resurfacing, it has a lower cost, a better safety profile, and can be used in almost any outpatient setting. Dermabrasion is ideally performed 6 to 8 weeks following the initial surgical procedure. At this point in the wound healing process, tensile strength is essentially maximized at 80% and can withstand the stresses of the procedure. Of note, dermabrasion can also be performed at a later date with similarly effective results.
Preoperative Consideration
In addition to taking a full medical history, surgeons should be particularly careful in obtaining a medication history. Ideally, the use of anticoagulants should be discontinued 2 weeks before the procedure. Isotretinoin (Accutane) should be discontinued for 6 to 12 months prior due to the concern of causing hypertrophic scarring and keloid formation. If a patient has a history of herpes simplex virus (HSV) outbreaks, he or she should be treated prophylactically with antivirals. Some surgeons advocate treating all patients with antivirals regardless of history. Although the senior author typically does not prescribe preoperative medications for localized treatment, 2 medications have been studied in the context of facial resurfacing to prevent hyperpigmentation: hydroquinone and retinoic acid. Hydroquinone inhibits melanocyte conversion of tyrosine to dihydroxyphenylalanine (DOPA), causing a reversible lightening of the skin. It is typically prescribed as a 4% topical cream or gel that is applied twice daily. Retinoic acid, a vitamin A derivative, has been shown to result in accelerated re-epithelialization when applied daily starting 2 weeks before dermabrasion.
Equipment
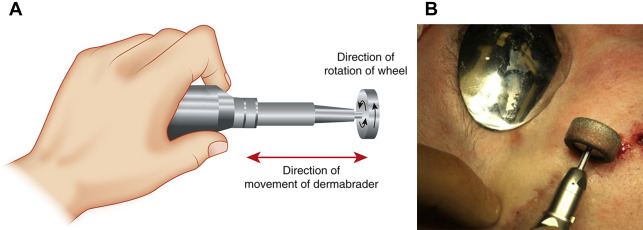
A variety of dermabrasion equipment brands are available ( Fig. 1 ). Of significant help is a dermabrasion unit that allows foot control, reversible direction, and variable speed. Typically, for facial scars, diamond fraises of variable coarseness are used. Wire brush heads are avoided on the face as they tend to cause unintended deep dermis injury.

Procedure
Universal precautions should be used by all staff because the treated tissue and blood products can be spread into the air. This includes gowns, gloves, and surgical masks with eye protection. The targeted area is then anesthetized, usually with local injection of 1% lidocaine with 1:100,000 epinephrine. If a larger area is being treated, then the addition of a nerve block can be used. The skin is then prepped in a sterile fashion and the superficial skin can be inked to provide a reference for the surgeon. The targeted area is then treated until diffuse punctate bleeding is noted. This finding signifies that the depth of injury is within the papillary dermis. The reticular dermis, which has a yellow chamois color and visible collagen strands, houses the adnexal structures (sweat glands, hair follicles, sebaceous glands) that are necessary for re-epithelialization. If these deeper structures are injured, scarring is likely to occur ( Fig. 2 ).