(1)
Department of Anatomy, Medical School Democritus University of Thrace, Alexandroupolis, Evros, Greece
Abstract
The cheek constitutes the face’s largest anatomic and aesthetic unit. The soft tissues and the fasciae of the cheek are arranged concentrically over its bony skeleton. From an anatomic and surgical point of view, these structures are layered as follows: skin, subcutaneous tissue, musculoaponeurotic layer (SMAS-mimic muscles), parotidomasseteric fascia, buccal space and contents, deep muscular layer, and retaining ligaments. Surgically important nerves and vessels travel through these layers often changing planes. All types of local flaps can be derived from the cheeks providing a wide range of restoration options. Random pattern advancement, transposition, and rotation flaps work well in this region and are used to reconstruct primarily the cheek itself, but also the nearby nose, lips, and lower lid.
The cheek is a convex area of either side of the face constituting the face’s largest anatomic and aesthetic constituent. It is bounded superiorly by the zygomatic arch and the orbital-cheek crease, inferiorly by the lower border of the mandible, laterally by the preauricular crease, and medially, from up to down, by the nasofacial sulcus, the nasolabial crease, and the labiomandibular creases (Fig. 5.1).
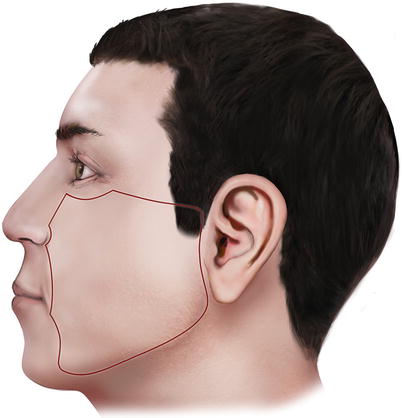
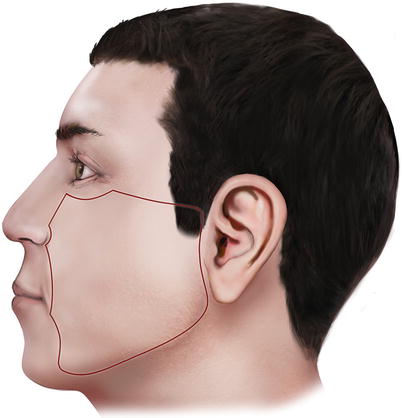
Fig. 5.1
The boundaries of the cheek
According to the morphologic-anatomic differences of the bony foundation and the soft tissue covering it, the cheek can be further subdivided into infraorbital, zygomatic, nasolabial, buccal, and parotidomasseteric subunits (Fig. 5.2).
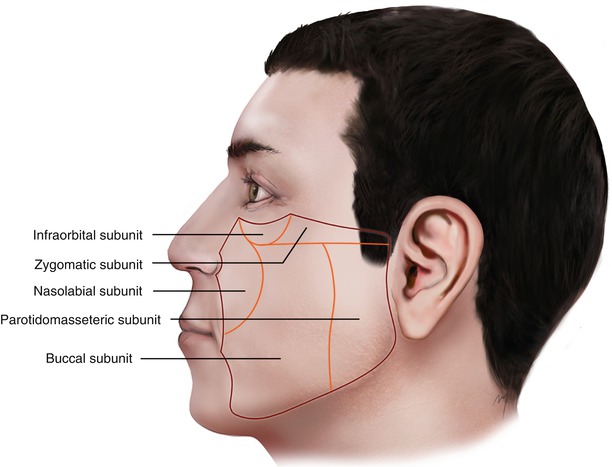
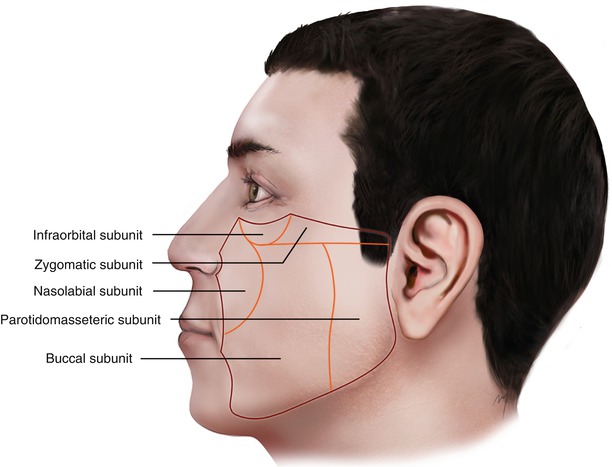
Fig. 5.2
Cheek subunits
The above subunits of the cheek are primarily anatomic in orientation as opposed to their aesthetic value. In contrast with other areas of the face such as the nose that the subunit approach during reconstruction focused attention, the cheek demands less symmetry due to the fact that its counterpart is not comparable from the same point of view.
5.1 Layered Anatomy
The soft tissues and the fasciae of the cheek are arranged concentrically over the bony skeleton. From an anatomic and surgical point of view, these structures are layered as follows:
1.
Skin
2.
Subcutaneous tissue
3.
Musculoaponeurotic layer (SMAS-mimic muscles)
4.
Parotidomasseteric fascia
5.
Buccal space and contents
6.
Deep muscular layer
7.
Retaining ligaments
Surgically important nerves and vessels travel through these layers often changing planes.
5.1.1 Skin
The skin of the cheek histologically consisted of the same components across genders and its subunits. Keratinized epithelium, hair follicles, and sebaceous and sweat glands are not homogenous throughout its entirety showing differences in thickness (ranging from 0.6 mm at the infraorbital subunit to 2.1 mm at the nasolabial subunit), quality, and laxity in each of the cheek’s subunits and across genders.
5.1.1.1 Skin and Cheek Subunits
5.1.1.1.1 Infraorbital Subunit
The skin of the infraorbital subunit is very thin with little laxity that becomes even thinner as it reaches the eyelids. Reconstructive options that involve this neighboring area to the lower lid may easily lead to ectropion. Skin incisions here must always run horizontally, parallel to the direction of the infraorbital RST lines. Every tension that is applied to the lower lid must be very carefully calculated with respect to the above factors. In addition, incisions can be camouflaged in the lower lid crease and almost become invisible after a short time.
5.1.1.1.2 Zygomatic Subunit
The zygomatic subunit is defined by the bony zygomatic complex. The skin of this subunit is attached to the underlying fascia due to fibrous retaining ligaments. The zygomatic subunit transitions from a convex area, the malar prominence, to a flatter one. Effort should be made to rebuild this protrusion by choosing an appropriate flap thickness.
5.1.1.1.3 Parotidomasseteric (Preauricular) Subunit
This subunit is bounded by the preauricular crease and a line that begins at the anterior center third of the zygomatic subunit and ends in front of the mandible’s corner. This area corresponds to the underlying parotid gland. The skin of the parotidomasseteric subunit is moderately thin and to some degree fixed to the underlying fascia showing a relative absence of laxity, especially at its most lateral preauricular part. As the skin continues medially, the thickness, laxity, and tissue availability increase particularly in elders. Incisions at this area can be hidden in the preauricular crease.
5.1.1.1.4 Buccal Subunit
The buccal cheek subunit consists of skin thicker than the rest of the other subunits, which is freely mobile over the underlying fasciae and fat. Its most medial border is the labiomandibular crease. Just lateral to the crease, the labiomandibular fold is formed by an excess of subcutaneous fat (jowl fat pad). Flaps that include the buccal subunit of the cheek become very flexible with abundant excessive tissue movement.
5.1.1.1.5 Nasolabial Subunit
The skin of the nasolabial subunit resembles the characteristics of the skin of the buccal subunit, being thick and mobile, but encompasses an important facial complex, the nasolabial crease and the nasolabial fold.
The nasolabial crease is the boundary between the cheek and the lips. Lateral to this, the nasolabial fold descends from the side of the nose to the angle of the mouth (Mallouris et al. 2013). The nasolabial crease is formed by direct (due to the absence of SMAS) dermal attachments from the underlying levator labii superioris alaeque nasi and orbicularis oris muscles (Gassner et al. 2008). The nasolabial fold is formed by the redundancy of subcutaneous fat (nasolabial fat pad) that is present lateral to the nasolabial crease in contrast to the almost absent fat medial to the nasolabial crease on the lips.
Close proximity of the nasolabial subunit with nasal ala, lip, and commissure must be considered for possible distortion, which must be prevented during flap reconstruction. The nasolabial crease does not only represent the medial boundaries of the cheek to the lips and the nose but also constitutes a line where a scar can easily be camouflaged. Furthermore, the nasolabial crease parallels the axis of the facial artery and serves as a landmark to its course.
The relaxed skin tension lines (RSTLs) on the cheek run horizontally at its upper-medial part and curve in a vertical direction as they descend to its mid- and lower third (Fig. 5.3).
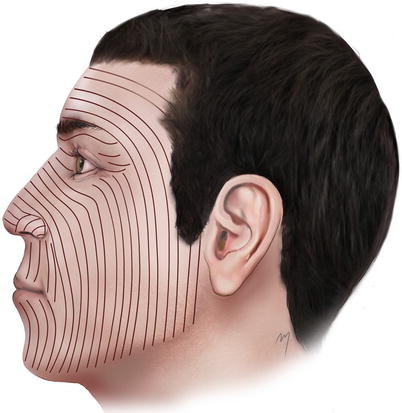
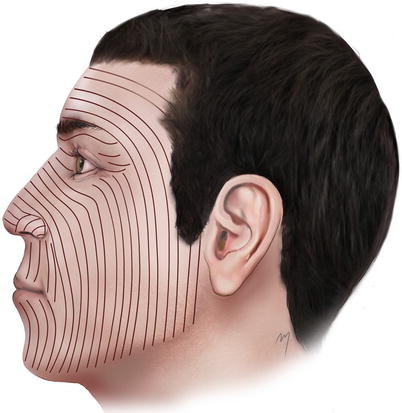
Fig. 5.3
Relaxed skin tension lines (RSTLs) at the cheek
5.1.2 Subcutaneous Layer
Just under the cheek skin lays the subcutaneous layer (Fig. 5.4). The subcutaneous layer of the cheek mainly consists of fat and connective tissue fibers running through it connecting the SMAS layer with the dermis. Vascular perforators run vertically into the subcutaneous layer as they come from the deep arteries and pass through the SMAS layer to the overlying skin. In the same manner, final neural rami are distributed to the skin undersurface. The subcutaneous layer does not show a homologous thickness like other regions of the head. It varies from being very thick in the nasolabial area and very thin (almost disappearing) close to the eyelids and the lips. The subcutaneous tissue of the cheek is characterized by the way that the fat of this layer is arranged. The subcutaneous fat is compartmentalized in multiple, distinct superficial fat pads or pockets. Retaining ligaments usually border these compartments. Within these compartments the adipose tissue is accumulated in different volumes forming the unique contour of the cheek. The fat pads that are found in the cheek have been described in detail (Owsley 1993; Pessa et al. 1998; Rohrich and Pessa 2007; Gierloff et al. 2012; Pilsl et al. 2012). The main superficial fat pads of the cheek are the malar fat pad, the nasolabial fat pad, and the jowl fat pad.
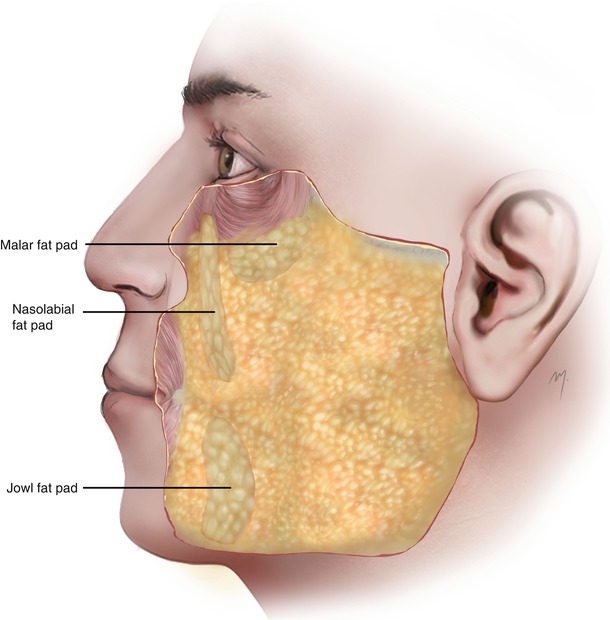
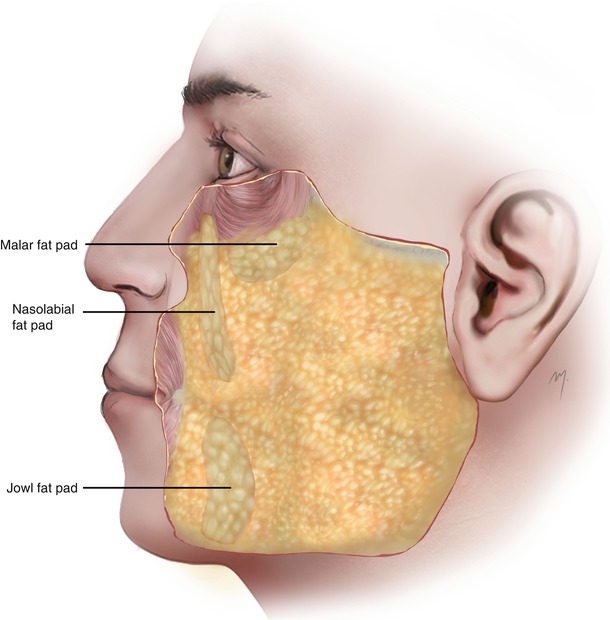
Fig. 5.4
Subcutaneous layer of the cheek and superficial fat pads
5.1.2.1 Superficial Fat Pads of the Cheek (Fig. 5.4)
The nasolabial fat pad extends lateral and parallel to the nasolabial crease and is responsible for the formation of the nasolabial fold.
The malar fat pad is located lateral to the nasolabial fat pad at the zygomatic region where it thickens to form the malar prominence. It extends superiorly toward the inferior and lateral orbital margins. Its lateral part may extend even up to the parotis. This fat pad plays an important role in facial rejuvenation procedures.
The jowl fat pad is the most inferiorly situated fat pad and lying lateral to the depressor anguli oris muscle.
The aging process in addition to the synchronous loss of ligament suspension results in fat pad ptosis. This leads to an increased prominence of the folds and the characteristic appearance of the elder face.
5.1.3 SMAS and Superficial Muscle Layer
The third layer of the cheek consisted of the SMAS and the superficial layer of the mimic muscles.
5.1.3.1 SMAS
The SMAS (superficial musculoaponeurotic system) is a single and continuous fibromuscular tissue layer of the face (Fig. 5.5). It consists of collagen, elastin and muscle fibers, fat cells, and interstitial fluid. The SMAS layer varies in its micro- and macrostructure among different areas and can appear as more adipofascial or musculofascial in nature. It has no bony attachments and supports the overlying skin. This layer contains the tendon fibers of the mimic muscles that attach to the overlying skin and thus plays an important functional role in facial movement, as it distributes the forces of the muscles to the skin.
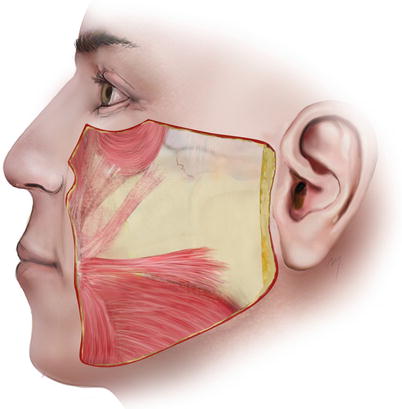
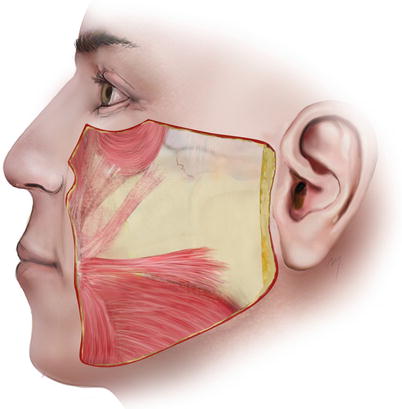
Fig. 5.5
The SMAS in lateral face
The SMAS, first described in detail as a single structure by the classic anatomic work of Mitz and Peyronie (1976), was originally defined as the fibromuscular layer in the parotid and cheek area that divides the subcutaneous fat in two discrete layers and that it is in continuity superior with the frontalis muscle and inferiorly with the platysma. Prior the definition of the SMAS by Mitz and Peyronie (1976), Skoog (1974) had already introduced dissection in a deep (“sub-SMAS”) plane for face-lifts.
Ever since its introduction, much controversy was raised in important cadaveric and histologic studies that rose questions that have not yet been definitively answered. The main points of disagreement can be summarized as follows: a clear anatomic definition, extent of SMAS in the various regions of the face and the head, the form of relation to the mimic muscles (having been described as enveloping, overlying, or merging), the number of facial muscles related to the SMAS, whether it is separate from the parotid fascia, or if it is a distinct layer from the head and neck superficial fascia (De Castro 1980; Jost and Levet 1984; Ruess and Owsley 1987; Thaller et al. 1990; Stuzin et al. 1992; Gosain et al. 1993; Yousif et al. 1994; Fuleihan 1994; Har-Shai et al. 1996, 1997; Gardetto et al. 2003; Levet 2004; Gassner et al. 2008). Parallel to the controversies regarding the SMAS, a variety of face-lifting techniques had been developed related to it (Skoog 1974; Owsley 1983; Hamra 1990; Mendelson 1992; Kamer 1996; Baker 1997).
In the posterior cheek, the SMAS lies over the parotid fascia as a clear, relatively dense layer and adheres firmly with it in a zone of 2–3 cm (Gardetto et al. 2003). Thus, the elevation of the SMAS in this area is difficult and can be achieved only by sharp dissection.
Inferiorly the SMAS passes the lower border of the mandible becoming continuous with the platysma muscle and lies over the investing layer of the deep cervical fascia. Superiorly it crosses over the zygomatic arch and becomes continuous with the temporoparietal fascia of the temple.
Extending over the masseter muscle, the SMAS covers in its upper half the zygomatic and the upper buccal branch of the facial nerve (that are running beneath the masseteric fascia) and the parotid duct. Over the lower half of the masseter, it becomes the roof of an avascular areolar tissue layer, the “premasseteric space” Mendelson et al. (2008). This layer lies immediately superficial to the masseteric fascia which constitutes its floor. It passes over the buccinator muscle, where Gassner et al. (2008) demonstrated the presence of a zone of fusion between SMAS and buccinator muscle.
In the upper cheek, the SMAS is continuous with the inferolateral portion of the orbicularis muscle. Anteriorly, medial to the zygomaticus major and to the nasolabial fold, the SMAS becomes a thin, fragile, and discontinuous fibrous network connected in variable extent and a lesser or greater degree with the mimic muscles. Τhe SMAS in this region does not appear as a clear identifiable, dissectible layer. The histologic differences of SMAS in the various areas of the face (Gardetto et al. 2003; Ghassemi et al. 2003; Gassner et al. 2008), especially those posterior and lateral to the nasolabial fold, led some authors to deny the presence of a SMAS at the anterior region of the cheek (Jost and Levet 1984; Levet 2004; Gassner et al. 2008) or even at the whole cheek (Gardetto et al. 2003). At the modiolus the SMAS merges with the orbicularis oris, zygomaticus major, and buccinator muscles.
5.1.3.2 Superficial Mimic Muscle Layer
The superficial layers of the muscles that are associated with the cheek are the orbicularis oculi, levator labii superioris alaeque nasi, levator labii superioris, zygomaticus minor, zygomaticus major, risorius, platysma, and depressor anguli oris muscles. These muscles can be topographically distinguished in an upper and a lower group (Figs. 5.6 and 5.9).
5.1.3.2.1 Orbicularis Oculi Muscle
The inferior segment of the circularly running fibers of the orbital part of the orbicularis muscle (see Chap. 3) constitutes the superficial muscle layer of the infraorbital region of the cheek (Fig. 5.6). Often the lower border of the orbicularis oculi muscle lies over the upper lip levator muscle complex, and its lateral border may extend over the upper third of the zygomaticus major muscle.
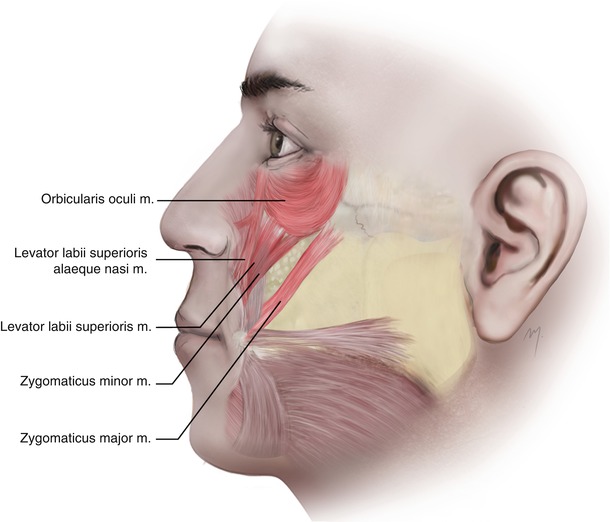
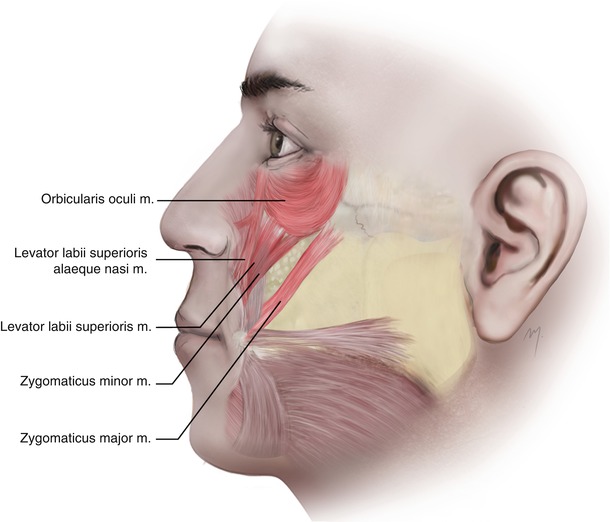
Fig. 5.6
The upper group of the superficial cheek muscles: orbicularis oculi, levator labii superioris alaeque nasi, levator labii superioris, zygomaticus minor, zygomaticus major
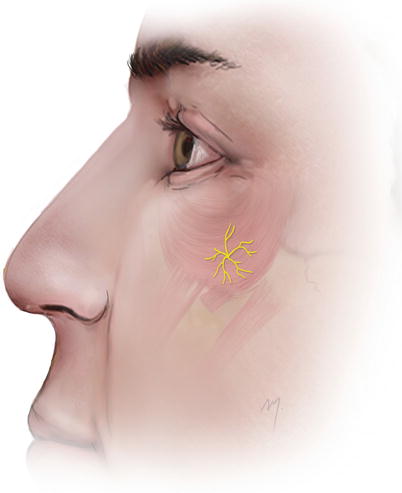
5.1.3.2.2 Suborbicularis Oculi Fat (SOOF)
Immediately under the inferolateral portion of the orbicularis oculi muscle and over the periosteum, a fat pocket termed “suborbicularis oculi fat” or SOOF is found (Fig. 5.7). This fat pocket belongs to the deep fat pockets of the face. The SOOF was described as a submuscular and supraperiosteal fat excess that is situated over the zygoma and acts as a mechanism for the orbicularis oculi muscle to glide (Aiache and Ramirez 1995; Aiache 2001). It is analogous to the retro-orbicularis oculi fat (ROOF) of the supraorbital area. It shows a horizontal medial part and a vertical lateral part (Hwang et al. 2008; Rohrich et al. 2009). Due to this it has been described having a “hockey stick head shape” with a horizontal length measuring 48 mm and a vertical height of 27 mm (Hwang et al. 2007c). The SOOF may slightly extend over the inferolateral orbital rim and protrude also slightly from the periphery of the orbicularis oculi muscle over the lip levator muscles.
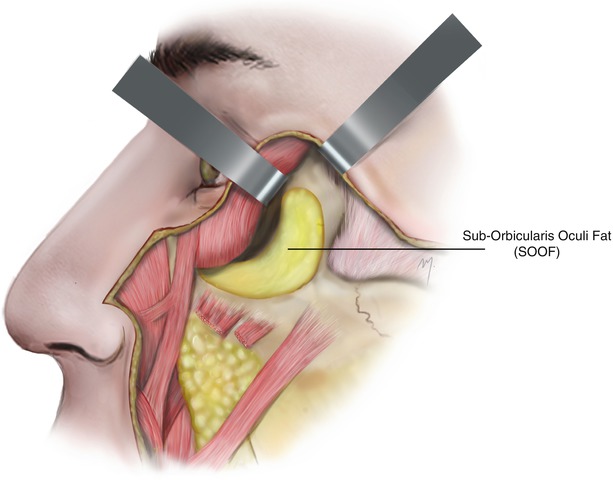
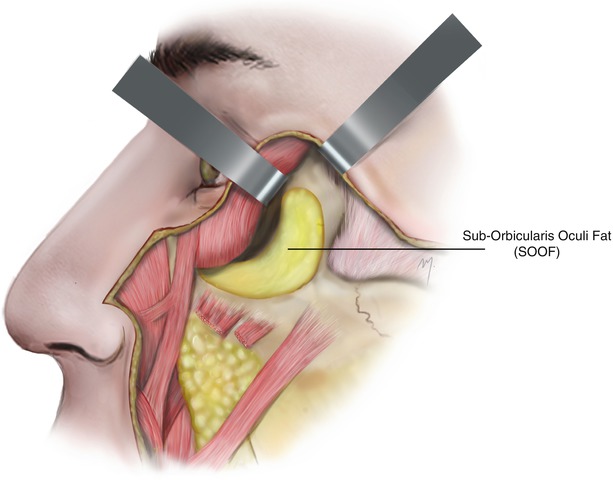
Fig. 5.7
The SOOF. The buccal extension of the buccal fat pad is seen below the lip levators
5.1.3.2.3 Levator Labii Superioris Alaeque Nasi Muscle
5.1.3.2.4 Levator Labii Superioris Muscle
The fibers of the levator labii superioris muscle (Fig. 5.6) originate from the infraorbital rim, just above the infraorbital foramen. The muscle runs inferiorly and slightly oblique to the upper lip. Before it inserts, its fibers blend with fibers of the zygomaticus minor muscle. It inserts to the upper lip between the insertions of the lateral slip of the levator labii superioris alaeque nasi and the zygomaticus minor muscles.
Branches of the facial and infraorbital arteries supply the muscle. Levator labii superioris is innervated by the zygomatic and buccal branches of the facial nerve.
Levator labii superioris muscle elevates the upper lip.
5.1.3.2.5 Zygomaticus Minor Muscle
The zygomaticus minor muscle has been found to be present in approximately 36–42 % of individuals (Pessa et al. 1998; Waller et al. 2008).
The zygomaticus minor muscle originates (Fig. 5.6) from the lateral aspect of the zygomatic bone just behind the zygomaticomaxillary suture. Some of its fibers originate from the orbicularis oculi muscle. It runs downward and medially into the upper lip. As it continues, its fibers blend with fibers of the orbicularis oculi muscle in various sites, which is the reason that the zygomaticus minor is in many cases difficult to distinguish (Youn et al. 2012). It inserts to the upper lip, but before its insertion, it blends with levator labii superioris muscle.
The superior labial branch of the facial artery supplies the muscle. Innervation is supplied by rami of the zygomatic and buccal branches of the facial nerve. It elevates the upper lip.
5.1.3.2.6 Zygomaticus Major Muscle
The zygomaticus major muscle (Fig. 5.6) originates from the zygomatic bone, anterior to the zygomaticotemporal suture and lateral to the origin of the zygomaticus minor muscle.
Because the zygomaticus major muscle serves as an important landmark to deep-plane (sub-SMAS) dissection, many attempts have been made to identify its upper part and origin by using several bony landmarks (Mowlavi and Wilhelmi 2004; Spiegel and DeRosa 2005; Miller et al. 2007).
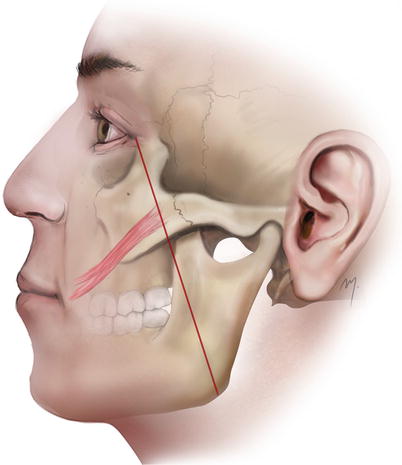
A simple and accurate landmark depicting the origin of the zygomaticus major muscle was proposed by Tremolada et al. (1994). According to them, its origin is represented by the point where a line that connects the lateral canthus with the mandibular angle crosses the inferior edge of the zygomatic bone (Fig. 5.8). The origin of the zygomaticus major sometimes may be covered by the inferolateral part of the orbicularis oculi muscle.
The zygomaticus major runs in an oblique direction toward the angle of the mouth.
It may appear bifid, having two separate muscle bands, in the 35–40 % of individuals (Pessa et al. 1998; Hu et al. 2008). In these cases the muscle originates normally and at the infrazygomatic region divides in a superior and an inferior bundle. The superior bundle inserts at the oral commissure and the inferior below it. Its mean width is approximately 12 mm (Pessa et al. 1998).
The muscle fibers insert into the labial angle, where they blend with the fibers of the levator anguli oris, the depressor anguli oris, and orbicularis oris muscles, risorius, buccinator. The muscle fibers that converge at the oral commissure form a tendinous node that firmly attaches to the dermis at the labial angle that is termed modiolus (see Chap. 6). The zygomaticus major muscle short before its insertion at the commissure is bifurcated into one superficial and one deep insertion head where the levator anguli oris muscle passes between them (Nairn 1975; Frellinger et al. 1987). In a detailed study, Shim et al. (2008) found that the above pattern is present in 60 % of the cases while in about 24 % the muscle divides into three insertion heads and in the remainder no division occurs. Depending on the insertion pattern, the muscle fibers blend each time with different muscle fibers of the modiolar region.
Its vascular supply comes from the superior labial branch of the facial artery. The muscle is innervated by rami of the zygomatic and buccal branches of the facial nerve.
This muscle belongs to the levator muscles of the oral commissure as it draws the angle of the mouth upward and laterally.
5.1.3.2.7 Risorius Muscle
The risorius (Fig. 5.9) is an inconstant muscle that is present in only 6 % of the individuals (Pessa et al. 1998). When present, the risorius muscle is variable in shape and form and is located at the lateral aspect of the cheek.
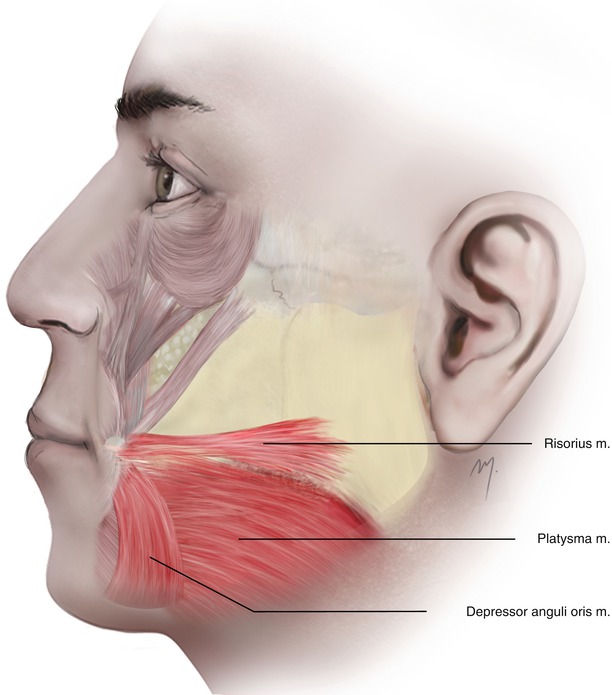
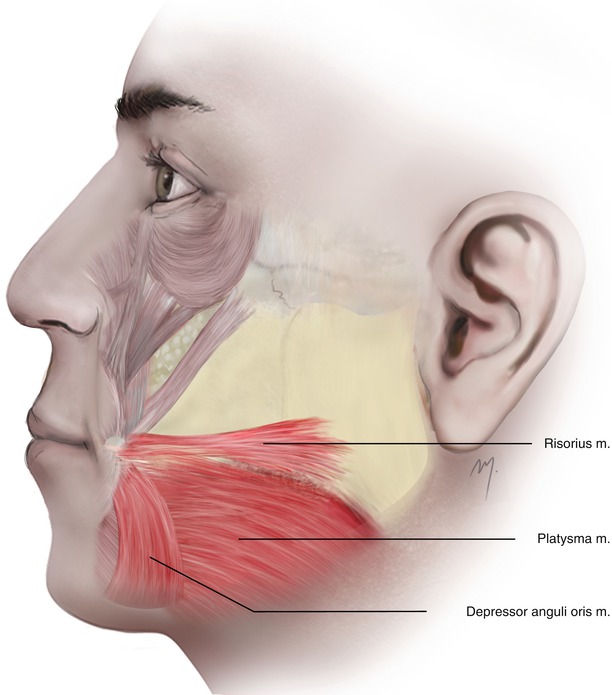
Fig. 5.9
The lower group of the superficial cheek muscles
Its fibers usually arise from the SMAS over the parotis and from the platysma muscle. It may also originate from the zygomatic arch. Depending on its origin, the muscle fibers run anteriorly in an oblique or horizontal axis. It inserts to the angle of the mouth.
The superior labial branch of the facial artery supplies the risorius. Buccal branches of the facial nerve innervate the muscle. Risorius retracts the angle of the mouth laterally.
5.1.3.2.8 Platysma Muscle
The platysma muscle (Fig. 5.9) is a neck muscle (see Chap. 8) but its lateral fibers cover a wide area of the inferior cheek. Superiorly the platysma becomes continuous with the SMAS, representing an anatomically homogenous unit that maintains its muscular consistency and direction of fibers as it crosses the mandible. The lateral fibers of the platysma muscle, coming from the neck, cross the mandible, pass over and cover the lower part of the parotid fascia and the masseteric fascia, and run superomedially. They continue deep to the risorius muscle, reaching the posterolateral border of the depressor anguli oris. They converge with the facial muscles at the lower lip. A portion of platysma muscle fibers also converges to the modiolus of the angle of the mouth and is referred to as platysma pars modiolaris.
The platysma muscle pulls the lower lip down and the corner of the mouth downward and laterally.
5.1.3.2.9 Depressor Anguli Oris Muscle
The depressor anguli oris muscle belongs to the depressor muscles of the oral commissure.
The depressor anguli oris muscle (Fig. 5.9) originates from the mandible inferior to the mental foramen and some fibers from the platysma. It has a linear origin that extends from the mental tubercle to a lateral distance of about 36 mm (Hur et al. 2008). Its muscle fibers run upward converging toward the angle of the mouth. It inserts to the angle of the mouth with its fibers blending with fibers of the orbicularis oris and risorius muscles. The inferior labial branch of the facial artery and the mental branch of the maxillary artery supply the muscle. The buccal and mandibular branches of the facial nerve innervate the depressor anguli oris. The depressor anguli oris pulls the angle of the mouth downward and laterally.
5.1.4 Parotidomasseteric Fascia
Just below the SMAS is a thin and glazed fascia that lies over the parotis posteriorly and over the masseter muscle anteriorly, termed the parotidomasseteric fascia (Fig. 5.10). This fascia can be found having a variable thickness and transparency, making the underlying structures slightly distinguishable.
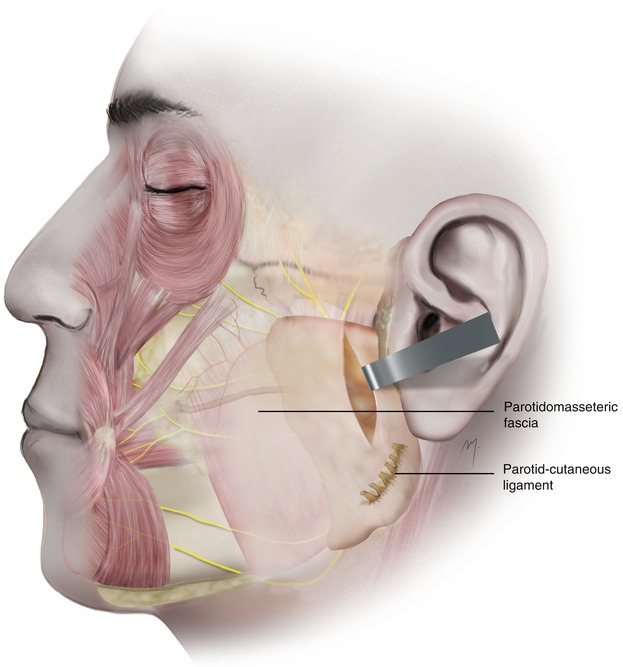
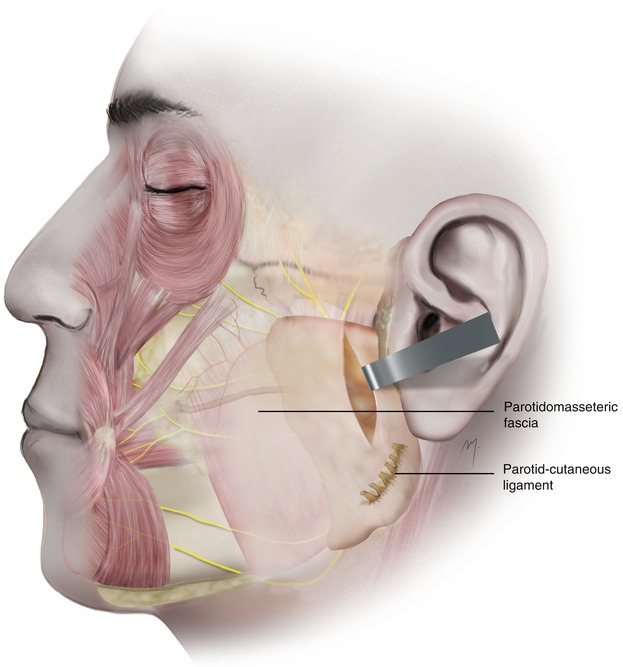
Fig. 5.10
The parotidomasseteric fascia and the parotid-cutaneous ligament
The parotidomasseteric fascia is formed from the continuation of the investing layer of the deep cervical fascia to the head. The investing layer of the deep cervical fascia at the mandible splits in a lateral and a medial layer to surround the outer and the inner surfaces of the mandible body, respectively. As it extends superiorly, the lateral layer covers the outer surfaces of the parotis and masseter muscle and is termed parotidomasseteric fascia. Above the zygomatic arch, the parotidomasseteric fascia corresponds to the loose areolar tissue layer of the temporal area but is quite different in nature. The parotidomasseteric fascia must not be confused with the masseter muscle fascia that invests directly the masseter muscle and lies in deeper layer.
The parotidomasseteric fascia covers the parotid duct, branches of the facial nerve, and the transverse facial artery that runs beneath it and may be felt as they protrude. It also lies over the buccal fat pad and extends anteriorly blending with the epimysium of the facial muscles.
Over the parotis the fascia may show a variable thickness and strength and is densely adherent to the overlying SMAS. A false retaining ligament found here, the parotid-cutaneous ligament, amplifies the restraint of the skin. The parotid-cutaneous ligament (Fig. 5.10) is situated as a fibrous band along the posteroinferior part of the parotid gland that originates from the parotid fascia and running to the dermis anchors the skin. It is felt as resistance when elevating the skin over the parotis and has to be released. In contrast to the above area, over the lower half of the masseter muscle, Mendelson et al. (2008) described a loose areolar space, the “premasseter space”, that exists between the parotidomasseteric fascia and the SMAS platysma. This space contains no vital structures and can serve as a safe avascular sub-SMAS dissection plane.
5.1.5 Buccal Space
The parotid masseteric fascia bounds the lateral border of the buccal space found beneath it. It is filled by the buccal fat pad and its extensions and important structures that are contained in this compartment. The contents of the buccal space are the buccal fat pad and its extensions that almost fill the space, the parotid duct and minor salivary glands, the inconstant accessory parotid gland, buccal nodes, and nerves and vessels (Fig. 5.11). The nerves found in this space are the motor buccal nerve (branch of the facial nerve) and the sensory buccal nerve (division of V3). The vessels found here are the facial artery and vein and the buccal artery, all of which are examined below.
The buccal fat pad (of Bichat) is one of the deep fat pads that provide fullness to the cheek. Bichat was the first to describe it in (1802) as an encapsulated (with a thin capsule), fatty mass that fills the buccal space and has the buccinator muscle medially and the masseter muscle laterally. It shows a body and multiple extensions. The buccal fat pad is well developed and evident in infants. In adults its mean volume ranges from 9 to 10 ml, being grater in males, and its mean thickness is 6 mm (Loukas et al. 2006b). It plays an important role in suckling, mastication, and aesthetics, as it is located in a protrusive position of the cheek. Zhang et al. (2002) described in details the body and the processes of the buccal fat pad. He mentioned that the body of the buccal fat pad consists of three lobes (an anterior, an intermediate, and a posterior), fixed by ligaments to the surrounding structures. According to this description that has been further accepted (Loukas et al. 2006b; Yousuf et al. 2010), the anterior lobe is triangular in shape, is located below the zygoma, and extends anterior to the buccinator, under the zygomatic major, filling the deep space below the labii superioris muscle. The intermediate lobe is developed in children and thin in the adults and is situated around the posterior and the anterior lobe. The posterior lobe is located in the masticatory space and the surrounding spaces. The buccal fat pad shows four extensions: the pterygoid process, the pterygopalatine process, the buccal process, and the temporal process. The pterygoid process fills the pterygoid space, while the pterygopalatine extends to the pterygopalatine fossa. The temporal process is the buccal fat pad’s extension into the temporal region. This extension in the temporal area is termed as deep temporal fat pad that lies between the temporalis fascia and the outer surface of the temporalis muscle (the superficial temporal fat pad is not a part of this extension but a distinct entity) (Stuzin et al. 1989, 1990). Functionally this extension allows the temporalis muscle to glide easily under the zygomatic arch. The buccal process is the most superficial and is the extension of the buccal fat pad body below the parotid duct. The parotidomasseteric fascia covers the buccal fat pad in its lateral aspect, and the buccal branch of the facial nerve and the parotid duct are related to it. The buccal branch of the facial nerve crosses usually (74 %) superficial to the buccal fat pad but sometimes (26 %) small branches of the nerve pass through its buccal extension (Hwang et al. 2005). The arteries that supply the buccal fat pad are derived from the buccal and deep temporal branches of the maxillary artery, from the transverse facial branch of the superficial temporal artery, and from branches of the facial artery. The buccal fat pad has been widely used as a flap in the closing of oroantral fistulas. It is also a very useful tool in mucosa resurfacing in nearby to it through and through cheek defects.
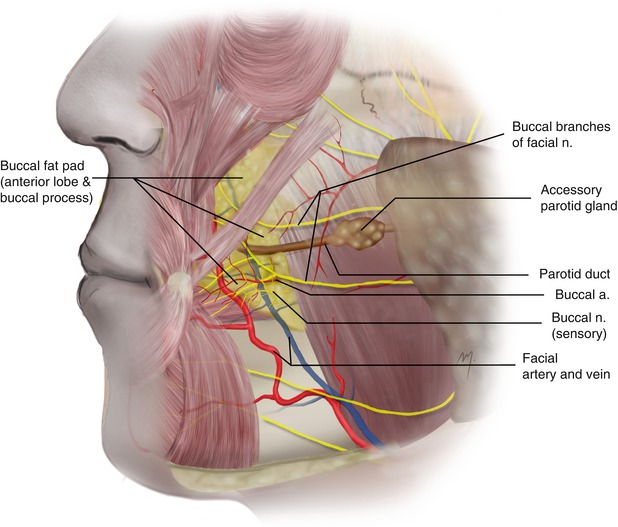
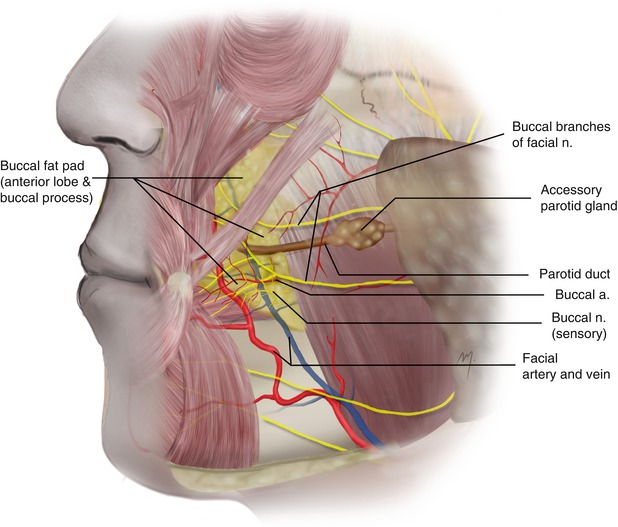
Fig. 5.11
Buccal space and its contents
The parotid duct (Stensen’s duct), with a length of 6–7 cm, arises from the anterior border of the parotis and runs horizontally over the masseter muscle. At its anterior border, it turns sharply, passing through the buccal fat pad, pierces the buccinator, and opens to the oral cavity, opposite the upper second molar. Its trajectory can be represented by a line connecting the tragus with the commissure. The buccal branches of the facial nerve are related to the parotid duct as they are running parallel, above and below to it. The parotid duct passes along the lateral surface of the buccal fat pad and its buccal extension. It has been reported that in 26 % of the individuals the parotid duct can also be found deep to the buccal extension of the fat pad (Hwang et al. 2005).
The facial artery courses through the buccal space at its anterior part while the facial vein is found slightly posterior.
5.1.6 Deep Muscle Layer
The deep muscle layer of the cheek consists of the masseter, buccinator, and levator anguli oris muscles.
5.1.6.1 Masseter Muscle
The masseter muscle (Fig. 5.12), a quadrilateral in shape muscle, anatomically belongs to the masticatory muscles but topographically it occupies the frontal half of the parotidomasseteric region of the cheek. The parotid gland lies over its posterior part, and the buccal, the lower zygomatic branches of the facial nerve, and the parotid duct run over its surface. The masseter muscle consists of three layers that blend anteriorly: the superficial layer being the largest, the intermediate layer, and the deep layer.
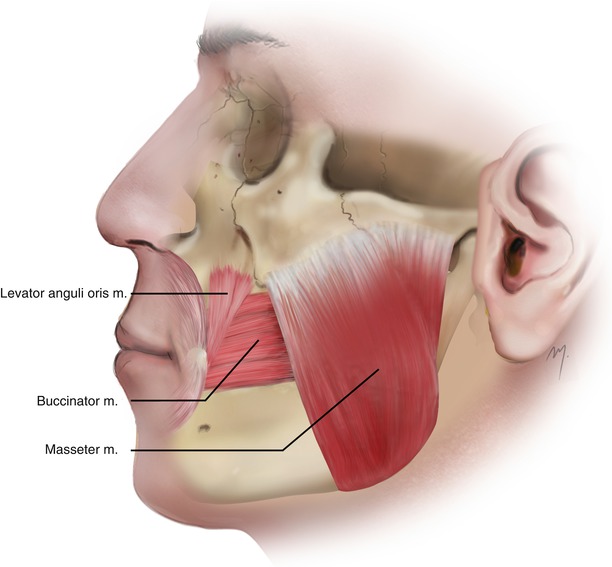
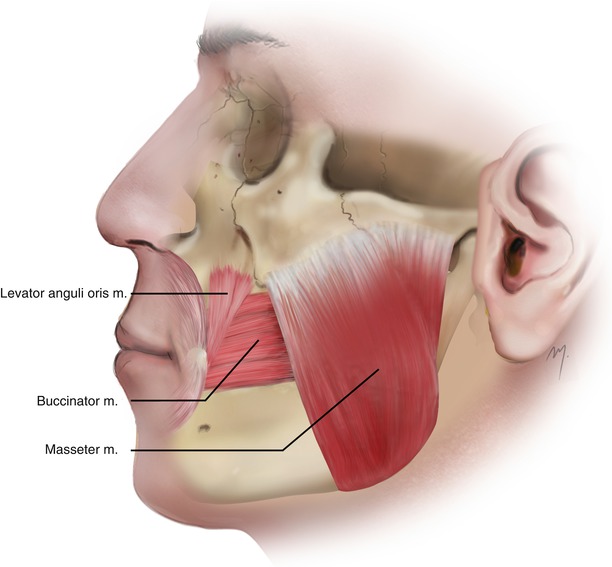
Fig. 5.12
Deep muscle layer of the cheek
The superficial layer originates by a thick aponeurosis from the maxillary process of the zygomatic bone and the anterior two-thirds of the inferior border of the zygomatic arch. The intermediate layer originates from the deep surface of the anterior two-thirds of the zygomatic arch and from the lower border of its posterior third. The deep layer originates from the deep surface of the zygomatic arch.
The fibers of the superficial layer run inferiorly and posteriorly to the mandible in an oblique axis, while the fibers of the intermediate and deep layer run in the same direction slightly more vertical.
The superficial layer inserts into the angle and the lower posterior half of the lateral surface of the mandibular ramus, the intermediate layer into the central part of the ramus, and the deep layer into the upper part of the ramus and the coronoid process.
It has not been clarified whether fibers of the masseter muscle are attached to the auricular disk of the temporomandibular joint (Yung et al. 1990; Velasco et al. 1993; Loughner et al. 1996). It has been reported that in about the half of the individuals, muscle fibers of the deep layer of the masseter attach to the auricular disk and capsule (Matsunaga et al. 2009).
The masseter muscle is supplied by the masseteric branch of the maxillary artery and small branches, which arise from the facial and the transverse facial arteries. Additionally, the deep temporal artery contributes to the masseter supply by means of a small muscular branch (Won et al. 2012). The masseter receives its nerve supply from a branch of the anterior trunk of the mandibular nerve.
The masseter primarily elevates the mandible to occlude the teeth.
5.1.6.2 Buccinator Muscle
The buccinator muscle (Fig. 5.12) is a thin and quadrilateral muscle that forms the base of the bucal space, and fills the gap between the maxilla and the mandible.
It originates in the form of a horseshoe from the maxilla, the mandible, and the pterygomandibular raphe. Its superior border is attached to the outer surface of the alveolar process of the maxilla, its posterior border to the anterior margin of the pterygomandibular raphe, and its inferior border to the outer surface of the alveolar process of the mandible.
The fibers of the buccinators run almost parallel to the angle of the mouth. The posterior part of the muscle is situated initially deep to the ramus of the mandible and to the masseter muscle being separated from them by the buccal fat pad. Its anterior part runs under the zygomaticus major, risorius, levator, and depressor anguli oris muscles and under the facial artery, the facial vein, and branches of the facial and buccal nerves. The parotid duct, after curving the frontal border of the masseter muscle, pierces the buccinator at the level of the maxillary third molar and enters the mouth opposite the maxillary second molar tooth. Deep in the muscle lies the submucosal layer of the oral cavity.
The buccinator muscle has been described as consisting of four muscle fiber bands: the upper band originating from the maxilla, the second band originating from the pterygomandibular raphe, the third band extending from the mandible, and an inconstant most inferior band originating from the mandible under the previous one, running to the midline and merging with its contralateral (Mortellaro et al. 2001; D’Andrea and Barbaix 2006; Hur et al. 2011).
The buccinator inserts into the labial angle, the upper and the lower lip in the following manner: The upper fibers of the buccinator continue as fibers of the lower part of the orbicularis oris muscle while the lower fibers continue as fibers of the upper part of the orbicularis oris muscle, intersecting each other.
The uppermost fibers continue as fibers of the upper part of the orbicularis oris muscle and the lowermost fibers continue as fibers of the lower part of the orbicularis oris muscle.
Small muscle fibers of the buccinator muscle, lengthening from 3 to 10 mm, form a distinct bundle that extends to the terminal portion of the parotid duct, functioning in the saliva secretion (Kang et al. 2006).
The vascular supply of the buccinator muscle has been described in detail due to its use as a flap for intraoral covering (Bozola et al. 1989; Carstens et al. 1991; Zhenmin Zhao et al. 1999). It receives its blood supply from branches of the facial and the internal maxillary arteries. The facial artery provides posterior, inferior, and anterior branches to the buccinator, which supply the posterior, inferior, and anterior portions of the muscle, respectively. The internal maxillary artery contributes to the vascular supply of the buccinator mainly due to the buccal artery and a contribution of the posterior-superior alveolar artery.
The buccal artery after branching from the second part of the maxillary artery runs deep into the mandibular ramus, anterior and inferior to the lateral pterygoid muscle, and supplies the posterior part of the buccinator. It anastomoses with the posterior buccal branch of the facial artery.
The posterior-superior alveolar artery enters the posterior-superior part of the buccinator and supplies this part of the muscle. Small branches of the infraorbital artery also supply the anterior-superior part of the buccinator.
The buccal branch of the facial nerve provides the motor innervation to the buccinator muscle.
The buccinator compresses the cheek and also acts to propel food during mastication, sucking, and whistling. It also participates in the lateral retraction of the oral commissure.
5.1.6.3 Levator Anguli Oris Muscle
The levator anguli oris muscle (Fig. 5.12) belongs to the levators of the oral commissure muscles and is the deepest muscle of the upper lip levator complex. It is rectangular in shape with a length of 4.8 cm and a width of 1.2 cm (Ewart et al. 2005).
Levator anguli oris muscle originates from the canine fossa of the maxilla, approximately 1 cm inferiorly to the infraorbital foramen. The muscle runs inferiorly, covered by the levator labii superioris and zygomaticus minor muscles. It inserts into the labial angle, converging with the fibers of the zygomaticus major, depressor anguli oris, and orbicularis oris and the fibers of the other muscles that form the modiolus.
The levator anguli oris muscle is supplied by the superior labial branch of the facial artery and the infraorbital branch of the maxillary artery. It receives its nerve supply from the rami of the zygomatic and buccal branches of the facial nerve. Levator anguli oris muscle raises the angle of the mouth.
5.1.7 Retaining Ligaments
Several ligaments support the facial skin in its normal anatomic position against gravitational forces. These ligaments, referred to as retaining ligaments, were first described by Furnas (1989). The retaining ligaments of the cheek draw attention due to their role in the aging process and in the rejuvenation procedures of the face (Stuzin et al. 1992; Pilsl and Anderhuber 2010; Furnas 1994; Mendelson 1995, 2009). The retaining ligaments run as fibrous bands from the deep facial structures to the overlying dermis. The retaining ligaments of the cheek are found in specific locations and can be felt as resistance to flap elevation and must be released as they cross through the dissection plane.
Several retaining ligaments have been described in the cheek (zygomatic ligament, masseteric ligament, mandibular ligament, platysma-auricular ligament, buccomaxillary ligament, platysma-mandibular ligament, subcutaneous parotid masseteric ligament) and are often the same ligaments with different nomenclature. The bands of the ligaments may originate from the periosteum and are termed as true retaining ligaments, or they may originate from the SMAS and insert as the previous into the dermis and are termed as false retaining ligaments.
The true ligaments of the cheek (Fig. 5.13) that arise from the osseous background of the cheek are the following.
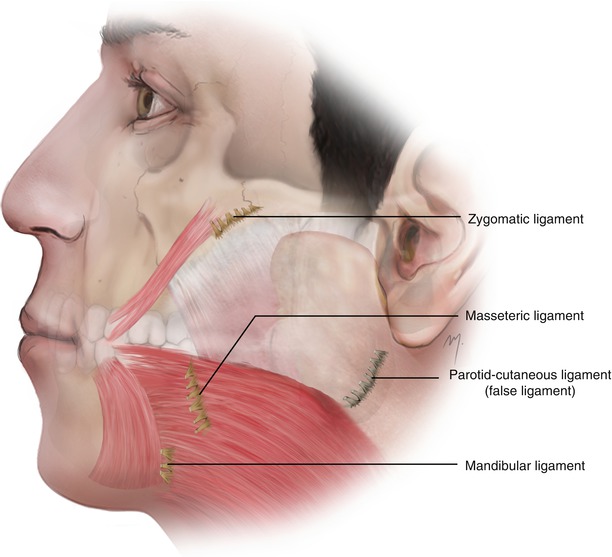
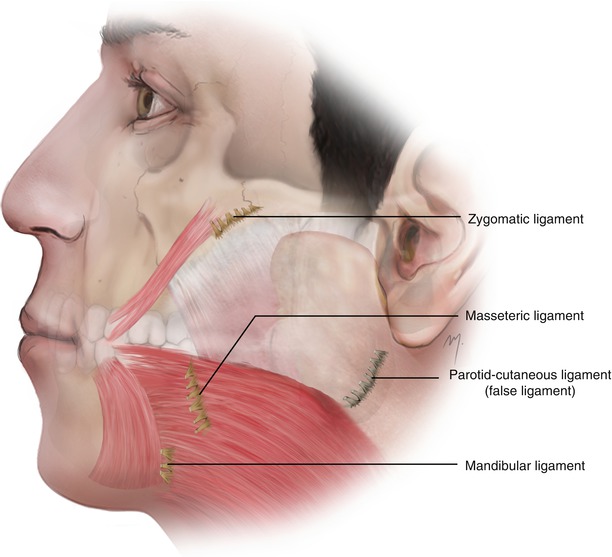
Fig. 5.13
True retaining ligaments at the cheek
The zygomatic ligament (McGregor’s patch) originates as a series of fibrous septa from the periosteum at the junction of the zygomatic arch and zygomatic body just lateral to the zygomaticus major muscle.
The masseteric ligaments are found as they extend along the anterior border of the masseter muscle.
The mandibular ligament originates from the periosteum of the external surface of the mandibular body, 5 mm superiorly to the inferior edge and lateral to the depressor anguli oris muscle.
5.1.8 Arterial Supply
The cheek receives its blood supply mainly from branches of the external carotid artery, with a minor contribution of the internal carotid artery due to a small branch of the ophthalmic artery. The arteries of the external carotid that contribute to its arterial vasculature are the infraorbital, the transverse facial, and the facial arteries. The contribution of the internal carotid system happens by the small zygomaticofacial artery.
5.1.8.1 Infraorbital Artery
The infraorbital artery is one of the three branches of the maxillary artery, together with the mental and buccal arteries, that supply the face.
The infraorbital artery arises from the third part of the maxillary artery. It enters the orbit through the posterior part of the inferior orbital fissure. It runs on the floor of the orbit along the infraorbital groove and enters the infraorbital canal in company with the infraorbital nerve. On its course in the infraorbital groove and canal, it gives branches for the inferior rectus and inferior oblique muscles, the nasolacrimal sac and the anterior superior alveolar artery, and sometimes the middle superior alveolar artery.
The artery emerges onto the face through the infraorbital foramen (Fig. 5.14). The infraorbital artery is located in the middle and superficial of the infraorbital nerve bundle in about 74 % of the cases, lateral to it in 20 %, and in the remainder medial to it (Hu et al. 2006). As it exits to the face, through the infraorbital foramen, it lies under levator labii superioris muscle and very quickly divides into its lower lid, nasal, and superior labial and cheek branches.
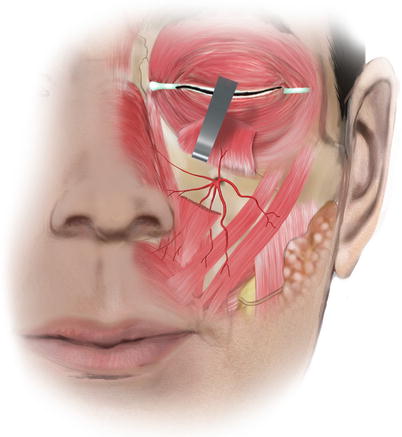
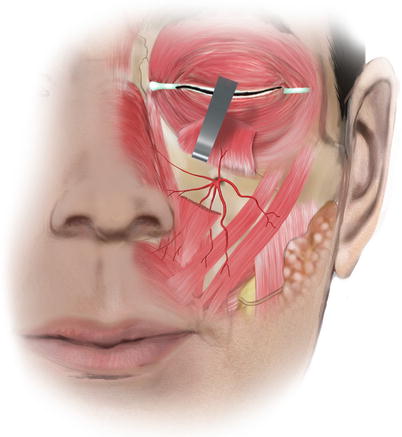
Fig. 5.14
The infraorbital artery at the face
The lower lid branches run upward under the cover of the orbicularis oculi muscle, and after piercing it they distribute to the skin of the lower eyelid. The nasal branches of the infraorbital artery distribute to the lateral side of the nose. The superior labial branches are larger and numerous. They run inferiorly between the levator labii superioris and the levator anguli oris and are distributed to the upper lip and the anterior part of the cheek. Multiple anastomosing branches connect the infraorbital artery with the angular, the dorsal nasal, the transverse facial, and the buccal arteries.
5.1.8.2 Zygomaticofacial Artery
The zygomaticofacial artery constitutes the contribution of the internal carotid artery to the cheek. It is a branch of the lacrimal artery, which in turn is branched from the ophthalmic artery of the internal carotid. The lacrimal artery runs forward at the junction of the orbital roof and the orbit lateral wall. Within the orbit, it gives off the zygomatic artery, which subdivides into the zygomaticotemporal and zygomaticofacial artery.
The zygomaticofacial artery appears on the cheek (Fig. 5.15) through the zygomaticofacial foramen and supplies the skin of the malar region. The zygomaticofacial foramen varies in its position and is expected to be found in a mean distance of 1.1 cm from the inferolateral orbital margin (Loukas et al. 2008). When the zygomaticofacial artery exits, it immediately supplies the skin of the malar region. In cases where the inferolateral portion of the orbicularis oculi muscle extends over the zygomaticofacial foramen, the artery pierces the muscle to reach the subcutaneous tissue. The zygomaticofacial artery anastomoses with the transverse facial and zygomaticoorbital arteries.
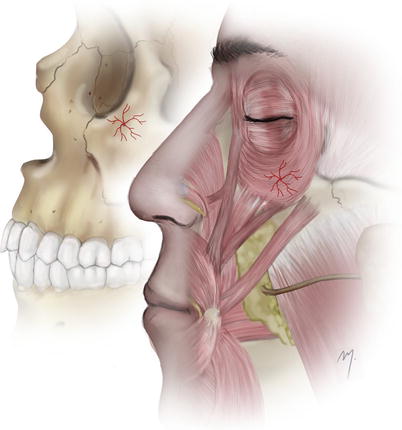
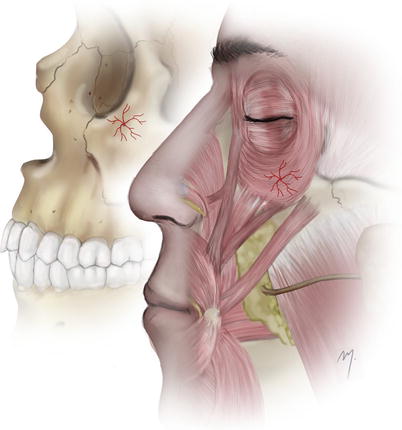
Fig. 5.15
Zygomaticofacial artery
5.1.8.3 Superficial Temporal Artery: Preauricular Course
The superficial temporal artery is the smaller of the two terminal branches of the external carotid artery (the other one being the maxillary artery). The bifurcation of the external carotid artery happens at the level of the neck of the mandibular condyle, deep or even within the parotis that identifies the origin of the superficial temporal artery. The artery runs upward as a continuation of the external carotid artery and passes over the zygomatic arch continuing along the side of the head where it bifurcates to the frontal and parietal branches.
Its long course can be distinguished in two parts: a first preauricular part at the cheek and a second temporal part above the zygomatic arch.
5.1.8.3.1 Preauricular Course
After its origin, the superficial temporal artery continues upward giving off the transverse facial artery after which it appears at the superior border of the parotid gland. It pierces the parotidomasseteric fascia and continues along within the SMAS temporoparietal fascia layer.
Ascending from the parotid gland, the superficial temporal (Fig. 5.16) artery passes at a distance ranging from 0.5 to 1.0 cm in front of the anterior edge of the tragus, in a depth of up to 1.0 cm. The mean diameter of the superficial temporal artery here ranges between 2 and 2.7 mm (Stock et al. 1980; Lang 1995; Chen et al. 1999; Pinar and Govsa 2006).
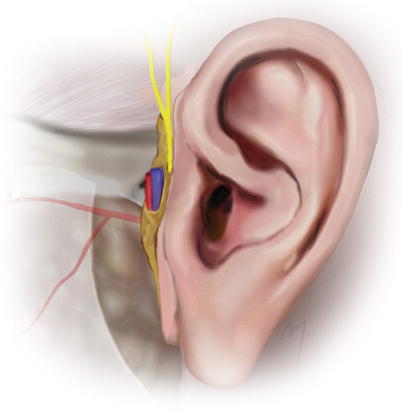
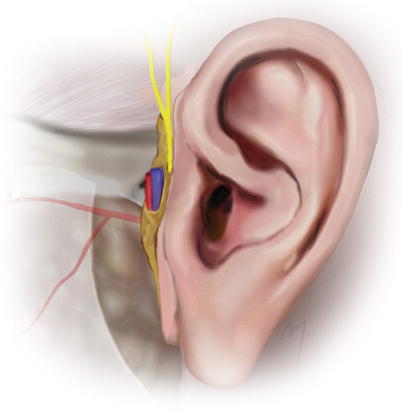
Fig. 5.16
Superficial temporal artery at the preauricular region and its relation to the superficial temporal vein and the auriculotemporal nerve
Even though many variations exist, the most usual in the pretragal area is that superficial temporal vein which accompanies the artery, runs laterally to it and in a more superficial level. The auriculotemporal nerve runs lateral or superficial to the artery and in a variable unpredictable relation to the vein. As many scalp and facial flaps involve a preauricular incision and a preauricular flap elevation, the above relation of the vessels and the distance from the tragus must be kept in mind so as to avoid injury.
The superficial temporal artery gives off two small branches, the middle and the lower auricular arteries (the upper auricular artery is branched from a higher level at the temporal course of the superficial temporal artery) that contribute to the supply of the auricle (see Chap. 7).
5.1.8.4 Transverse Facial Artery
The transverse facial artery (Fig. 5.17) arises from the superficial temporal artery before it emerges from the gland. In 70 % of cases, it arises as one branch and in the rest as two or three (Yang et al. 2010). It is situated in a plane deep to the facial nerve.
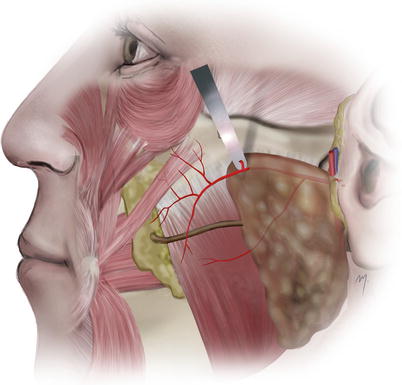
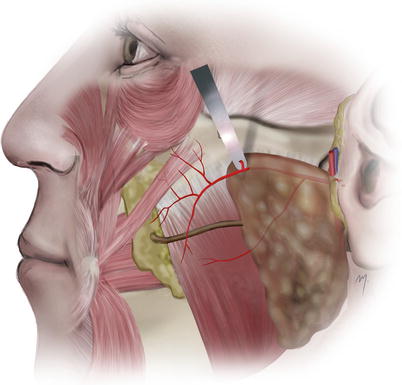
Fig. 5.17
The transverse facial artery
In their detailed study, Yang et al. (2010) found out that the transverse facial artery usually divides within in the parotid substance into two trunks that in most cases emerge from the anterior border of the gland, as superior and inferior branches, and described their course as follows.
The superior branch, the largest one, emerges from the upper part of the parotis and courses forward into the cheek, located between the zygomatic arch and the parotid duct in a distance of about 1.5 cm inferiorly to the zygomatic arch. It usually gives off a descending branch that crosses the parotid duct and supplies the area below the duct together with the inferior branch. The superior branch also gives branches to the superior part of the masseter, to the zygomaticus major, and multiple branches to the soft tissues of the malar area.
The inferior branch, smaller than the previous, emerges from the lower part of the parotis and runs superficial to the masseteric fascia, coursing inferior to the parotid duct. It distributes to the masseter muscle terminating as muscular or as cutaneous branch. The inferior branch in about 27 % terminates its course within the parotid gland as muscular branch.
Due to its numerous branches, the transverse facial artery supplies the parotid gland, the parotid duct, the facial nerve, the masseter muscle, and a large area of the cheek skin.
An important large cutaneous perforator of the transverse facial artery (Fig. 5.18), located approximately 3 cm lateral and 3.5 cm inferior to the lateral canthus, provides the main direct blood supply to the skin of the preauricular area and the lateral cheek, defining its vascular territory (Whetzel and Mathes 1992, 1997; Schaverien et al. 2009). The territory, perfused by this perforator, extends superiorly 1–2 cm above the zygomatic arch, inferiorly 2 cm above the border of the mandible, anteriorly over the malar eminence to the lateral canthus, and posteriorly 1–2 cm anterior to the ear (Whetzel and Mathes 1992; Whetzel and Stevenson 1997). This perforator branch is sectioned during elevation of flaps when dissecting in this area. However, the viability of the flaps is guaranteed due to collateral flow from the multiple anastomosing branches of the neighboring arteries.
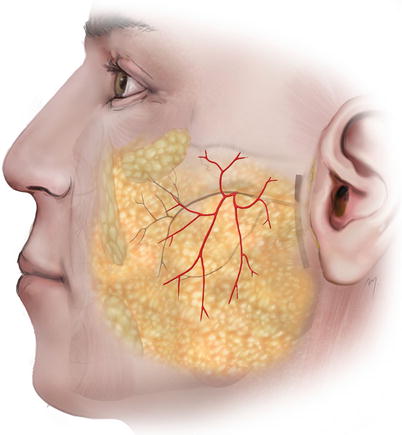
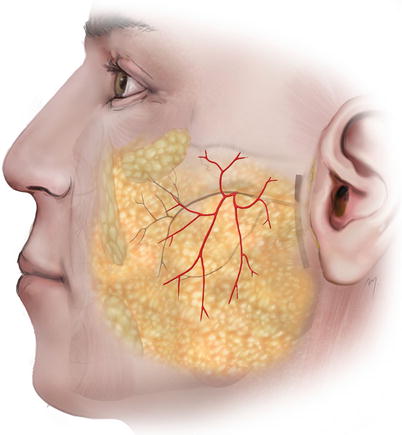
Fig. 5.18
Cutaneous perforator of the transverse facial artery
The transverse facial artery anastomoses with the zygomaticoorbital, the lacrimal and the infraorbital arteries superiorly, the facial and the masseteric arteries anteriorly, and the buccal artery deeply.
The development of the transverse facial artery is anatomically and functionally related inversely to the development of the facial artery. The facial artery may be underdeveloped and end as superior or inferior labial artery (see Sect. 5.1.8.7). In these cases the missing territory of the facial artery is “taken over” to a variable extent, by the ipsilateral transverse artery (Cormack and Lamberty 1994).
A giant and largely dilated transverse facial artery has also been reported to counterpoise the complete agenesis of a facial artery (Tubbs et al. 2005).
5.1.8.5 Buccal Artery
The buccal artery (Fig. 5.19) is a small branch that arises from the second part of the maxillary artery. It runs between the medial pterygoid and the attachment of the temporalis muscle, crosses the buccinator, and just anterior to the anterior edge of the masseter muscle pierces the buccal fat. It supplies the skin of an area over the buccinator muscle and anastomoses with branches of the infraorbital and facial artery.
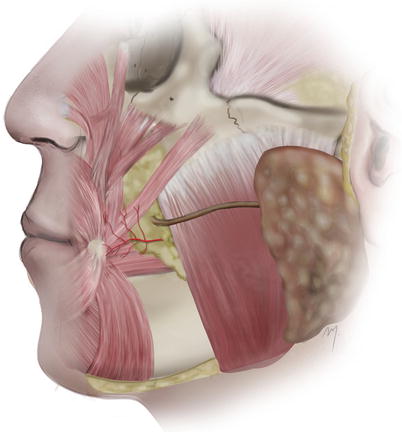
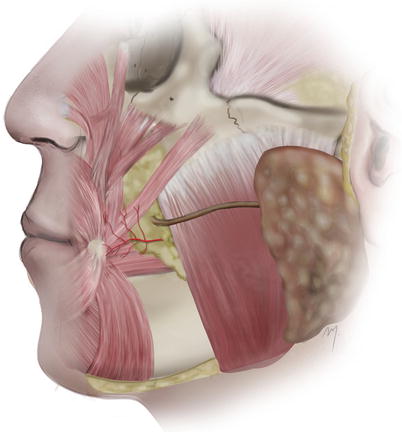
Fig. 5.19
Buccal artery
The artery is located about 3 cm lateral to the oral commissure and at the same level 5 mm medial to the medial aspect of the masseter muscle.
5.1.8.6 Facial Artery (Facial Part)
The facial artery is a long, major facial vessel, with important branches, that starts from the carotid triangle and usually ends to the inner canthus. This long course can be distinguished into a cervical and facial part. The cervical part of the facial artery is the segment from its carotid artery origin to the point where it curves around the lower border of the mandible to enter the face (see Chap. 8).
The cervical part of the facial artery as it comes from the posterior aspect of the submandibular gland reaches the lower mandibular border, curves around it, passes just in front of the anterior edge of the masseter muscle, pierces the deep fascia, and enters the face. At this point the facial artery, with its accompanying vein, lies immediately under the platysma and crosses with the mandibular branch of the facial nerve lying underneath it. When a dissection in this area is performed, it must be protected, as it lies very superficial at this point (where its pulsation is most palpable). In this region, its external diameter is about 2.6 mm (Pinar et al. 2005).
5.1.8.6.1 Facial Part
As the facial artery enters the face (Fig. 5.20), it courses tortuously up and forward toward the alar base, lying under the platysma and the fat of the cheek. It ascends passing lateral to the oral commissure in a distance that has been reported to range between 8 and 23 mm (Loukas et al. 2006a; Pinar et al. 2005; Park et al. 1994; Schulte 2001). Most of the time the facial artery is expected to be 1.5–2.0 cm lateral to the oral commissure and running up medial to the nasolabial fold (Fig. 5.21). The range of the distance from the oral commissure where the facial artery can be found is of great importance when designing a Gillies fan flap or a Karapandzic flap for lip reconstruction; the viability of these flaps requires an intact facial artery that must be identified and preserved.
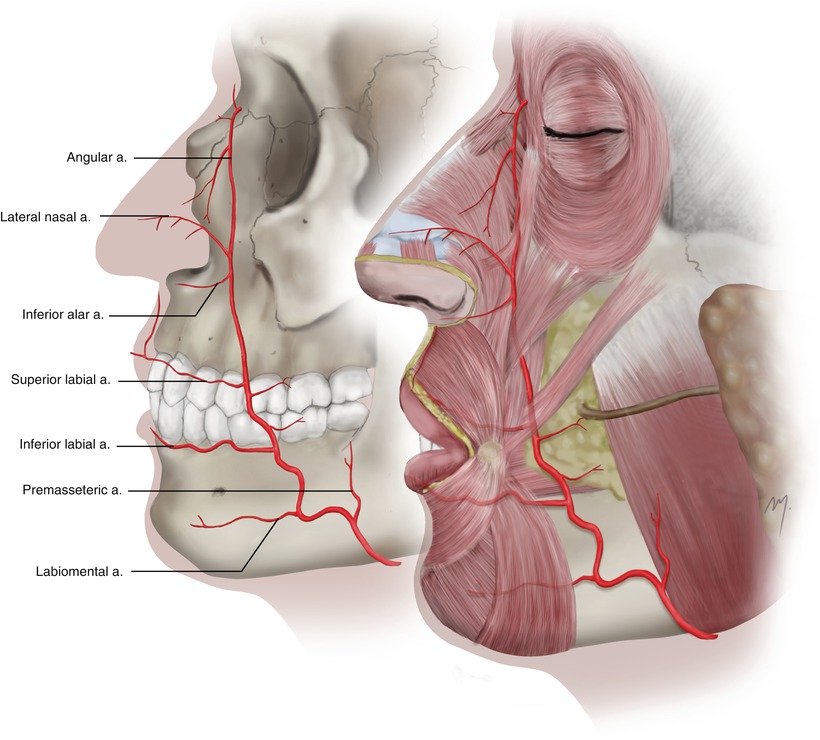
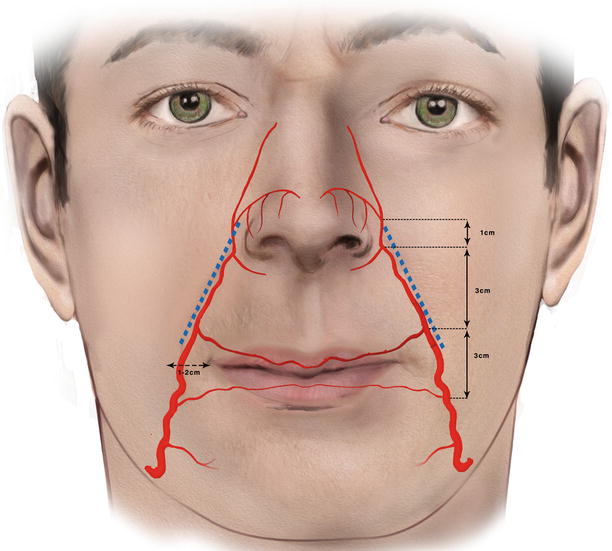
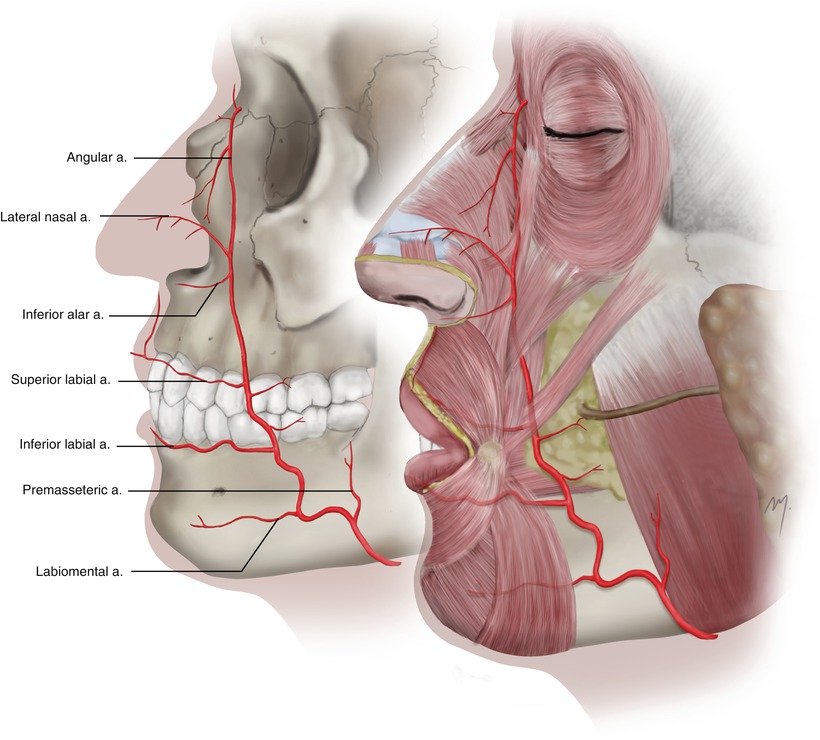
Fig. 5.20
The facial artery at the cheek
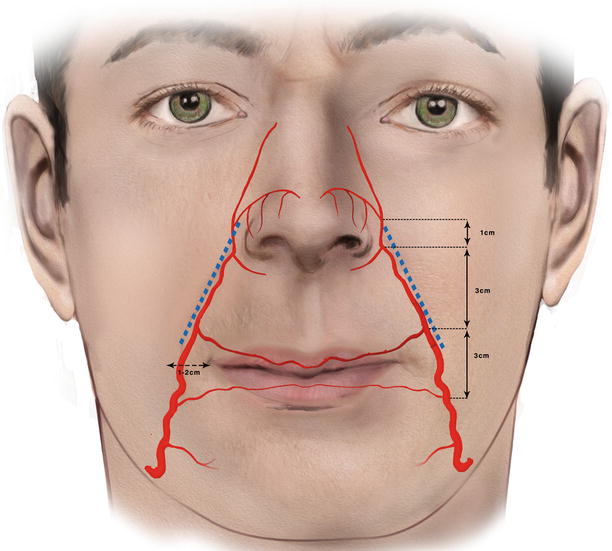
Fig. 5.21
The facial artery passes 1–2 cm lateral to the oral commissure and usually lies medial to the nasolabial fold (blue dotted line). The mean distances of the origin points of the facial artery branches are indicated
Near the angle of the mouth, the facial artery is under the cover of the zygomaticus major (or it may pass through its insertion heads) and the risorius muscles. It is superficial to buccinator and levator anguli oris muscles. Here it gives off small branches to the anterior part of the buccinator and to the zygomaticus major muscles. Above the labial commissure level in the upper lip, the facial artery usually lies medially in relation to the nasolabial sulcus. Turning cephalad, it passes either over or through the levator labii superioris and runs along the side of the nose, usually through the levator labii superioris alaeque nasi, toward the inner canthus, where it anastomoses with the dorsal nasal artery. Partial myotomy of the above superficial muscles must be done to expose the facial artery in cases that it is needed in flap surgery. The buccal fat pad is situated under the artery at this point. The distal and terminal part of the facial artery, after giving off its last branch, the lateral nasal artery, is termed the angular artery.
The branches (Fig. 5.20) given off by the facial part are the premasseteric artery, the labiomental artery, the inferior and superior labial arteries (see Chap. 6), and the inferior alar and the lateral nasal arteries (see Chap. 4). As mentioned above the terminal part of the artery distal to its terminal branch is named angular artery.
The premasseteric artery is a small and not always present branch that arises at the lower border of the mandible and ascends along the anterior border of the masseter muscle. The labiomental artery is an inconstant branch running horizontally to the chin.
After giving off the lateral nasal artery, it ascends along the nasal side, immediately under the skin, giving off small branches and finally anastomoses with the dorsal nasal artery, which establishes the communication between the external and internal carotid arteries.
The mean distances of the points where the facial artery branches originate are shown in Fig. 5.21.
The facial part of the facial artery anastomoses with the mental artery, the transverse facial artery, the infraorbital artery, and the ophthalmic artery (due to the dorsal nasal artery).
The facial artery shows multiple (mean six) perforating branches that supply large areas of facial skin and are more densely located at the level of the commissure (Fig. 5.22).
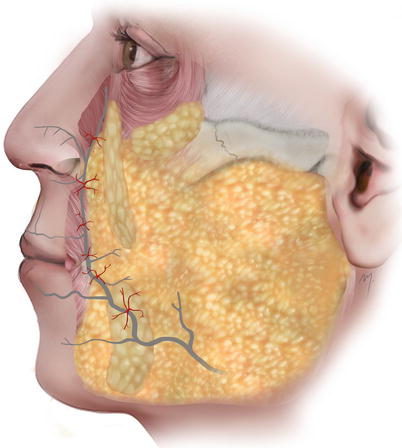
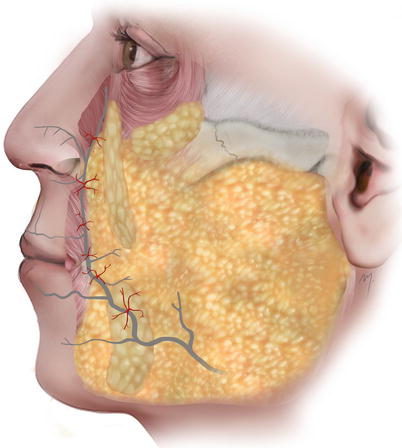
Fig. 5.22
Facial artery perforators to the skin
5.1.8.7 Facial Artery Variations
The variations and the branching pattern of the facial artery have been investigated thoroughly (Mitz et al. 1973; Kozielec and Jozwa 1977; Midy et al. 1986; Niranjan 1988; Whetzel and Mathes 1992; Park et al. 1994; Crouzet et al. 1998; Nakajima et al. 2002; Pinar et al. 2005; Loukas et al. 2006a).
Surprisingly great differences exist, ranging from frequency of types of branching patterns, in their description and nomenclature (specifically regarding the arteries to the nose) among the investigators.
A variation of the facial arteries course is exhibited when the artery is underdeveloped, and thus, the artery does not reach its normal ending point.
In general the result is that each type is missing a subsequent branch starting from the angular artery. Four major types of facial artery exist (Fig. 5.23). The first two types are the most common and represent about the 90 % of cases.
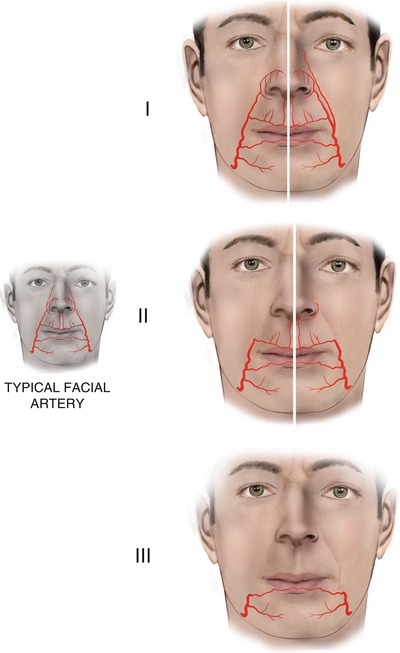
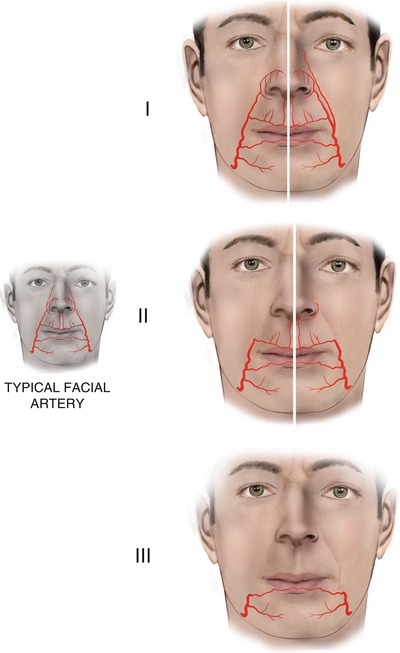
Fig. 5.23
Facial artery variations
5.1.8.7.1 Typical
In the typical form, the facial artery is completely developed and ends with its final angular artery.
5.1.8.7.2 Ending as Lateral Nasal
In this form, the angular artery is absent and the facial artery ends to its lateral nasal branch. In this type, sometimes the angular artery is present as “ectopic.” It arises individually at the level or from a slightly lower point of the commissure and ascends to the inner canthus.
5.1.8.7.3 Ending as Superior Labial
When both angular and lateral nasal arteries are not present, the facial artery ends to the superior labial artery. In these cases, often a “reverse” inferior alar artery is branched from the columellar artery and courses along the inferior margin of the nostril.
5.1.8.7.4 Ending as Inferior Labial
In very rare cases, the facial artery consists, in its facial part, only of the inferior labial artery.
In the various types where the facial artery is underdeveloped, other neighboring arteries of the face—infraorbital, ophthalmic, transverse facial, or even a hyperdeveloped contralateral—assume the role of supplying the area.
5.1.9 Venous Drainage
The small veins of the cheek generally follow the associated arteries and converge to larger ones that drain to the named larger veins of the cheek. The facial vein provides the major venous drainage to the cheek. It appears to the cheek (Fig. 5.24) as continuation of the angular vein running at the side of the nose (see Chap. 4).
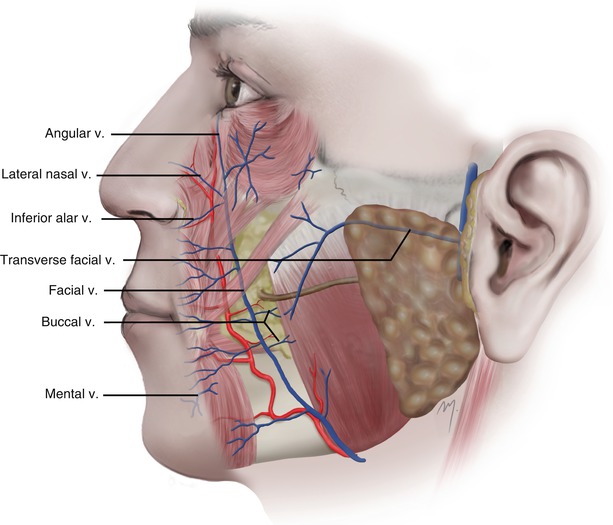
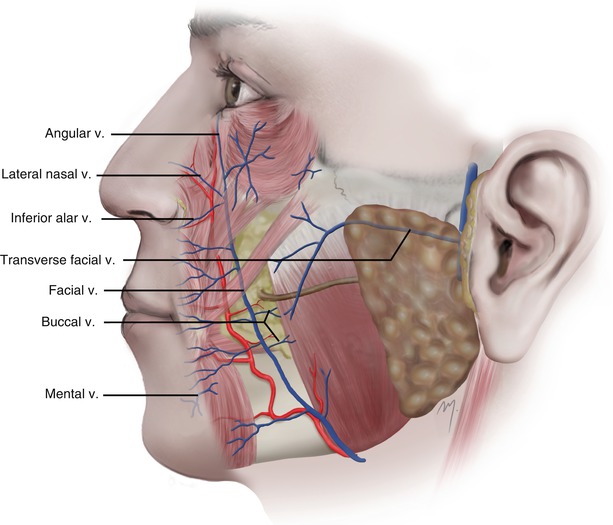
Fig. 5.24
The venous drainage of the cheek
The facial vein continues running within the buccal space lying above the buccal extension of the buccal fat pad. Although the facial vein runs in a same direction as the facial artery it is situated posterior to the facial artery in a variable distance. At the level of the nasal ala the mean distance of the facial vein and artery has been measured to be 16.3 mm and at the oral commissure 13.6 mm (Zhao et al. 2000). As the facial vein proceeds to the lower border of the mandible it approximates the artery and the two vessels run in close proximity. It crosses the lower mandibular border lying beneath the platysma and continues down in the neck where it drains into the common facial vein and the internal jugular vein.
The facial vein at the cheek receives the lateral nasal (superior alar) and the inferior alar veins of the nose, the venae commitante of the lips, and the buccinator and masseteric veins. It communicates also with the infraorbital vein.
The transverse facial, infraorbital, mental, and buccal veins contribute to the venal system of the cheek draining the first into the superficial temporal vein and the next three into the pterygoid venous plexus.
5.1.10 Sensory Innervation
Sensory innervation of the cheek comes from the infraorbital nerve and zygomaticofacial nerve, branches of the maxillary division of the trigeminal nerve, and the auriculotemporal, the mental, and the buccal nerves, branches of the mandibular division, the third and largest division, of the trigeminal nerve (Fig. 5.25). The anterior branch of the great auricular nerve (C2-C3) with its final filaments, contributes to the innervation of the skin of the parotidomasseteric region.
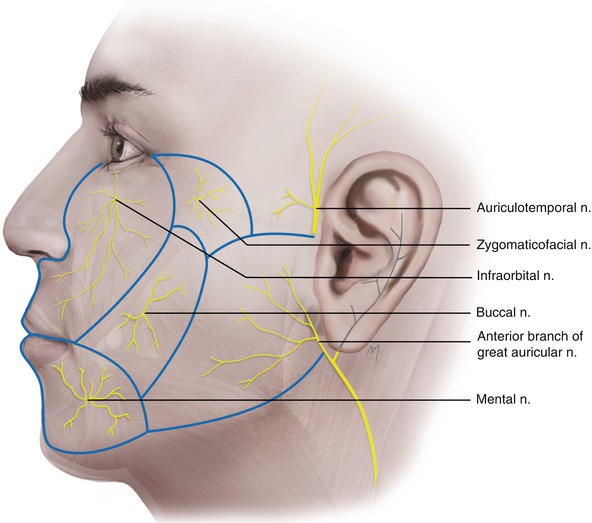
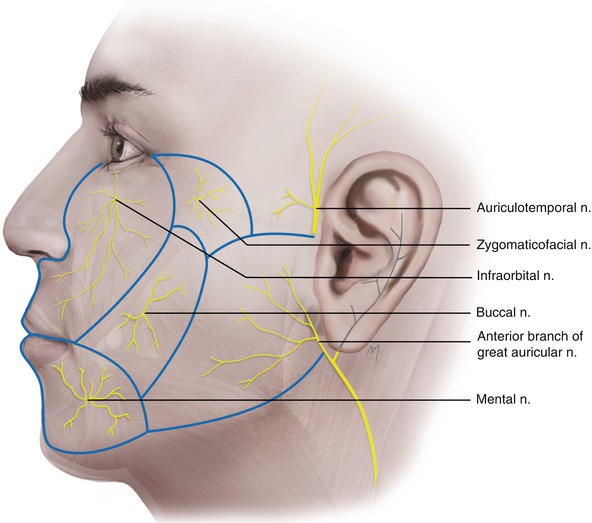
Fig. 5.25
Sensory innervation of the cheek
5.1.10.1 Infraorbital Nerve
The intraorbital continuation of the maxillary nerve just after it passes through the inferior orbital fissure is named the infraorbital nerve constituting actually the terminal branch of the maxillary nerve. It courses on the floor of the orbit along the infraorbital groove in common course with the infraorbital artery and enters the infraorbital canal.
The infraorbital nerve (Fig. 5.26) exits to the face through the infraorbital foramen. It lies under levator labii superioris and over levator anguli oris muscles and divides into its terminal palpebral, nasal, and superior labial branches. The terminal branches of the infraorbital nerve in about 40 % of the cases exit the infraorbital foramen as a completely separated bundle; in the remainder they may be fused and separate after a short course (Hu et al. 2006).
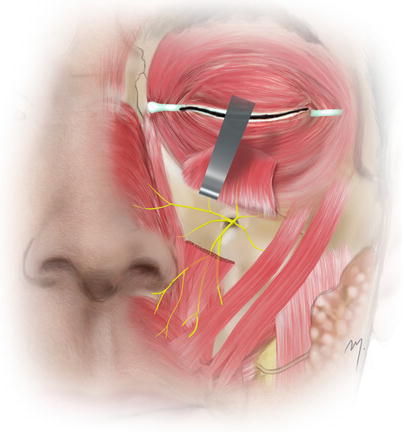
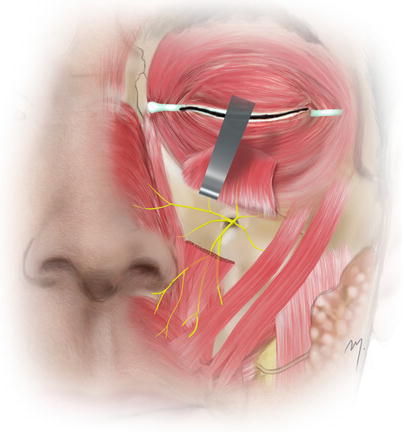
Fig. 5.26
The infraorbital nerve
The palpebral branches of the infraorbital nerve run upward under the cover of the orbicularis oculi muscle, and after piercing it they distribute to the skin of the lower eyelid. Near the lateral canthus, they anastomose with branches of the facial and zygomaticofacial nerves. The nasal branches of the infraorbital nerve distribute to the skin of the lateral side of the nose and to the ala. They anastomose with the external nasal nerve. The multiple superior labial branches are the larger one. They run inferiorly under cover of the levator labii superioris muscle and are distributed to the skin and the mucosa of the anterior part of the cheek and the upper lip. They anastomose with filaments of the facial nerve.
The infraorbital foramen is located at a point usually 8–10 mm below the inferior orbital rim and approximately 25–30 mm from the midline (Fig. 5.27). This point may range between 3 and 15 mm from the inferior orbital rim and between 18 and 33 mm from the midline (Aziz et al. 2000; Chrcanovic et al. 2011).
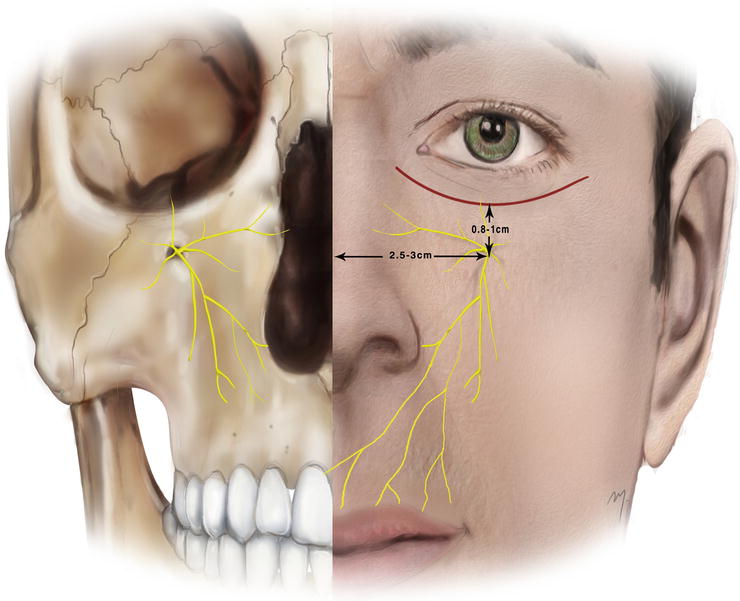
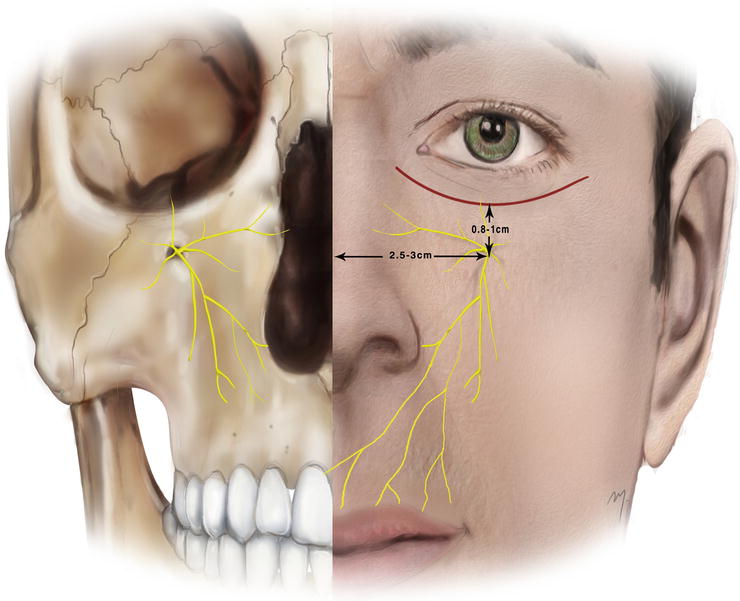
Fig. 5.27
Landmarks of infraorbital nerve
5.1.10.1.1 Infraorbital Nerve Blockade
Excision of small or medium lesions and minor flap reconstruction can be achieved by local or better by regional anesthesia. The infraorbital block provides anesthesia to the half of the upper lip in its whole thickness and can be performed either extraorally or intraorally (Fig. 5.28).
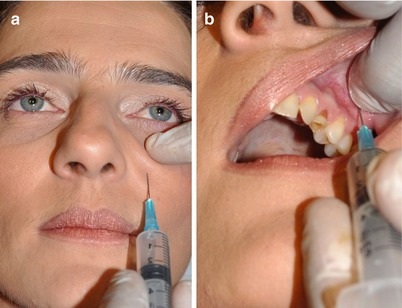
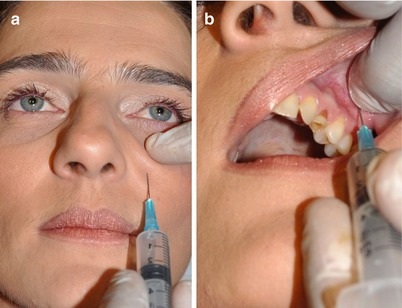
Fig. 5.28
Block of the infraorbital nerve. (a) Extraorally. (b) Intraorally
For an extraoral nerve block, the infraorbital foramen is palpated inferior to the infraorbital rim. If this is unclear, then the point of injection is situated 2.5 cm lateral to the midline and 1 cm below the orbital rim. At this point about 1 ml of local anesthetic solution is injected just above the bone with the needle carried slightly cephalad. Entering the foramen should be avoided because direct injection within the foramen may result in nerve damage.
At an intraoral block of the infraorbital nerve, the needle is inserted slightly lateral to the buccal sulcus above the first premolar teeth. It proceeds upward, parallel to the long axis of the first premolar and targeting the infraorbital foramen. When the tip of the needle is palpated near the foramen, the anesthetic solution is injected.
5.1.10.2 Zygomaticofacial Nerve
The zygomaticofacial nerve is the second of the two branches of the zygomatic nerve along with the zygomaticotemporal nerve (see Chap. 2) that is branched from the maxillary nerve and runs along the inferolateral border of the orbit.
The zygomaticofacial nerve exits the face (Fig. 5.29) through the zygomaticofacial foramen that is situated in the zygomatic bone 2 cm lateral and 2 cm inferior to the lateral canthus. It pierces the overlying orbicularis oculi muscle and distributes in an area to the skin over the prominence of the cheek up to the lateral canthal area. It anastomoses with the zygomatic branches of the facial nerve and the palpebral branches of the maxillary nerve.