(1)
Department of Anatomy, Medical School Democritus University of Thrace, Alexandroupolis, Evros, Greece
Abstract
The deltopectoral region constitutes the donor site of mainly two classic and widely used in head-neck reconstruction regional fasciocutaneous flaps: the cervicopectoral and the deltopectoral flaps. The anatomy relevant in the surgery of these flaps involves in layered arrangement the superficial fascia, the pectoral-deltoid fascia, and the pectoralis major and deltoid muscles. The skin of the deltopectoral region is supplied by branches of the acromiothoracic, internal thoracic, and lateral thoracic and by the supraclavicular arteries. The deltopectoral flap is a transposition flap that transfers skin from the deltoid region. The flap is of axial pattern, based on the internal thoracic artery perforators, in its medial part and of random pattern in its lateral part. The cervicopectoral flap is a large rotation flap best used in the reconstruction of large lateral facial defects. The flap is of axial pattern, based on the internal thoracic artery perforators, in its thoracic part and of random pattern in the rest of it.
9.1 Layered Anatomy
The pectoral and the deltoid regions constitute the donor sites of mainly two very popular regional fasciocutaneous flaps that are used in head-neck reconstruction: the cervicopectoral and the deltopectoral flaps. The anatomy relevant in the surgery of these flaps includes in layered arrangement the superficial fascia, the pectoral-deltoid fascia, and the pectoralis major and deltoid muscles.
9.1.1 Superficial Fascia in the Anterior Chest Wall
The superficial fascia in the anterior chest wall consists of loose areolar connective and adipose tissue and is loosely connected to the skin. Depending on gender and ethnicity, the superficial fascia may consist of more than one membranous sheet of varying thickness and variable amount of fat (Abu-Hijleh et al. 2006). The superficial fascia is perforated by small blood vessels and nerves that supply the skin. It is continuous with the SMAS layer at the neck and with the corresponding layer of the upper limb (and hence the deltoid region) superiorly and with that of the abdomen inferiorly. In the chest, it encompasses the mammary gland, giving off septa that pass between its lobes.
9.1.2 Pectoral and Deltoid Fascia
The pectoral fascia (Fig. 9.1) is a fibroelastic sheath that covers the pectoralis major muscle and corresponds to the deep cervical fascia. It is thin (mean thickness of 297 μm) and is thicker in the inferior thorax and thinner in the subclavicular region (Stecco et al. 2009a, b). It is connected to the pectoralis muscle through multiple intramuscular septa that are detached from its inner surface. The pectoral fascia superiorly is fused with the clavicle and the coracoid process and inferiorly is continuous with the ipsilateral and contralateral rectus abdominis sheaths. It consists of two layers: a superficial layer and a deep one. The superficial layer is thin and covers the outer surface of the pectoralis major muscle also separating the muscle from the mammary gland. The superficial layer crosses over the sternum and continues with the superficial layer of the contralateral pectoral fascia, whereas the deep layer covers the inner surface of the pectoralis major muscle and fuses with the sternal periosteum. The deep layer of the pectoral fascia forms the clavipectoral and the axillary fasciae.
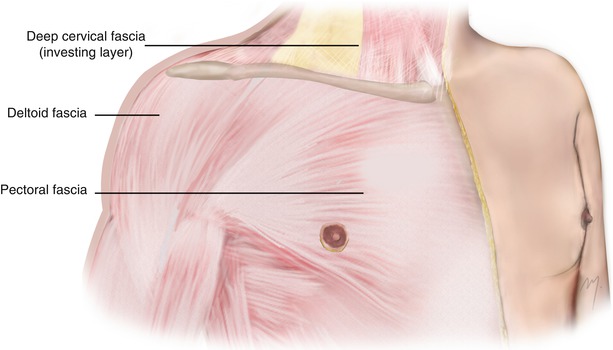
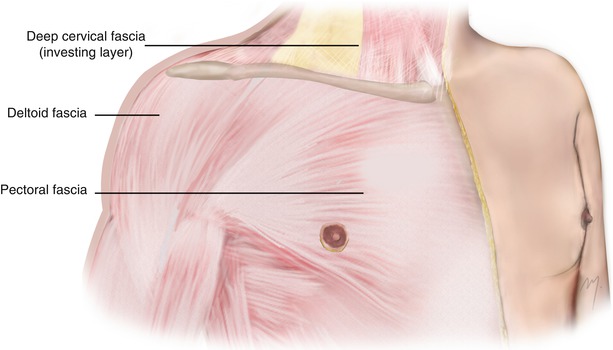
Fig. 9.1
Pectoral and deltoid fascia
The deltoid fascia is a fibrous membrane that overlies the deltoid muscle. Like the pectoral fascia, it sends intramuscular septa into the deltoid muscle. Superiorly it is attached to the clavicle, the acromion, and the spinal crest of the scapula; inferiorly it is continuous with the brachial fascia, medially with the pectoral fascia, and posteriorly with the infraspinous fascia (Standring 2008).
9.1.3 Pectoralis Major Muscle
The pectoralis major muscle (Fig. 9.2) is a triangular-shaped muscle that occupies the major part of the chest. It is separated from the deltoid muscle by a groove termed the deltopectoral groove. The deltopectoral groove transitions upward to the infraclavicular fossa (deltopectoral triangle) that can be seen as a small depression inferior to the clavicle. The cephalic vein runs in the deltopectoral groove and ascends deeply in the infraclavicular fossa where it pierces the clavipectoral fascia to join the axillary vein. The infraclavicular fossa contains furthermore the deltoid branch of the acromiothoracic artery.
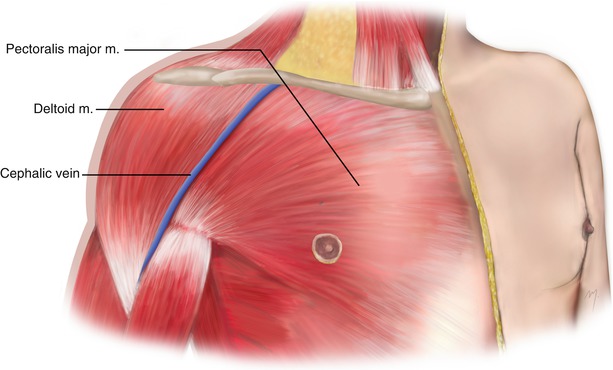
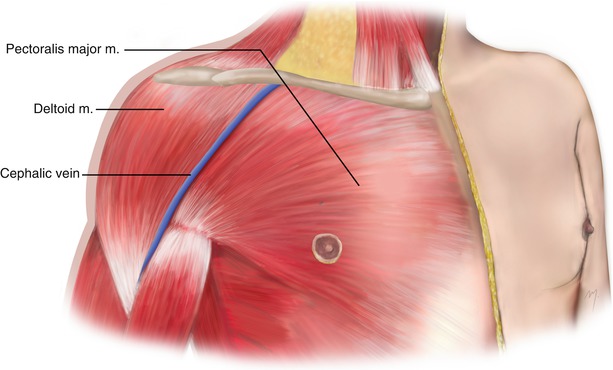
Fig. 9.2
Pectoralis major and deltoid muscles
The pectoralis major muscle arises from the anterior surface of the medial half of the clavicle; from the half of the breadth of the anterior surface of the sternum, down to the level of the attachments of the sixth or seventh costal cartilage; from the cartilages of the first to seventh ribs; from the sternal end of the sixth rib; and from the aponeurosis of the external oblique muscle. According to the muscle fibers’ origin, the pectoralis major exhibits a clavicular and a sternocostal part that are separated by a slight cleft. All of its muscle fibers run horizontally to converge to a tendon approximately 5 cm across. The upper muscle fibers descend obliquely and laterally, the middle fibers run horizontally and laterally, and the lower fibers ascend obliquely and laterally. The tendon that is formed from the converging muscle fibers of the pectoralis major is bilaminar in form (with an anterior and a posterior lamina) and is attached to the lateral lip of the intertubercular sulcus of the humerus.
The pectoralis major is supplied by a primary arterial pedicle from the pectoral branch of the thoracoacromial artery. The pectoralis major musculocutaneous flap is based on this primary arterial pedicle from the thoracoacromial artery. The perforating branches of the internal thoracic artery and the lateral thoracic artery complete the vascular pedicles of the muscle.
Multiple smaller muscular vessels arising from the deltoid and clavicular branches of the thoracoacromial artery and the superior thoracic artery contribute to the supply of the most upper and lateral clavicular portion of the pectoralis major. It has been reported (Yang et al. 2003) that the pectoralis major muscle and the overlying skin are supplied in approximately 50.7 % by the pectoral branch, in 43 % by the perforating branches of the internal thoracic artery, and in the 6.6 % by the lateral thoracic artery. The pectoralis major musculocutaneous flap traditionally is based only to the pectoral branch of the thoracoacromial artery. Newly improved techniques of harvesting the pectoralis major myocutaneous flap preserve the lateral thoracic artery enhancing thus the vascularity of the distal skin island (Po-Wing Yuen 2006). The muscle is innervated from the medial and lateral pectoral nerves that are branches of the brachial plexus.
The pectoralis major muscle when both of its parts act adducts the humerus at the shoulder and rotates the humerus medially. It also draws the scapula anteriorly and inferiorly. Acting alone its clavicular part flexes the humerus at the shoulder and its sternocostal part extends it.
9.1.4 Deltoid Muscle
The deltoid muscle (Fig. 9.2) is one of the scapular muscles that surround the shoulder joint. It is a thick muscle, having a shape of an inverted Greek letter “delta.”
The deltoid muscle originates from the anterior border and the superior surface of the lateral third of the clavicle, the lateral margin and the superior surface of the acromion, and the lower edge of the crest of the spine of the scapula. The muscle fibers descend forming the smooth contour of the shoulder and converge to form a short tendon. The tendon formed by the converging muscle fibers inserts to the deltoid tuberosity on the lateral aspect of the humerus. The deltoid muscle receives its blood supply from the acromial and deltoid branches of the thoracoacromial artery, the anterior and the posterior circumflex humeral arteries, the subscapular artery, and the deltoid branch of the profunda brachii. The muscle is innervated by the axillary nerve (C5, C6). When acting, the anterior muscle fibers flex and rotate the arm medially, the middle fibers abduct the arm, and the posterior fibers extend and rotate the arm laterally.
9.2 Arteries Supplying the Skin of the Deltopectoral Region
The skin of the deltopectoral region is supplied by branches of the acromiothoracic, internal thoracic, and lateral thoracic arteries and by the supraclavicular artery (Fig. 9.3).
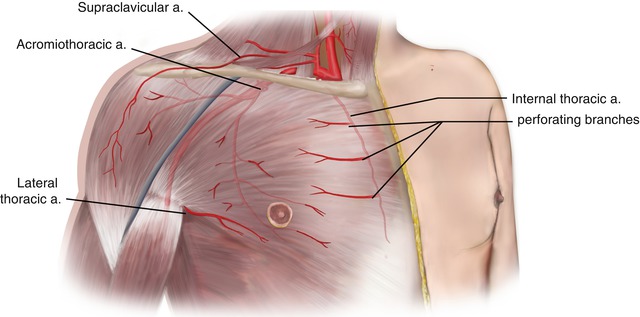
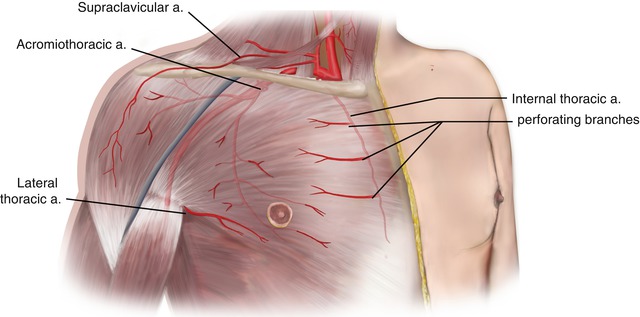
Fig. 9.3
Main arteries that supply the skin of the anterior chest and deltoid region
9.2.1 Acromiothoracic Artery
The acromiothoracic (thoracoacromial) artery is a short arterial trunk (1–1.5 cm) that arises from the anterior aspect of the second part (sometimes it arises from the first part) of the axillary artery usually 3 cm from its starting point. Its mean diameter is 2–2.5 mm. It curves around the superior margin of the tendon of the pectoralis minor muscle, pierces the clavipectoral fascia, and after its origin gives off four branches: the pectoral, the acromial, the clavicular, and the deltoid branch.
The point related to the midclavicular line where the acromiothoracic artery originates from the axillary artery differs in the left and right sides probably due to the different embryologic origins of the right and left subclavian systems (the right originated from the brachiocephalic trunk and the left from the aortic arch). In the right side, the acromiothoracic artery originates from the axillary artery in a point 2–3 cm below the clavicle and laterally to the midclavicular line, and in the left side, 2–3 cm below the clavicle and usually medial to the midclavicular line (Nakajima et al. 1997; Park et al. 2004).
9.2.1.1 Branches
9.2.1.1.1 Pectoral Branch
The pectoral branch is the largest branch of the acromiothoracic artery and the main feeding vessel of the myocutaneous pectoralis major flap. It runs inferiorly on the deep surface of the pectoralis major muscle, after giving a branch to the pectoralis minor muscle. It penetrates the pectoralis major muscle and anastomoses within the muscle mass with the branches of the perforators of the internal thoracic and the lateral thoracic arteries. The course of the pectoral branch corresponds to a line that runs from the middle of the clavicle vertically downward and then turns medially at the point where it meets a line that connects the acromion and the xiphoid process, running along this line (Ariyan 1979; Freeman et al. 1981). The pectoral branch of the acromiothoracic artery supplies more of the half of the muscle parenchyma of the pectoralis major (Yang et al. 2003). Through the musculocutaneous perforators, it also supplies the overlying chest skin. The skin area that is supplied by the pectoral branch can range from 7 × 12 cm to 24 × 30 cm in the region between the 3rd and 6th rib from the parasternal line to the anterior axillary line (Kovacević et al. 2008).
9.2.1.1.2 Clavicular Branch
The clavicular branch runs superomedially, between the clavicular part of the pectoralis major muscle and the clavipectoral fascia, and supplies the subclavius muscle.
9.2.1.1.3 Deltoid Branch
The deltoid branch crosses pectoralis minor muscle and travels within the infraclavicular fossa in company with the cephalic vein. It supplies the pectoralis major and deltoid muscles.
9.2.1.1.4 Acromial Branch
This branch crosses the coracoid process and runs initially beneath the deltoid muscle, penetrates the muscle, runs over its surface, and reaches the acromion. The deltoid and the acromial branches of the acromiothoracic artery anastomose each other, and via musculocutaneous perforators and direct cutaneous branches, they supply the skin of the anterior part of the deltoid region.
9.2.2 Internal Thoracic Artery
The internal thoracic artery (internal mammary artery) arises from the inferior surface of the first part of the subclavian artery exactly opposite to the origin of the thyrocervical trunk. Its average diameter is approximately 3 mm. It runs inferiorly inside the chest in a parasternal plane, 1–1.5 cm lateral to the border of the sternum. It ends in the sixth intercostal space, where it divides into its terminal branches: the superior epigastric artery and the musculophrenic artery. It is accompanied by 1 or 2 veins, the internal thoracic veins, which ascend and drain into the brachiocephalic vein.
The internal thoracic artery gives off thymic branches that supply the thymus; sternal branches that supply the sternum and the medial part of the transversus thoracic muscle; the mediastinal arteries, which supply the structures of the anterior mediastinum; and the pericardiophrenic artery which travels in company with the phrenic nerve and supplies the pericardium and the perforating branches.
9.2.2.1 Perforating Branches
These are direct perforating branches that pierce through the internal intercostal muscles of the upper five or six intercostal spaces in company with the anterior cutaneous branches of the corresponding intercostal nerves and one perforating vein. They next penetrate the pectoralis major muscle comprising part of its blood supply. After penetrating the muscle, they become cutaneous, curve laterally, and supply the overlying skin. The perforator in the second intercostal space is usually the largest followed by the perforator in the third intercostal space and is termed as the “principal perforator” (Palmer and Taylor 1986). The average diameter of the second perforator has been found to measure 1.6 mm while the third perforator 1.4 mm and their lengths 9.6 and 8.7 cm, respectively (Schmidt et al. 2010).
These perforating branches of the internal thoracic artery constitute the dominant blood supply of the deltopectoral flap and of the pectoral portion of the cervicopectoral flap.
9.2.3 Lateral Thoracic Artery
The lateral thoracic artery (external mammary artery) arises from the second part of the axillary artery, being its second branch. The artery descends to the side of the chest initially along the lateral (axillary) border of the pectoralis minor muscle, afterward proceeds to the undersurface of the pectoralis major, and ends at the fifth intercostals space distributed to the lateral thoracic wall, the pectoral muscles, and the breast. It gives off branches that supply the serratus anterior and pectoral muscles and branches across the axilla to supply the subscapularis muscle and the axillary lymph nodes. It anastomoses with the subscapular, intercostal, acromiothoracic (pectoral branch), and internal thoracic arteries.
The lateral thoracic artery gives off cutaneous branches that course around the lateral border of the pectoralis major muscle and supply a portion of the skin of the lateral thoracic wall and the lateral part of the breast (Standring 2008).
9.2.4 Supraclavicular Artery
An important cutaneous artery that contributes to skin supply of the deltoid region is the supraclavicular artery, a vessel that is branched from the superficial cervical/transverse cervical artery. The supraclavicular artery after arising at the medial portion of the omoclavicular (supraclavicular) triangle courses laterally. At the angle between the anterior border of the trapezius and the superior border of the clavicle, it pierces the deep cervical fascia, crosses the clavicle, and travels subcutaneously to the deltoid region. It supplies the skin of the lateral and upper part of the deltoid region, giving off branches to the pectoralis major muscle, which, after piercing the muscle, contribute also to the supply of the upper thoracic skin.
9.3 Superficial Veins
Small veins that coalesce into larger ones and drain into the anterior intercostal veins drain the anterior thoracic wall. The anterior intercostal veins which accompany the intercostal arteries are tributaries of the internal thoracic and musculophrenic veins. The veins that accompany the perforating branches of the internal thoracic artery drain directly into the internal thoracic vein. The internal thoracic vein, sometimes double, travels along the border of the sternum just medial to the internal thoracic artery and drains in turn into the brachiocephalic vein.
The lateral thoracic vein contributes to the venous drainage of the lateral chest wall and the breast. The lateral thoracic vein runs with the corresponding artery and drains into the axillary vein. The lateral thoracic vein normally is connected inferiorly with the superficial epigastric vein through the thoracoepigastric vein that runs superficially on the anterolateral aspect of the trunk (Fig. 9.4).
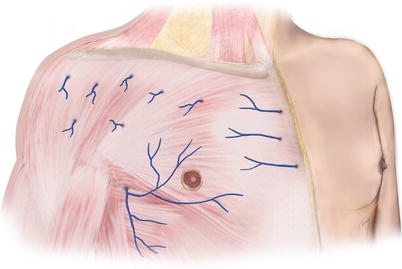
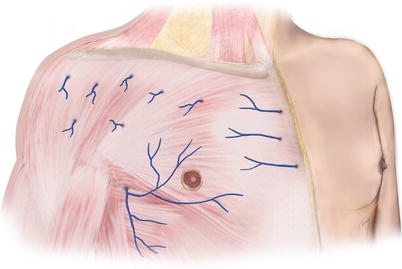
Fig. 9.4
Superficial veins of the anterior thorax
9.4 Cutaneous Nerves
The skin of the thorax receives its sensory innervation by cutaneous branches of the cervical and the thoracic nerves. The supraclavicular nerves of the cervical plexus (see Chap. 8) through their branches supply the skin of the upper thoracic region.
Particularly the medial supraclavicular branches supply the skin of the medial part of the upper thoracic region. The intermediate supraclavicular branches supply the skin of the middle and lateral part of the upper thoracic region. And the lateral supraclavicular branches distribute to the skin of the lateral part of the upper thoracic region and to the skin of the upper part of the deltoid region.
The thoracic nerves supply the skin of the anterior part of the anterior chest through their anterior cutaneous branches and the anterolateral part through the lateral cutaneous branches, respectively (Fig. 9.5).
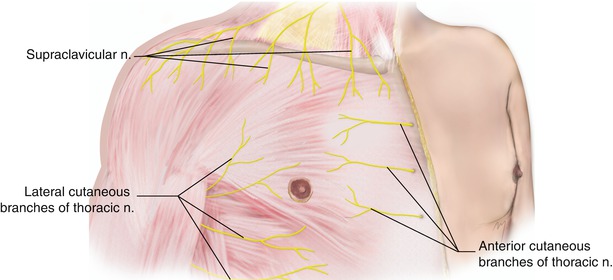
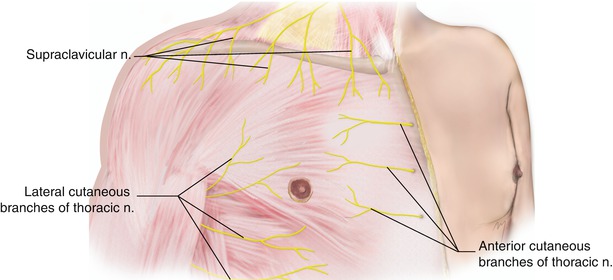
Fig. 9.5
Cutaneous nerves of the anterior thorax
9.5 Deltopectoral Flap
The deltopectoral flap is one of the two most widely used fasciocutaneous flaps in head and neck reconstruction that are derived from the deltopectoral region, the other one being the cervicopectoral flap.
The deltopectoral flap is a transposition flap that has first been designed by Aymard in 1917 for nose reconstruction. It received increased attention since 1965, when Bakamjian began using the flap for pharyngoesophageal reconstruction. The deltopectoral flap transfers the skin from the deltoid and thoracic region and shows similarities to the thoracic part of the cervicopectoral flap in terms of anatomy, vascularity, and surgical technique. The flap is of axial pattern, based on the internal thoracic artery perforators, in its medial part and of random pattern in its lateral part.
The deltopectoral flap had lost its popularity and was deported by the free vascularized flaps but recently has been reappearing in the international literature (Feng et al. 2006; Sharma and Panda 2006; Bey et al. 2009; Rebelo et al. 2009; Krijgh and Mureau 2012; Nayak and Nilamani 2012).
9.5.1 Flap Design
The deltopectoral flap is designed in rectangular shape, in the upper thorax extending from the sternum in a variable degree to the anterior deltoid region. The base of the flap is situated parasternally 2 cm from the sternal edge. The superior boundary follows the clavicle, and the inferior boundary is parallel to the previous line over the 3rd or 4th intercostal space. The flap extends horizontally beyond the deltopectoral groove onto the deltoid region, in an extent depending on the needed length to reach the defect, and ends in a curvilinear distal margin (Figs. 9.6 and 9.7).
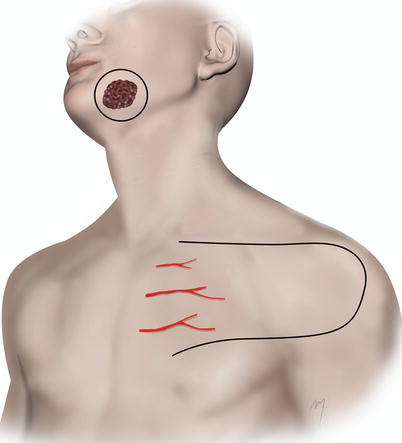

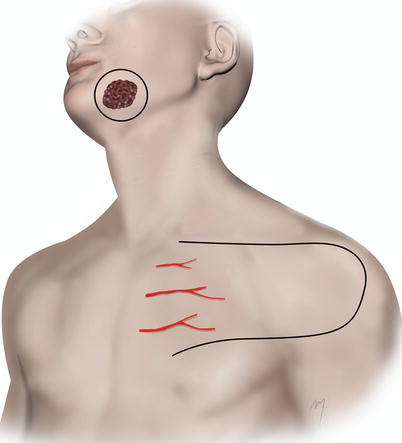
Fig. 9.6
Outline of the deltopectoral flap. The flap is of axial pattern in its medial part and of random pattern in its lateral part

Fig. 9.7
Tumor resection margins and flap are outlined
There are cases where to reach the defect the needed length of the flap compels it to extend to the lateral deltoid region and a flap delay is required at least 1 week prior to the flap harvest.
9.5.2 Flap Vascularity
The deltopectoral receives its blood supply from the perforating vessels of the internal mammary artery with the main contribution of the 2nd and 3rd perforators in its medial part having an axial blood supply at this part (Fig. 9.6). The distal part is of random pattern, so far as the musculocutaneous perforators of the deltoid and acromial branches of the acromiothoracic artery are cut during flap elevation.
9.5.3 Flap Elevation
The incision is made deep to the deltoid fascia at the deltoid region and deep to the pectoral fascia at the chest (Fig. 9.8




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








