(1)
Department of Anatomy, Medical School Democritus University of Thrace, Alexandroupolis, Evros, Greece
Abstract
Five distinct layers structure the scalp: the skin, the connective subcutaneous tissue, the galea aponeurotica and the muscles, the loose areolar tissue, and the pericranium. In the temporal region, the layers increase in number and the fascial anatomy becomes more complex. The scalp and the temple are supplied by the superficial temporal, the supraorbital, the supratrochlear, the posterior auricular, and the occipital vessels. The rich vascular network that is formed allows for the design of a great number of versatile, random, or axial pattern flaps. Robust, predominantly rotation and transposition, flaps can be derived and used for the reconstruction of even the largest defects with safety.
The scalp is defined as the hair-bearing part of the soft tissues that cover the cranial vault. The scalp is bounded anteriorly by the anterior hairline, posteriorly by the superior nuchal lines, and laterally by the posterior part of the zygomatic arches. The frontal process of the zygomatic bone and the zygomatic process of the frontal bone delimit the temporal region anteriorly. Superiorly and posteriorly, the region is bordered by the superior temporal line and inferiorly by the zygomatic arch.
The hair-bearing scalp extends to the parietal and the occipital regions, but laterally, at the temporal region, it stretches in a variable area that depends on the position of the temporal hairline (Fig. 2.1).
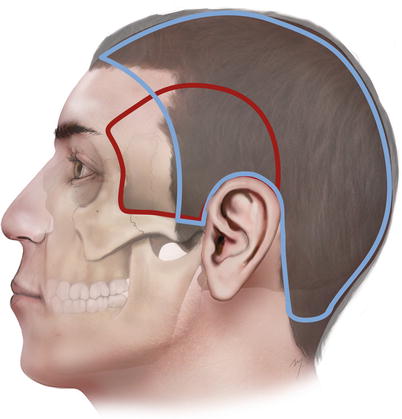
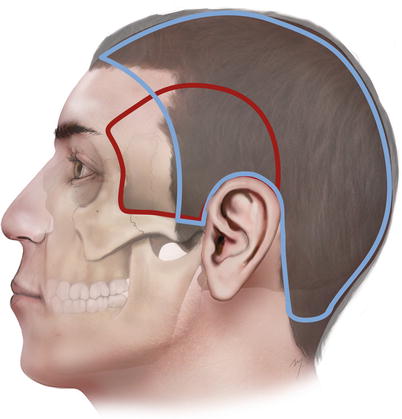
Fig. 2.1
Boundaries and overlap of the scalp to the temporal region
2.1 Layered Anatomy of the Scalp
The scalp consists of five distinct layers. These are the same layers, with the same arrangement, that cover the forehead and continue superiorly covering the cranial vault until reaching the back of the head (Fig. 2.2). The layers of the scalp are consisted of the skin, the subcutaneous connective tissue, the occipitofrontalis muscle and the epicranial aponeurosis, the loose areolar connective tissue, and the pericranium (Fig. 2.3). The known mnemonic device SCALP is a useful tool to remember these layers:
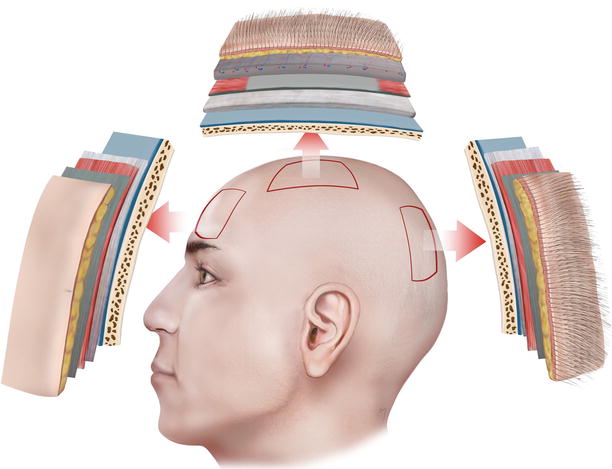
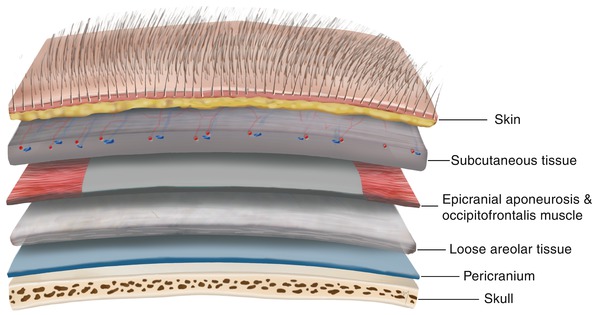
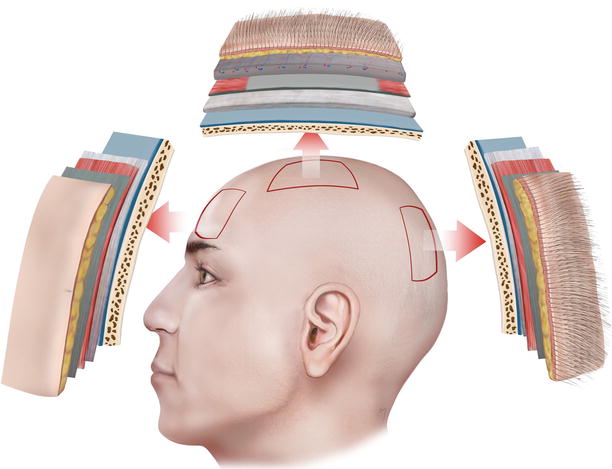
Fig. 2.2
The same five-layered soft tissue covering of the forehead continues up to the cranial vault constituting the scalp
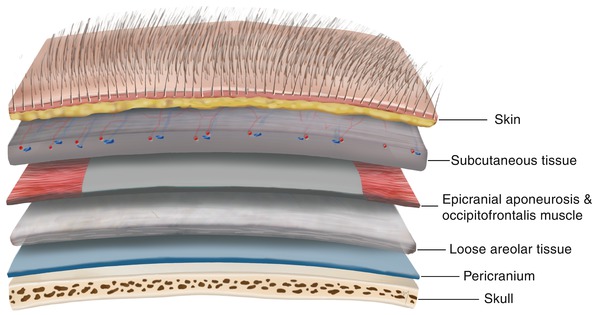
Fig. 2.3
The five layers of the SCALP
S: Skin
C: Connective (subcutaneous) tissue
A: Aponeurosis and muscles
L: Loose areolar tissue
P: Pericranium
The first three layers are firmly attached to each other constituting a surgically single unit.
2.1.1 Skin
The scalp skin, being its first layer, is one of the thickest dermises of the body. It is thicker in the occipital area, with a thickness of 8 mm, and thinner in the vertex, where it is 3 mm (Matloub and Molnar 1996). Its thickness decreases during the aging process, by the presence of baldness, and it is thinner in females. It is firmly bound to the underlying subcutaneous connective tissue layer and difficult to separate from it. It contains, beneath the dermis, the hair follicles and numerous sebaceous and sweat glands.
The relaxed skin tension lines at the scalp are oriented in a coronal direction, parallel to the ones of the forehead; at the frontal scalp, they run from front to back; at the mid-scalp, they run in a sagittal direction and turn into a horizontal direction; and at the posterior scalp, they run at a slightly oblique direction (Fig. 2.4).
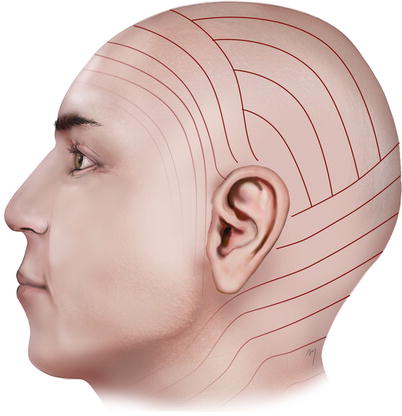
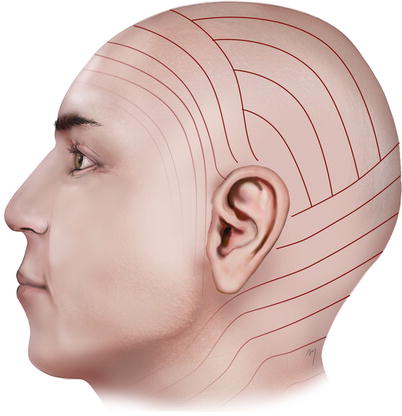
Fig. 2.4
Relaxed skin tension lines (RSTLs) at the scalp
2.1.2 Connective Subcutaneous Tissue
The second layer is the subcutaneous connective tissue (Fig. 2.3). It is a fibrofatty, firm, dense, and vascular layer that connects the skin to the underlying epicranial aponeurosis. It is a layer with an average thickness of 4–7 mm even though a natural thickness of 20 mm has been observed (Hayman et al. 2003).
Multiple fibrous septa divide this layer into small compartments. The large vessels that run over the surface of the underlying musculoaponeurotic layer just beneath this layer give branches within this layer that form a rich subcutaneous vascular plexus. These vessels are attached to the fibrous septa, which diminishes their ability to contract when they are cut. This leads to the profuse bleeding encountered in scalp incisions or in scalp trauma. Nerves and lymphatic vessels are situated also in this layer.
2.1.3 Aponeurosis and Muscles
The musculoaponeurotic layer, third layer, of the scalp consists of the aponeurosis, correctly termed as the epicranial aponeurosis, the occipitalis muscles, and the upper portion of the frontalis muscles (Fig. 2.5). The frontalis muscle and the occipital muscle are the anterior and posterior bellies of the two occipitofrontalis muscles that together with their intermediate connection, epicranial aponeurosis, cover, as a broad musculofibrous layer, the dome of the skull from the highest nuchal lines to the eyebrows.


Fig. 2.5
The musculoaponeurotic layer of the scalp: frontalis muscle-galea aponeurotica-occipitalis muscle
2.1.3.1 Epicranial Aponeurosis
The epicranial aponeurosis (also termed galea or galea aponeurotica) is a thin, inelastic, broad tendinous sheet of connective tissue that lies over the dome of the skull, joining both the paired frontalis and occipitalis muscles. Its thickness ranges from 1 to 2 mm. In actuality, the galea, as mentioned, corresponds to the aponeurotic compartment of the occipitofrontalis muscle, which posteriorly encompasses the occipital bellies and in the forehead the frontal bellies. Laterally, in the temporal region, it fuses with the temporoparietal fascia.
The dense and tendinous nature of the galea makes the scalp flaps rigid and stiff, sometimes making it difficult to achieve adequate flap mobility so as to close a defect with ease and without tension. This is more obvious in the vertex of the scalp where the galea is much more resistant in distension. Therefore, strict geometry of flap design in the scalp is mandatory.
A useful tip to release some of the galea’s tension is the “galeal scoring” (Fig. 2.6). With this technique, galeal incisions are made every 0.5–1 cm, in a depth that preserves the underlying vessels parallel to the foremost edge of the flap (Jackson 2007). Although this “tip” was first described in 1944 by Kazanjian and Holmes brought about by their experience, later, biomechanical studies of this principle were performed. Raposio et al. (1988) found out that galeotomy can reduce the closing tension even by 40 % and gain a flap lengthening approximately 1.5 mm per galeotomy.
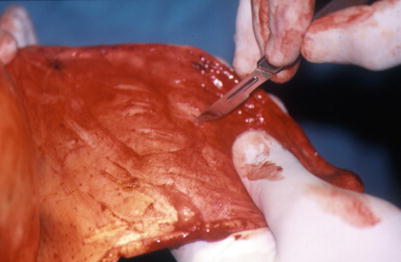
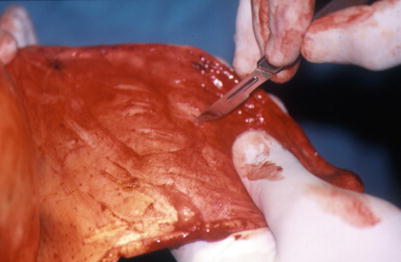
Fig. 2.6
Galeal scoring
The galea tightly adheres to the overlying subcutaneous connective tissue layer but is loosely connected to the underlying pericranium through the layer of loose areolar connective tissue.
Among the frontal and occipitalis muscles, only the last is involved with the hair-bearing scalp. The frontal muscle as far as it occupies the frontal region is examined in detail in the Chap. 3.
2.1.3.2 Occipitalis Muscle
The paired occipitalis muscles (Fig. 2.7) are thin and quadrilateral in shape originating by the tendinous fibers from the lateral two-thirds of the superior nuchal line and from the mastoid part of the temporal bone. They travel a short course after which its fibers insert into the galea. A space, which leaves between the two occipital muscles, is filled by a posterior extension of the epicranial aponeurosis. Branches of the posterior auricular and occipital arteries supply each occipitalis muscle. They are innervated by the posterior auricular branch of the facial nerve. The occipital muscles act to move the scalp backward.
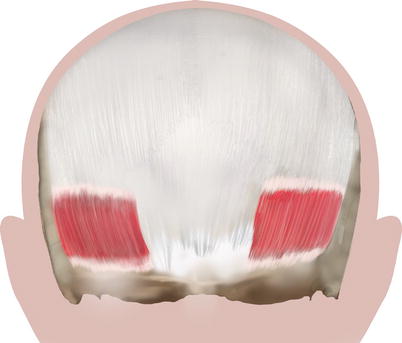
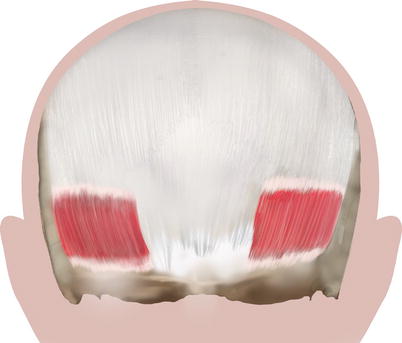
Fig. 2.7
Occipitalis muscles
2.1.4 Loose Areolar Tissue
The loose areolar tissue layer of the scalp is actually a subgaleal space that connects the musculoaponeurotic layer with the pericranium (Fig. 2.8). Its thickness ranges from 1 to 3 mm (Tremolada et al. 1994). The loose areolar tissue layer continues in the forehead and extends laterally to the temporal area, beneath the temporoparietal fascia and over the temporalis fascia. From a lateral aspect, the loose areolar tissue layer is attached in a line starting from the frontal process of the zygoma, continuing laterally along the superior aspect of the zygomatic arch, above the external auditory meatus, and over the mastoid process and superior to the attachments of the sternocleidomastoid and trapezius muscles. Posteriorly it terminates along the superior nuchal line by fusing with the periosteum (Tolhurst et al. 1991). Due to this loose layer, the galea and the tightly overlying superficial structures can freely move over the periosteum of the skull bone.
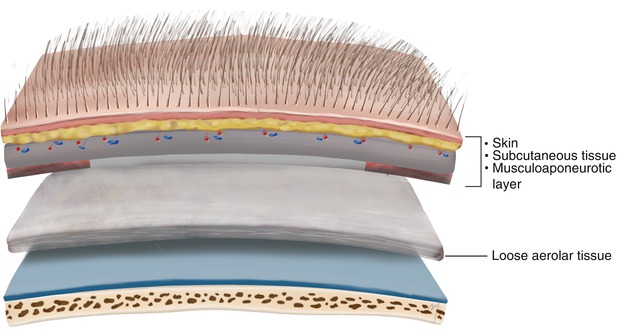
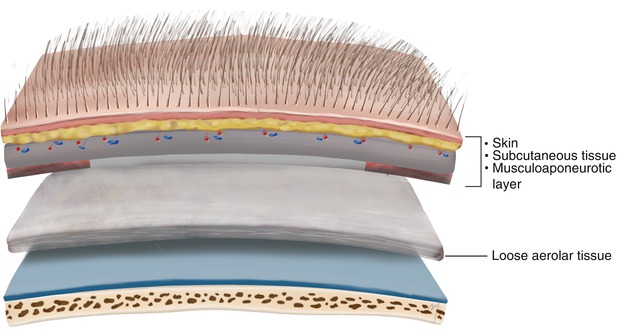
Fig. 2.8
Loose areolar tissue layer. The above the loose areolar tissue three layers are firmly attached to each other constituting a surgically single unit
In terms of microstructure, this layer is composed of multiple and of various thickness fibrous laminae that run parallel and are loosely adherent to one another (Tremolada et al. 1994). The loose areolar tissue layer is often referred to as an avascular space although in reality it is a clearly vascularized layer. Tiny branches that are derived from the overlying blood vessels can be seen running through it. Some of these branches descend deep to the pericranium and the outer table of the skull (Cutting et al. 1984; McCarthy and Zide 1984; Casanova et al. 1986).
This subgaleal layer is of great importance in scalp surgery. Being very loose, it can be easily dissected, creating the surgical dissection plane when raising scalp flaps. Injection of a vasoconstrictive (e.g., epinephrine) solution transforms it practical to an avascular dissection plane.
2.1.5 Pericranium
The pericranium lies just beneath the loose areolar layer and is the skull’s periosteum (Fig. 2.3). It is a dense layer of connective tissue that is adherent to the outer surface of the skull bones and as it runs forward over the supraorbital zone becomes even more adherent. Beyond the superior temporal line, it divides and encompasses the temporalis muscle becoming confluent with the temporalis fascia. Although the pericranium varies in thickness among the different locations, in general it is slightly thinner than the galea. It becomes continuous with the endosteum (the periosteum of the inner surface of the skull) at the interosseous suture lines of the skull bones. Even though it is often stated that the periosteum is difficult to remove at the suture lines, in practice, there is no added difficulty regarding its elevation in this area.
The pericranium receives its blood supply mainly from branches of the overlying major scalp vessels that run through the loose areolar tissue and reach the pericranium. Intracranial vessels that come from the underlying skull bones, as bone perforators, contribute also in the vascularization of the pericranium.
2.2 Layered Anatomy of the Temporal Region
The temporal region even directly related to the scalp, however, is different than the rest of it, having its unique anatomic, microstructural, and mechanical characteristics in the layered structure. In the temporal region, the scalp layers differentiate, become more complex, and increase in number. In general the difference of the five-layered scalp is summarized in the presence of the temporoparietal fascia instead of corresponding to the galea and the presence of temporalis muscle with its muscle fascia, lying between the periosteum and loose areolar tissue layer (Fig. 2.9).
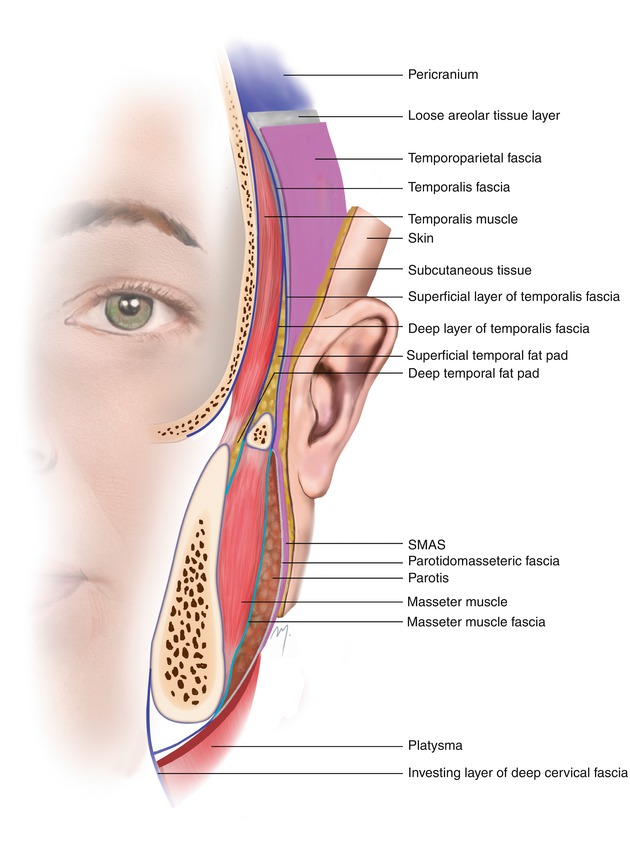
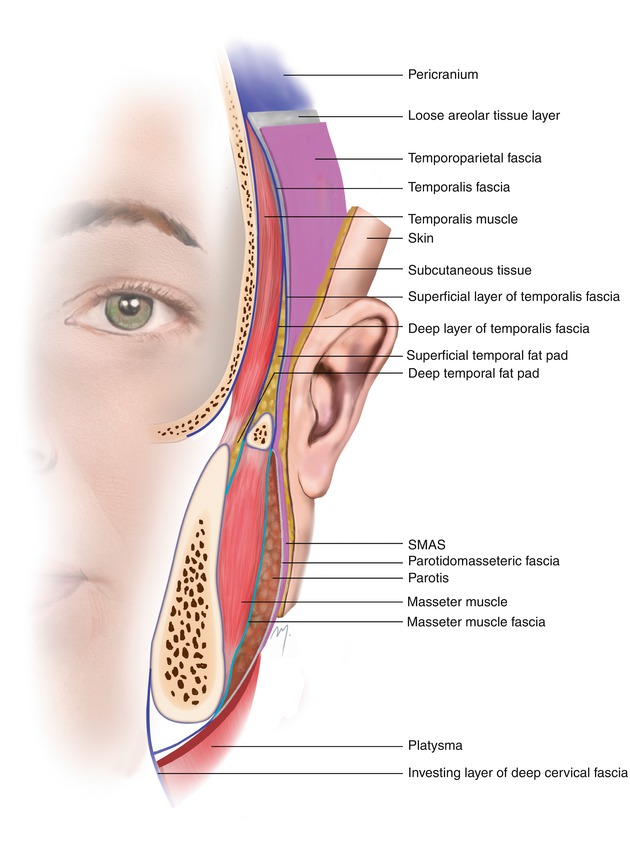
Fig. 2.9
Fascial anatomy of temporal region and lateral face
The presence of an “extension” of the galea (the temporoparietal fascia) in the temporal musculoaponeurotic layer that is not so thick, stiff, and rigid leads to increased elasticity and tissue availability at the temple. The complicated course and layered position of the frontal branch of the facial nerve is another important point to be kept in mind during planning and rising of a flap when a part or the whole of it is derived from the temporal area.
Much confusion has surrounded the anatomy both in the description and nomenclature of the layers at the temporal region. In many descriptions of the 5-layered scalp, there is no differentiation between the structures of the temporoparietal region, resulting in the notion that the same layers are observed throughout. In addition further confusion is brought about concerning the various terms in the nomenclature of the structures, which vary among writers, and the absence of standardized terminology in classic anatomic textbooks. The terminology that follows is close to the precise anatomic identification of each structure but also includes a common ground across different surgical specialties.
2.2.1 Skin and Subcutaneous Tissue
The skin and subcutaneous tissue, the first two scalp layers, remain the same also in the temporal region, firmly attached the one to the other, with the same microscopic anatomic features.
2.2.2 Temporoparietal Fascia, Temporoparietalis Muscle, and Extrinsic Auricular Muscles
The musculoaponeurotic layer (3rd scalp layer) is represented in the temporal area by the temporoparietal fascia along with the extrinsic auricular and temporoparietalis muscles, encompassed by that fascia.
2.2.2.1 Temporoparietal Fascia
The temporoparietal fascia lies just beneath the subcutaneous layer. It extends like a fan from the periauricular area toward and above the superior temporal line where it fuses with the galea (Fig. 2.10). Inferiorly it passes over the zygomatic arch and becomes continuous with the superficial musculoaponeurotic layer (SMAS) of the face (Fig. 2.9).
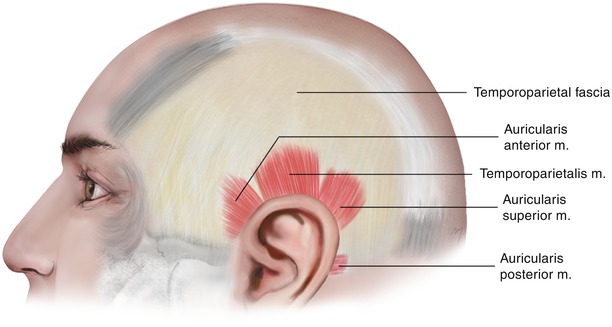
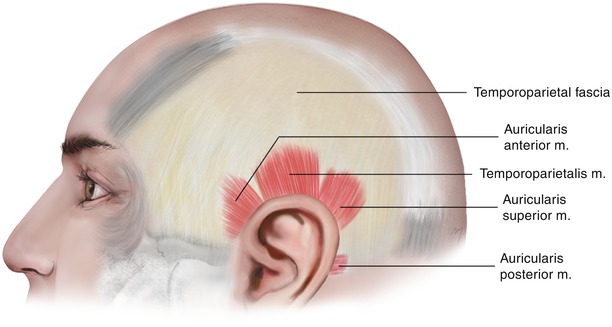
Fig. 2.10
The temporoparietal fascia, the temporoparietalis muscle, and the extrinsic auricular muscles
The superficial temporal artery is related to the temporoparietal fascia. Coming from the preauricular region, it runs within the temporoparietal fascia and continues with its branches gradually transitioning more superficial over its surface. The frontal branches of the motor facial nerve run deep to the temporoparietal fascia, while the auriculotemporal sensory nerve runs above the temporoparietal fascia.
The temporoparietal fascia is thin (approximately 2–3 mm) but wide enough (approximately 15 × 15 cm) to be harvested as a thin, pliable, and broad flap. On the other hand, it is less dense compared to the galea, which makes skin flaps derived from the temple less stiff and rigid. The temporoparietal fascia is responsible for the particular mobility that the scalp shows at the temporal area and in some extent at the parietal area.
2.2.2.2 Temporoparietalis Muscle and Extrinsic Auricular Muscles
The temporoparietalis muscle, often underdeveloped, belongs in the epicranial muscle group and actually is a muscle sheet, which lies between the frontal part of the occipitofrontalis and the anterior and superior auricular muscles (Fig. 2.10).
The three extrinsic auricular muscles, the auricularis anterior, auricularis superior, and auricularis posterior, are very thin muscles (fan of muscle fibers) that connect the auricle to the scalp and the skull. The auricularis anterior and auricularis superior arise from the galea, and the auricularis posterior arises from the mastoid part of the temporal bone. The muscles receive their blood supply from the posterior auricular artery and are innervated by the frontal and posterior auricular branches of the facial nerve.
2.2.3 Loose Areolar Tissue
The loose areolar tissue layer of the scalp continues at the temporal region between the overlying temporoparietal fascia and the underlying temporalis fascia (Fig. 2.9). Tiny branches coming from the superficial temporal artery are found within the loose areolar tissue layer defining it just like at the scalp as a clearly vascularized space.
The micro-architecture of the loose areolar tissue layer is quite similar to that of the rest of the scalp and is consisted of multiple fibrous laminae (Accioli de Vasconcellos et al. 2003). This layer is the conventional dissection plane for the scalp and temple, in skin flap surgery. Thus, large skin flaps that involve the scalp and the temple (and even the forehead) can be raised at the same level.
2.2.4 Temporalis Fascia
The next layer beneath the loose areolar tissue is the temporalis fascia (temporal fascia, deep temporal fascia). The temporalis fascia is the fascia that immediately lies over and covers the temporalis muscle (Fig. 2.11). It is a white, thick, dense, and strong connective tissue layer that is attached to the superior temporal line. Above the superior temporal line, it fuses with the pericranium.
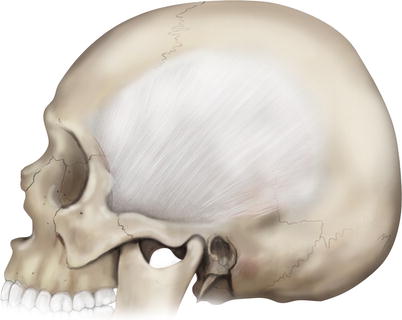
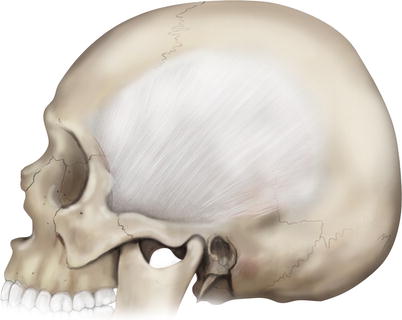
Fig. 2.11
Temporalis fascia
As the temporalis fascia runs inferiorly, 2 cm above the zygomatic arch, a point that corresponds to the level of the superior orbital margin, it splits in two layers, the thick superficial layer (superficial lamina, superficial leaflet) of temporalis fascia and the thinner deep layer (deep lamina, deep leaflet) of temporalis fascia (Fig. 2.9).
The superficial layer of the temporalis fascia attaches to the lateral border of the zygomatic arch. It lies directly over the periosteum and is continuous with the fascia of the masseter muscle. The deep layer of the temporalis fascia attaches to the medial border of the arch and blends with the deep layer of the masseter muscle fascia.
2.2.4.1 Superficial Temporal Fat Pad
Between the superficial and deep layers of the temporalis fascia, a small amount of fat is encompassed: the superficial temporal fat pad (Fig. 2.9). This fat pad has been referred to as being part of the buccal fat pad (Tideman et al. 1986). In his detailed work, Stuzin et al. (1989, 1990) revealed that the superficial temporal fat pad is a distinct entity to the buccal fat pad that has no continuation with it, such as the masticatory space, differs in appearance, and has a different vascularization as it is supplied by the middle temporal artery. The middle temporal artery, the zygomaticoorbital artery, and the zygomaticotemporal nerve are running within the superficial temporal fat pad.
2.2.4.2 Deep Temporal Fat Pad
Another thin fat pad, the deep temporal fat pad, exists at a deeper plane, between the temporalis fascia and the outer surface of the temporalis muscle (Fig. 2.9). It covers the inferior portion of the temporalis muscle, starting at a level 2–4 cm above the arch; continues beneath the arch, also covering the muscle tendon; and becomes continuous with the buccal fat pad (Stuzin et al. 1989).
2.2.5 Temporalis Muscle
Under the temporalis fascia, the temporalis muscle is found (Figs. 2.9 and 2.12). The temporalis muscle is a fan-shaped muscle that belongs to the masticatory muscle group and fills the entire temporal fossa. Its fibers arise from the whole vicinity of the temporal fossa up to the inferior temporal line and the deep surface of its fascia (temporalis fascia). Anteriorly they are oriented in a vertical manner and become more oblique when getting posteriorly. Coming from the periphery, the fibers converge and form the temporalis muscle tendon. The tendon passes between the zygomatic arch and the side of the skull and attaches firmly to the coronoid process of the mandible and to the anterior border of the mandibular ramus as far as the third molar.
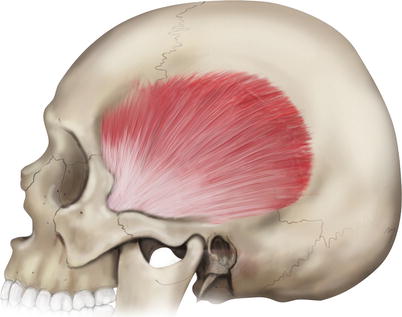
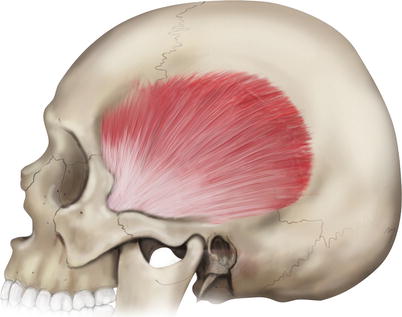
Fig. 2.12
Temporalis muscle
The temporal muscle is supplied by the deep temporal branches of the maxillary artery and is innervated by the deep temporal branches of the mandibular nerve. The temporalis closes the mouth by elevating the mandible.
2.2.6 Pericranium
The scalp pericranium extends laterally at the temporal area. At the superior temporal line, it fuses with the temporalis fascia and continues below the temporalis muscle covering the bones of the temporal fossa (Fig. 2.9). It is vascularized mainly from perforating branches of the superficial and deep temporal arteries with contribution from intracranial vessels that perforate and supply the underlying calvarial bone.
2.3 Superficial Anatomy of Posterior Neck
In the design of a scalp flap, the skin from the posterior neck might sometimes need to be incorporated. Usually this is raised and transferred to the recipient site together with a scalp flap that is derived from the occipital region.
The anatomy of the posterior neck that concerns the elevation of a cutaneous flap encompasses the skin and the subcutaneous tissue, the fasciae, and the muscles encountered in the superficial level.
2.3.1 Skin and Subcutaneous Tissue
The skin and subcutaneous tissue layer of the posterior cervical region is thicker than the corresponding layer of the anterior neck but thinner than that of the back of the torso. The presence of hair, as an extension from the hair-bearing occipital scalp to the nuchal region, depends on gender and race and also varies from one individual to the other. The relaxed skin tension lines are almost horizontally oriented like the ones of the posterior scalp (Fig. 2.13).


Fig. 2.13
Relaxed skin tension lines (RSTLs) at the posterior neck and posterior scalp
2.3.2 Deep Cervical Fascia
Just beneath the skin and subcutaneous tissue, the investing layer and the prevertebral layer of the deep cervical fascia are encountered (Fig. 2.14). The investing layer of the deep cervical fascia appears at the nape of the neck as a thin fascia that running from its bone attachments envelopes first the trapezius and then the sternocleidomastoid muscle in each side, as it passes anteriorly to encircle the whole neck (see Chap. 8). Superiorly, along the superior nuchal line, it fuses with the periosteum of the occipital bone. The prevertebral layer of the deep cervical fascia lies beneath the previous one and is encountered at the gap between the sternocleidomastoid and trapezius muscles covering the splenius capitis and the semispinalis capitis muscles. Τhe investing and the prevertebral layers of the deep cervical fascia and the tendinous origin of the upper muscle fibers of the trapezius all fuse together at the midline.
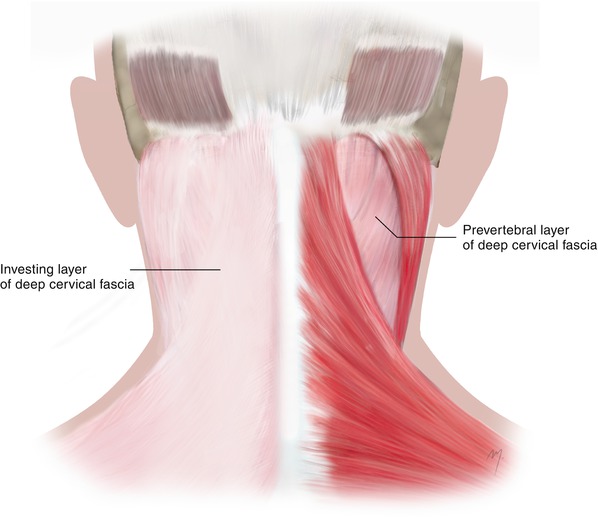
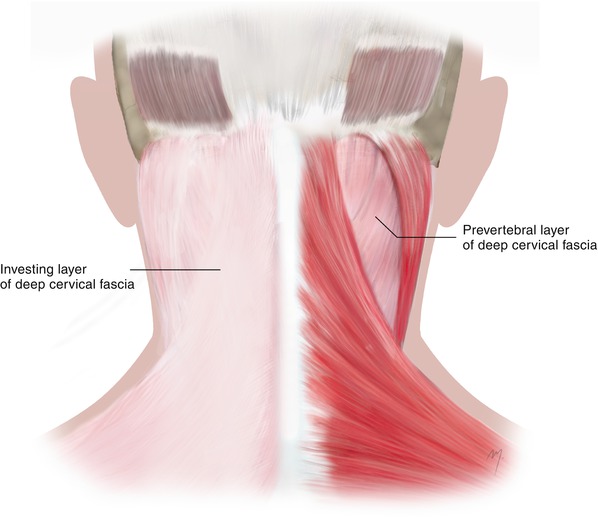
Fig. 2.14
The layers of the deep cervical fascia at the posterior neck. The investing layer lies superficial and encircles the whole neck (left side). When the investing layer is removed (right side), the deeper prevertebral layer is encountered at the gap between the sternocleidomastoid and the trapezius muscles
2.3.3 Superficial Muscles
The surface muscles that are encountered at the nape of the neck just under the skin and the deep cervical fascia are the trapezius, the splenius capitis, and the semispinalis capitis (Fig. 2.15). These muscles are arranged in three layers, each of them being under the other.
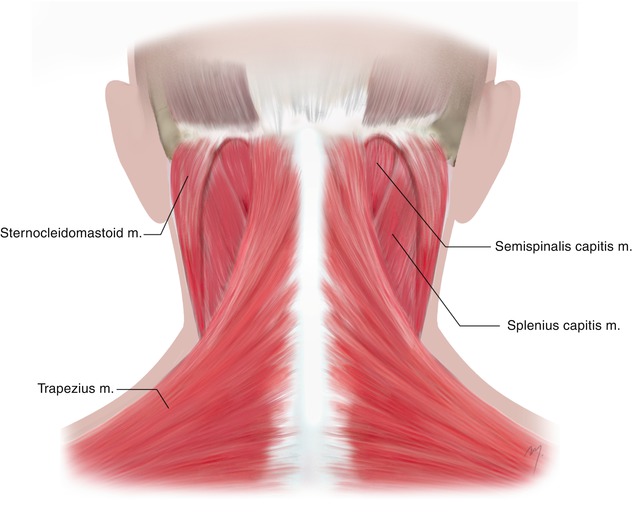
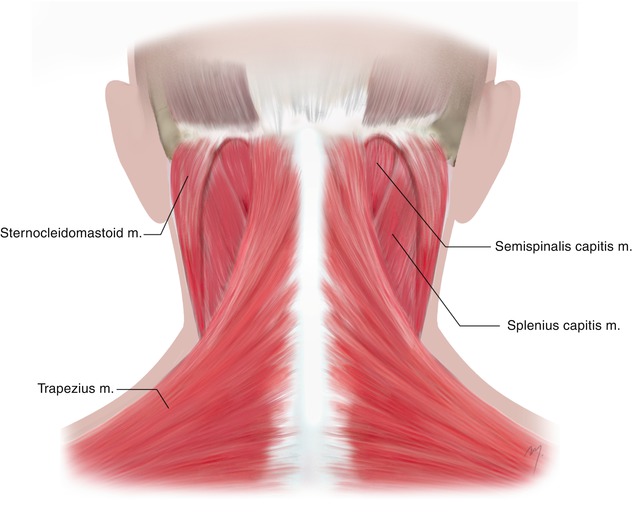
Fig. 2.15
Superficial muscles of the posterior neck
2.3.3.1 Trapezius Muscle
The trapezius muscle is an extended muscle of the upper limb that extends over the nape of the neck and the upper thorax. Its shape is triangular, with the upper angle corresponding to the external occipital protuberance, the lower angle to the spinous process of the twelfth thoracic vertebra, and the lateral angle to the acromion. The paired triangular muscles form a wide trapezium, from which the name is derived.
The muscle is subdivided in an upper, a middle, and a lower part according not only to the topography but also to the different muscle fibers’ direction. The upper muscle part is the part of interest in the nape of the neck.
2.3.3.1.1 Upper Part of the Trapezius Muscle
The muscle fibers of the upper part arise from the medial third of the superior nuchal line, the external occipital protuberance, and the nuchal ligament. The attachment of this part is by an adherent to the skin, thin aponeurotic fibrous lamina, which is also continuous with the aponeurosis at the insertion of the sternocleidomastoid muscle. The occipital artery and the greater occipital nerve pierce this fibrous lamina. The muscle fibers of the upper part of the trapezius muscle descend to meet the horizontally running fibers of the middle muscle part and the ascending lower fibers as they all converge laterally to the shoulder. The fibers of the upper part of the trapezius are attached to the posterior border of the lateral third of the clavicle and the scapula. This part of the trapezius muscle is vascularized by the transverse muscular branch of the occipital artery (contributed by branches of the ascending superficial cervical artery) and is innervated by branches of the accessory nerve. The upper part of the trapezius elevates the scapula, and with the scapula steady, it bends the head backward and laterally.
2.3.3.2 Splenius Capitis Muscle
Splenius capitis lies deep to the trapezius muscle and its upper part beneath the sternocleidomastoid muscle. It fills the gap between the sternocleidomastoid and trapezius, forming the upper part of the floor of the posterior triangle of the neck. It completely covers the longissimus capitis and almost all of the semispinalis capitis, except a small triangle of its upper part, just suboccipital.
The muscle fibers of the splenius capitis arise from the lower half of the nuchal ligament and the spinous processes of the 7th cervical and 1st, 2nd, 3rd, and 4th thoracic vertebrae. The fibers run upward and laterally under the trapezius and the sternocleidomastoid. They insert to the mastoid process and just below the lateral third of the superior nuchal line. The descending branches of the occipital artery supply the upper portion of the splenius capitis muscle. The lateral branches of the dorsal rami of the middle cervical spinal nerves innervate the muscle. The splenius capitis acts as synergist with the contralateral sternocleidomastoid. When it acts bilaterally, it draws the head backward and extends the neck.
2.3.3.3 Semispinalis Capitis Muscle
The semispinalis capitis lies under the splenius capitis muscle and belongs to the transversospinalis muscle system of the deep muscles of the back. It arises by the tendons from the articular processes of the lower (4th, 5th, 6th) cervical vertebrae and from the transverse processes of the last cervical (7th) and the half of the thoracic vertebrae (1st–6th). The muscle fibers run upward and insert to the middle part of the area between the superior and inferior nuchal lines. A small triangular area in the upper part of the muscle, between the trapezius and the splenius capitis, lies under the skin. This triangular part constitutes the floor of the apex of the posterior triangle of the neck. The descending branches of the occipital artery supply the upper part of the muscle. The semispinalis capitis is innervated by the dorsal rami of the cervical and thoracic spinal nerves. The semispinalis capitis extends the head turning the face slightly to the contralateral site. When acting bilaterally, they extend the head and the neck.
2.4 Vascular Anatomy
2.4.1 Arterial Anatomy of the Scalp and Temple
The vascular system of the scalp mainly consists of the superficial temporal, posterior auricular, and occipital arteries that are branched from the external carotid artery. The internal carotid system that provides the majority of blood supply to the forehead (through the supraorbital and supratrochlear arteries) supplies the anterior part of the scalp by the terminal parts of these vessels. Bone perforators of the meningeal arteries provide a small contribution to the scalp blood supply.
The major scalp arteries run within and on the surface of the musculoaponeurotic layer. They give branches directly to the above subcutaneous layer that form the subcutaneous vascular plexus and branches to the deeper loose areolar tissue layer.
2.4.1.1 Terminal Parts of the Supraorbital Artery and Supratrochlear Artery
The terminal part of the superficial branch of the supratrochlear artery as it ascends turns slightly toward the midline, where it reaches the frontal portion of the scalp, traveling in the subcutaneous level. Some of the sub-branches of the superficial branch of the supraorbital artery, as they travel lateral to the supratrochlear artery in a same plane, may sometimes reach and contribute to the vascular supply of the frontal scalp. However, both arteries perfuse significantly the vascular plexus of the frontal scalp and must be taken into account during scalp flap design (Fig. 2.16).
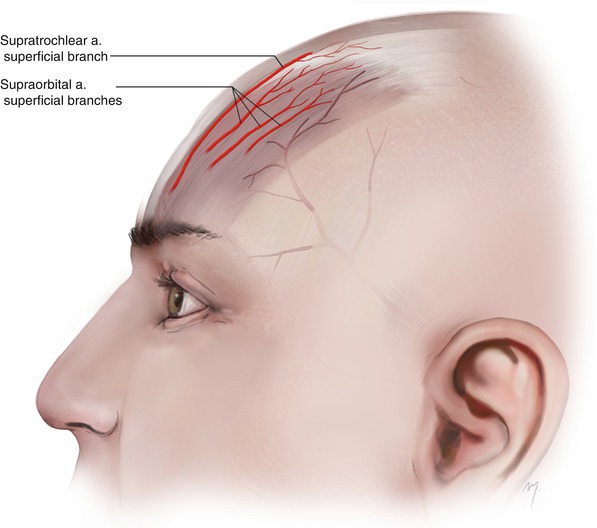
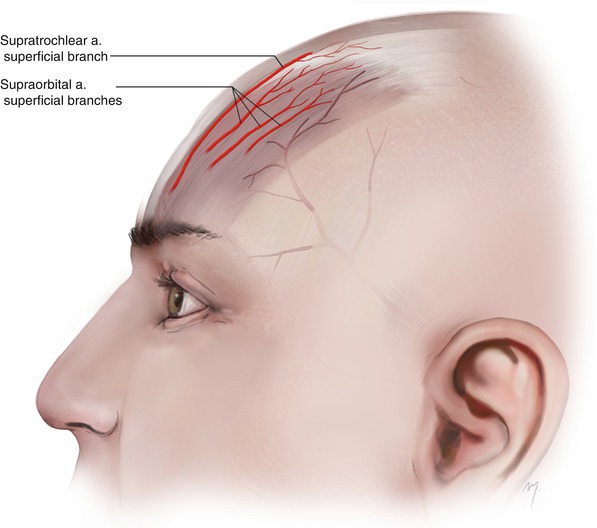
Fig. 2.16
The terminal parts of the supraorbital and supratrochlear arteries contribute to the vascular supply of the most anterior part of the scalp
2.4.1.2 Superficial Temporal Artery at the Scalp
The course of the superficial temporal artery at the scalp is the part of its course over the zygomatic arch (Fig. 2.17). As the artery comes from the preauricular region, it is found passing over the posterior root of the zygomatic process. The artery runs within the temporoparietal fascia, and as it continues branching, it becomes more superficial and runs over the surface of the fascia. It runs upward giving off some branches and finally bifurcates into the frontal (anterior) and parietal (posterior) final branches. The bifurcation of the superficial temporal artery into its terminal frontal and parietal branches occurs above the zygomatic arch in the majority of the individuals (60–88 %). Bifurcation at the level of the arch has been reported to range between 4 and 26 %, whereas bifurcation below the arch ranges between 8 and 11 % of individuals (Stock et al. 1980; Marano et al. 1985; Abul-Hassan et al. 1986; Czerwinski 1992; Nakajima et al. 1995; Chen et al. 1999; Pinar and Govsa 2006; Tayfur et al. 2010). Rarely, in approximately 3.7 % of cases, the artery does not bifurcate and courses only as a frontal branch, and the parietal branch is absent (Pinar and Govsa 2006).
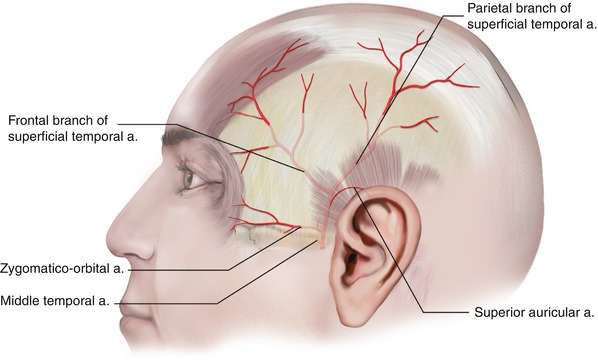
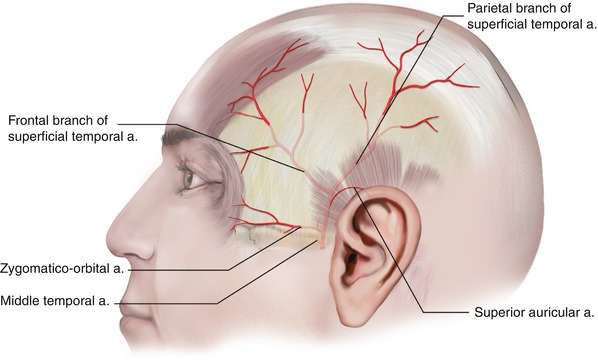
Fig. 2.17
The superficial temporal artery at the temple and its branches
When the bifurcation of the superficial temporal artery occurs above the zygomatic arch, it happens at a point within 2–4 cm above the arch. At the branching point, the diameter of the artery is approximately 1.8–2.7 mm (Stock et al. 1980; Marano et al. 1985; Abul-Hassan et al. 1986; Chen et al. 1999; Pinar and Govsa 2006).
2.4.1.2.1 Branches of the Superficial Temporal Artery at the Temple
The superficial temporal artery, after branching the transverse facial artery to the cheek (see Chap. 5), gives off the rest of its branches over the zygomatic arch at the temporal region (Fig. 2.17).
1.
Middle Temporal
The middle temporal artery arises usually at the superior border of the zygomatic arch or alternatively 1–2 cm below its upper border. It pierces the superficial layer of the temporalis fascia immediately above its attachment to the zygomatic arch, enters the superficial fat pad, and then pierces the deep layer of the temporalis fascia. It runs along the undersurface of the temporalis fascia and finally anastomoses with the deep temporal arteries (branches of the maxillary artery). The middle temporal artery supplies the superficial fat pad and contributes to the supply of the temporalis muscle.
2.
Zygomaticoorbital Artery
The zygomaticoorbital artery arises immediately after the middle temporal artery and runs forward to the lateral orbit, along and close to the upper border of the zygomatic arch within the superficial temporal fat pad. It anastomoses with the palpebral and lacrimal branches of the ophthalmic artery. Sometimes it arises not from the main stem of the superficial temporal artery but from its frontal branch. During its course it gives off cutaneous branches that supply the overlying skin.
In about 20 % of the individuals, the zygomaticoorbital artery may be absent and the supply of the lateral orbital region is taken off from the transverse facial artery and by small sub-branches of the superficial temporal artery (Pinar and Govsa 2006).
3.
Superior Auricular Artery
The superficial temporal artery at its temporal course gives rise to the superior auricular branch a small artery that contributes to the supply of the auricle (see Chap. 7).
4.
Frontal Branch of the Superficial Temporal Artery
The frontal branch of the superficial temporal artery after originating from the bifurcation of the superficial temporal artery runs tortuously upward and forward giving off ascending and descending branches at the temporal area. It has been reported that the diameter of the frontal branch of the superficial temporal artery measured at the level of bifurcation has a mean range between 1.6 and 2.1 mm (Stock et al. 1980; Lang 1995; Chen et al. 1999; Pinar and Govsa 2006; Edizer et al. 2009; Tayfur et al. 2010). Its length is approximately 11 cm (Tayfur et al. 2010). Reaching the forehead it usually gives off a transverse branch, as the main continuation ascends superomedially. It travels superficial to the frontalis muscle becoming shallow up to the subdermal level as it approaches the midline.
The frontal branch of the superficial temporal artery supplies all the layers of the frontal scalp and constitutes the main vascular supply for the temporal subunits of the forehead. The artery is easily palpable in the temple and can be easily mapped in cases where it needs to be incorporated into the flap.
5.
Parietal Branch of the Superficial Temporal Artery
The parietal branch of the superficial temporal artery after originating from the bifurcation of the superficial temporal artery runs on the side of the head curving slightly upward and backward. At the starting point, its diameter ranges between 1.6 and 1.8 mm (Stock et al. 1980; Lang 1995; Chen et al. 1999; Pinar and Govsa 2006; Tayfur et al. 2010). It lies initially within the temporoparietal fascia becoming more superficial and finally runs on the external surface of the galea. At a level 10–14 cm above the zygomatic arch, it becomes even more superficial and runs through the subcutaneous tissue layer (Tremolada et al. 1994).
Although the exact course of the temporal artery branches must be determined by Doppler examination, what follows is a useful landmark in regards to the position of the parietal branch that is quite accurate. The course of the parietal branch in continuity with the superficial temporal artery is presented within a vertical zone that starts 1 cm in front of the tragus and widens posteriorly for 4 cm (Fig. 2.18). Within this zone, the superficial temporal artery ascends almost vertically in front of the auricle, and after its bifurcation, the parietal branch continues curving up to the vertex. This constitutes a useful landmark in flap design when the parietal branch in continuity with the superficial temporal artery is to be caught in a scalp flap.
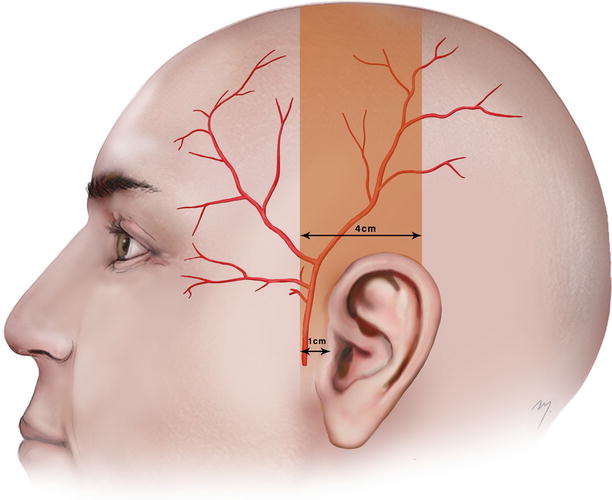
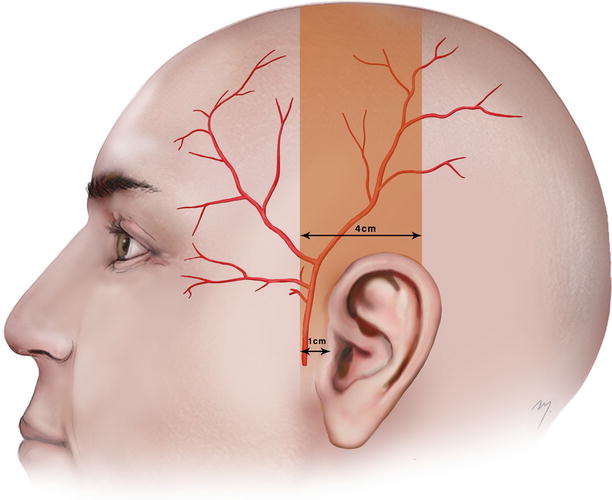
Fig. 2.18
The parietal branch in continuity with the superficial temporal artery runs within a vertical zone that starts 1 cm in front of the tragus and extends for 4 cm posteriorly
2.4.1.3 Posterior Auricular Artery
The posterior auricular artery is a small branch that arises from the posterior aspect of the external carotid artery above the digastric and stylohyoid muscles. It goes up between the parotid gland and the styloid process to the groove between the auricle and mastoid process. It gives off small neck branches (see Chap. 8) and at the level of the external auditory meatus pierces the deep fascia and divides into an auricular and occipital branch (Fig. 2.19).
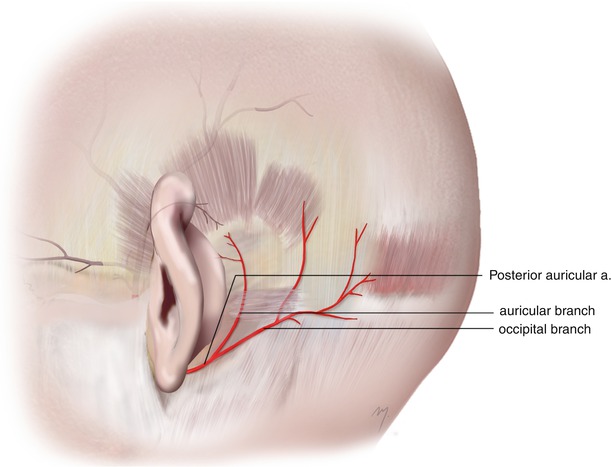
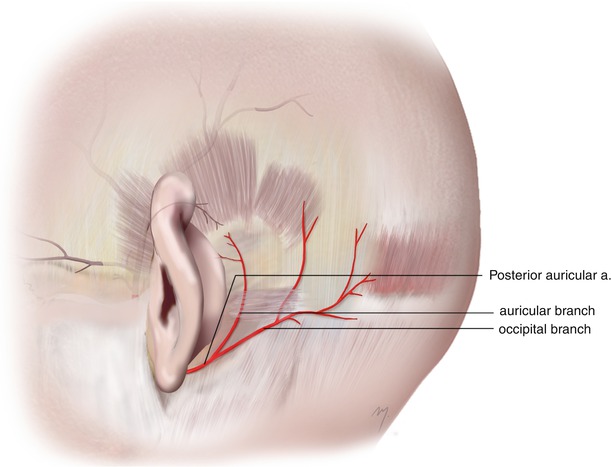
Fig. 2.19
Posterior auricular artery and its auricular and occipital branches
2.4.1.3.1 Auricular Branch
The auricular branch ascends under the posterior auricular muscle. It gives off small branches that supply the skin of the posterior aspect of the ear and branches that pierce the cartilage reaching the skin over the external surface of the ear (see Chap. 7). It anastomoses with the superior auricular artery, a branch of the superficial temporal artery.
2.4.1.3.2 Occipital Branch
The occipital branch runs laterally, across the mastoid process, over the insertion of the sternocleidomastoid muscle terminating over the occipitalis muscle. It supplies the posterolateral scalp.
2.4.1.4 Occipital Artery
The occipital artery arises from the posterior aspect of the external carotid artery about 2 cm from its origin and opposite to the origin of the facial artery. Its diameter is about 3 mm in its origin. At first it runs up- and backward, lying deep to the posterior belly of the digastric muscle. It crosses from the front the internal carotid artery, the internal jugular vein, the vagus, the hypoglossal, and the accessory nerves. Running in the occipital groove of the temporal bone and passing the medial aspect of the mastoid process, it reaches the occipital area. Here, it lies deep to the attachments of the sternocleidomastoid, splenius capitis, and longissimus capitis muscles.
In its final part, as it passes medially, it lies on to the semispinalis capitis muscle. It turns upward and 3.5–4.0 cm from the midline; the artery emerges through the attachments of the trapezius and sternocleidomastoid muscle (Fig. 2.20). After piercing the deep cervical fascia between the trapezius and sternocleidomastoid muscles, it ascends tortuously at the occipital area and divides into its terminal occipital branches.
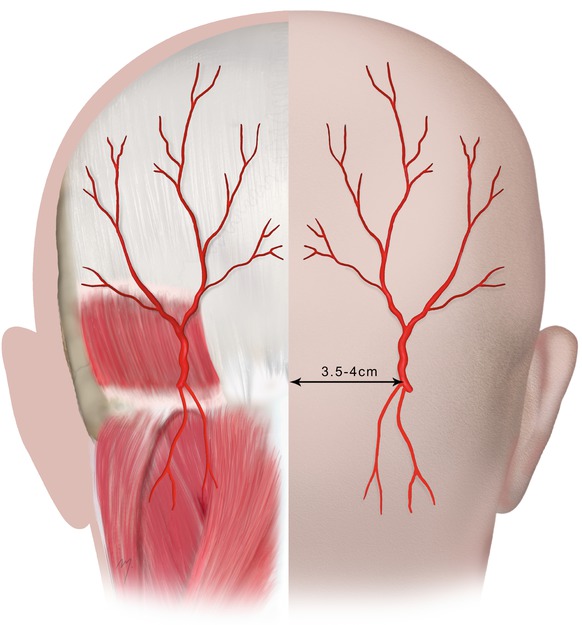
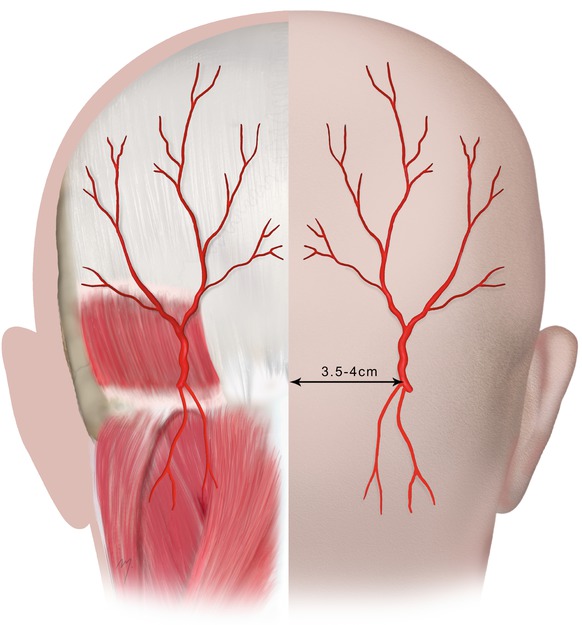
Fig. 2.20
Occipital artery. Distribution of the occipital branches to the posterior scalp and the distance of emerging point from midline
2.4.1.4.1 Branches
The occipital artery during its long course gives off a great number of branches: meningeal branches that enter the skull through the jugular foramen; a small mastoid branch that supplies the mastoid antrum; the stylomastoid artery, which enters the stylomastoid foramen and supplies the facial nerve; and the tympanic cavity and the mastoid antrum, muscular branches that supply the digastric, stylohyoid, longissimus capitis, trapezoid, and splenius muscles.
The occipital artery gives off branches that through cutaneous or musculocutaneous perforators supply also the skin: The lower and the upper sternocleidomastoid branches supply the upper part of the sternocleidomastoid muscle and the overlying neck skin (see Chap. 8). The descending branch, the transverse muscular branch for the trapezius muscle, and the cutaneous cervical branches contribute to the supply of the skin of the nape of the neck.
The occipital artery, just after emerging from the cranial attachments of the trapezius and sternocleidomastoid muscle, appears at the posterior scalp. It ascends tortuously over the occipitalis muscle and the galea within the dense subcutaneous tissue of the scalp and divides very quickly in its terminal occipital branches. The terminal occipital branches distribute to the posterior scalp running tortuously as high as the vertex constituting the major arterial system of the posterior scalp. Many of the terminal branches run in company with branches of the greater occipital nerve often having a straight anatomic intersection, or they can be intertwined in a helical form. The final part of the occipital artery and its terminal occipital branches supply the posterior scalp and the pericranium.
2.4.2 Vascularization of the Skin of the Posterior Neck
A major, direct cutaneous arterial vessel that supplies the posterior cervical skin does not exist. Musculocutaneous perforators are branched from the deep arteries and pierce the posterior neck muscles reaching the overlying skin. Minimum exception to this is the few direct small cutaneous branches coming from the occipital artery. The most important perforators come from branches of the occipital artery and the superficial cervical arteries (Fig. 2.21).
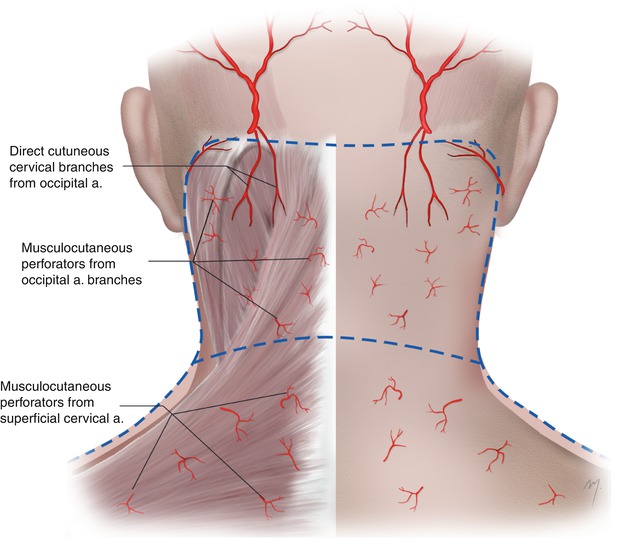
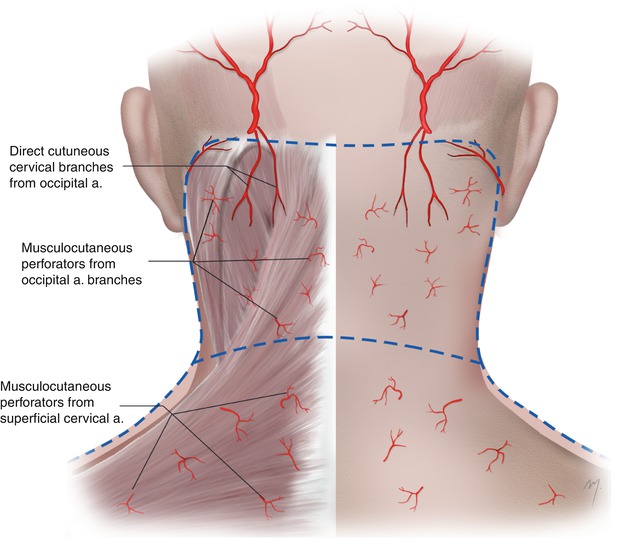
Fig. 2.21
The upper part of the skin of the nape of the neck is supplied by direct cutaneous and musculocutaneous perforators coming from branches of the occipital artery and the lower part by musculocutaneous perforators from the superficial cervical artery
2.4.2.1 Branches of the Occipital Artery That Contribute to the Vascularization of the Skin of the Posterior Neck
1.
The upper sternocleidomastoid branches give rise to perforators that are distributed to the skin of the upper lateral part of the nuchal region.
2.




The transverse trapezius branch that arises at the level of the mastoid process reaches the upper portion of the trapezius in its deep surface. It then pierces the muscle giving off multiple small perforating vessels to the overlying skin (Standring 2008).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








