Salyer Unilateral Cleft Lip/Nose Repair
Kenneth E. Salyer
DEFINITION
Cleft lip/nose deformity occurs during embryonic development when there is lack of normal migration and proliferation of neural crest cells leading to failure of the facial prominences to fuse.
ANATOMY
Normal Upper Lip Anatomy
The foundation of the face is the facial skeleton. The upper lip is supported by the underlying maxillary and mandibular framework, with its teeth and alveolar bone. Alveolar bone develops and matures with primary and secondary tooth eruption.
The orbicularis oris muscle consists of two well-defined and functional components: the pars superficialis and the deep pars marginalis.
The pars superficialis is located under the skin of the lip and is related to other facial muscles of expression (levator labii superioris, alaeque nasi, and zygomaticus minor), and these retract the upper lip as a group. The pars superficialis consists of an upper and lower bundle.
The upper bundle represents the common insertion of the muscles of facial expression and itself inserts onto the anterior nasal spine, septopremaxillary ligament, and the nostril sill, passing deep to the alar base.
The lower bundle derives its fibers from the depressor anguli oris muscle on each side and decussates in the midline, inserting in the skin and forming the philtral ridges of the contralateral side.
The deep portion of the pars marginalis muscle is responsible for sphincteric action of the mouth and runs under the vermilion from one modiolus to the other.
The two portions of the orbicularis oris muscle thus correspond to the double function of the upper lip. The deep pars marginalis, extending from one modiolus to the other, seals the extrinsic facial muscles to open the mouth as a retractor.
Contraction of the deep pars marginalis, when the mouth is pursed, thickens the vermilion and lengthens the upper lip height. Simultaneous relaxation of the pars superficialis produces perioral fine wrinkles and accentuates the philtral columns while flattening the nasolabial folds.
In contrast, when the mouth is opened, the contraction of the pars superficialis leads to flattening of the perioral wrinkles and philtral columns and accentuates the nasolabial fold. In addition, the upper lip height shortens. Simultaneous relaxation of the deep pars marginalis decreases the thickness of the vermilion.
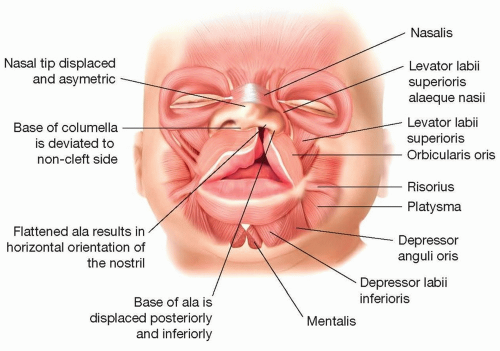
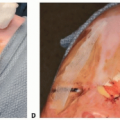
Abnormal Cleft Lip/Nose Anatomy (FIG 1)
Varying degrees of cleft dysmorphogenesis of the lip, alveolus, and palate result in skin, soft tissue, muscle, and skeletal deficiencies with functional and aesthetic imbalance.
This affects nasal symmetry in both complete and incomplete unilateral cleft lip/nose deformity by distorting the position of the ala base and shape of the nostril.
With an interruption of the orbicularis oris muscle in the unilateral cleft lip/nose, the other attached facial muscles pull the ala base more laterally compared to the noncleft side. The existing muscle imbalance also changes the position of the alar cartilage, as well as the orientation of the nostril from an oblique to a horizontal orientation.
When the muscle inserted on the base of the septum and columella is contracted on the noncleft side, the septum and columella is pulled toward that side. Thus, the severity of the cleft nasal deformity depends on the degree of separation of the orbicularis.
Hypoplasia of the lesser segment, or base, of the cleft nose results in the displacement of the lower lateral cartilage laterally and inferiorly on the cleft side. The nasal dome is flattened and slumped in a downward position.
The alar cartilage on the cleft side is flat, giving it the false appearance of having greater length when compared to the contralateral alar cartilage, which also is abnormally displaced to the noncleft side.
The relationship of the lower lateral cartilage to the septum is normal; however, the septum itself is deformed, thereby tilting the base of the nose toward the noncleft side and the tip of the nose toward the cleft side.
The following summarizes a list of characteristics typical of a unilateral cleft lip/nose deformity. The degree and severity of the deformities vary, and not all of them are present in each patient.
The columella is shorter on the cleft side with its footplate displaced and tethered inferiorly.
The base of columella is deviated to the noncleft side.
The medial crus of the alar cartilage is shorter on the cleft side.
The lateral crus of the alar cartilage on the cleft side is longer and, together with the adherent skin, is drawn to an S-shaped fold.
The alar cartilage on the cleft side is displaced in the backward and downward planes.
The nasal tip is displaced and asymmetric, with loss of the defining point on the cleft side.
The dome on the cleft side is obtuse.
The flattened ala results in horizontal orientation of the nostril on the cleft side, and it is usually larger than the opposite side.
The entire nostril is retropositioned.
The base of the ala is displaced posterior and inferiorly where it is tethered to the displaced underlying bone on the cleft side.
The nasal floor is lower or absent on the cleft side.
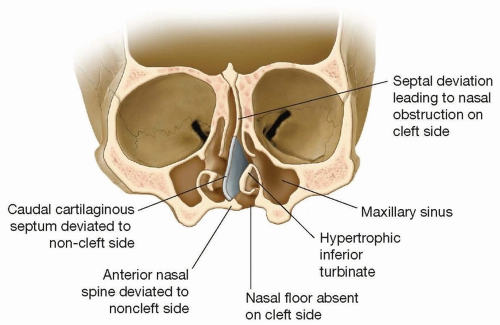
The caudal septum and anterior nasal spine are deflected to the noncleft vestibule (FIG 2).
Septal deviation of varying degrees leads to posterior nasal obstruction on the cleft side due to the deviation of the septum and, often, the narrowing of the internal nasal valve.
The lower turbinate on the cleft side is hypertrophic.
Nasolabial fistula may be present.
The lesser maxillary segment is hypoplastic and displaced on the cleft side.
The nasal pyramid is asymmetric.
PATHOGENESIS
Three major factors influence the nasal deformity in both complete and incomplete unilateral clefts:
Muscle imbalance
Tissue hypoplasia
Asymmetry of the skeletal base
NATURAL HISTORY
Orofacial clefting is the most common craniofacial birth defect, occurring in 1:500 to 1:750 live births worldwide.
The incidence of cleft lip in combination with cleft palate is estimated at 1:1000 with a gender ratio of 2:1 (male to female) with reverse gender ratio for cleft palate only.
In the population of children with cleft lip and/or cleft palate (CL +/- P), approximately 50% have CLP, 30% to 35% CP, and 15% to 20% CL.
Approximately 15% of CLP patients will have a syndrome, whereas 40% of CP patients are part of a syndrome.
PATIENT HISTORY AND PHYSICAL FINDINGS
The diagnosis of a cleft lip and/or palate is made by prenatal ultrasonography or by physical examination at birth and in early infancy. A detailed assessment is made of the child’s breathing, feeding, growth, and development.
Airway assessment must exclude the presence of sleep apnea and micro-/retrognathia.
Assessment of growth and weight is key to identify and monitor feeding difficulty, gastroesophageal reflux, and use of feeding aids (Haberman/Pigeon teat).
Hearing and middle ear function must be assessed and treated early by an otolaryngologist when associated with cleft palate.
The plastic surgeon should define in detail the cleft lip type according to the anatomic structures involved, ie, complete or incomplete, unilateral with or without a Simonart band or bilateral, and presence or absence of a cleft palate.
The child should also be assessed for associated anomalies suggestive of a syndrome, including craniofacial dysmorphia, airway compromise, cardiac defects, ocular and auricular abnormalities, and musculoskeletal anomalies. A genetics referral is suggested if syndromic cleft palate is suspected.
IMAGING
At 16 weeks gestational age or older, 3D, 4D, and HD in utero ultrasound provide early diagnosis readily available in the developed and, in certain places, in the developing world. Parents may seek consultation with experienced surgeons, genetics experts, and other team members for education and decision-making about treatment.
DIFFERENTIAL DIAGNOSIS
One of the main questions to determine in the presence of a cleft lip or cleft lip and palate is, “Does the patient have an isolated, or syndromic, cleft, which plays a major role in prognosis of treatment and genetic inheritance?” Van der Woude syndrome is a prime example, diagnosed with the presence of lip pits and means 50% subsequent inheritance.
If cleft lip and palate are present, then 15% will be syndromic.
Syndromic Cleft Lip and Palate
Stickler syndrome
Robin sequence
22q11.2 deletion syndrome
Treacher Collins syndrome
Nager syndrome
Ectrodactyly-ectodermal dysplasia
Klippel-Feil syndrome
Others
NONOPERATIVE MANAGEMENT
All cleft lip patients should be treated surgically unless in extreme cases where anesthetic risk for surgery is high.
SURGICAL MANAGEMENT
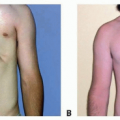
Cleft lip repair is ideally performed at 3 months of age, with the infant weighing greater than 5 kg.
Risks of the procedure are based on the risk of the anesthetic, which is minimal.
Main objectives of the procedure:
Separate the oral and nasal communication
Completely release and restore orbicularis oris function
Reconstruct the lip and nose to restore normal oral and nasal function
Provide an aesthetic result, which is accepted by the society and the patient
Main steps of the procedure:
Mark the lip.
Dissect, release, and mobilize all abnormally displaced structures of the lip and nose simultaneously: muscles of the lip and base of the nose with other abnormal soft tissue attachments including alar and septal cartilage of the nose.
A complete tension-free closure must be achieved, or further dissection is necessary.
Focus on creating 3D aesthetic balance and functional harmony of the lip and nose.
Muscle repair:
The muscle alignment is more important than the design of skin incision in achieving an excellent result.
Repositioning the muscle is one of the keys to achieving a good and stable result whether sub- or supraperiosteal, as this provides the foundation and support of the repair, maintaining alar base and nasal tip projection and symmetry.
To achieve complete mobilization and reconstruction, the complete release of the abnormal attachments of the muscle, and proper alignment, is key. The muscle should be vigilantly aligned.
Any under- or over-rotation of a carefully planned repair is usually due to a malaligned muscle repair.
Nose repair: Correction of the nasal cleft deformity is a necessary and integral part of the primary surgery.
Preoperative Planning
Perioperative orthopedics
Preoperative passive appliance: Hotz of Zurich introduced the use of an appliance placed preoperatively to control the greater and lesser segments, providing guidance for positioning the segments after lip/nose closure. This is left in place to prevent arch collapse until palatoplasty is performed.
Definitive scientific proof that this improves the end result is lacking. Thirty years of experience in Dallas improves the dental skeletal result, maxillary deformity, septal deviation, and other related deformities.
Preoperative active appliance: Nasoalveolar molding (NAM) with active preoperative segmental positioning has become internationally popular and used by many centers and teams. It provides better positioning of the maxillary segments while expanding and positioning the nasal soft tissues. It makes the surgery easier, particularly for the inexperienced surgeon.
Latham’s earlier techniques using active forces were proven to be detrimental to maxillary growth and alignment. Adverse effects on growth need further scientific investigation before the final outcome of all active techniques is known.
In my experience, excellent results can consistently be obtained without adding nasoalveolar molding in the unilateral cleft lip and palate patient. The technique can be labor intensive requiring family compliance and frequent visits to the orthodontist.
With NAM, the molding of the nose must be done carefully to prevent creating a mega nostril through the potential tissue expansion effect, rather than just the desired reshaping of the nostril.
Skin incision.
After three decades of cleft surgery, we believe that the skin incision is not very important in and of itself. The final aesthetic and functional outcome is determined by the extended dissection that allows the surgeon to free all the anatomic elements of the lip and nose that were displaced by the cleft in order to achieve complete repositioning of these elements.
The concept of the Salyer lip/nose repair is one of totally freeing all elements of the lip and nose in a plane above the periosteum, so they are floating free above the abnormal skeletal base.1
The lip and nose elements are then placed in the proper position, visualizing the 3D reconstruction and attempting to make form and function as normal as possible. The aesthetic result always remains foremost.
Repositioning the muscle is one of the keys to achieving a good and stable result, as this provides the foundation and support of the repair, maintaining alar base and nasal tip projection and symmetry. Lining up the muscle is the single most important maneuver in the repair, and it should be vigilantly aligned.
Various techniques today put emphasis on exact preoperative markings, which commits the surgeon. The repair should be fluid, allowing for improvisation and artistry by the surgeon, especially with respect to the nose.
For the first 20 years, I believed that an incision around the alar base was necessary to reshape the ala; however, today, this incision has been entirely eliminated, and we feel it only adds an unnecessary scar.2
Positioning
The infant’s head is stabilized on a small donut-shaped gel headrest placed at the edge of the head of the table.
The surgeon sits at the head of the table operating upside down with the infant’s head almost in the surgeon’s sterile lap slightly hyperextended to provide complete visualization of the infant’s face.
The patient is orally intubated by the anesthesiologist with a prebent tube fixed in the midline providing no distortion to the face or lip with minimal protrusion so as not to interfere with the procedure but provide safe control of the airway.
Approach
Delaire described a subperiosteal approach with a wide dissection and incisional release of the periosteum with anatomic muscle closure.
Supraperiosteal dissection is preferred by most plastic surgeons. We believe that the dissection above the periosteum is less detrimental to growth. Whether this philosophy is totally valid needs to be established.
Preperiosteal dissection offers the advantage of allowing the tissue to move more easily, which is especially important in wider clefts. The analogy can be drawn to a scalp flap, which mobilizes with greater freedom when raised in a preperiosteal (ie, subgaleal) plane vs a subperiosteal plane.
TECHNIQUES
▪ Salyer Unilateral Lip/Nose Repair
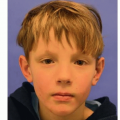
Key identifiable points are marked on the lip and nose (TECH FIG 1A).
The base of each ala is identified and marked using methylene blue or appropriate marking pen. The alar base on the cleft side is usually elongated and distorted compared to the normal side.
The peak of the Cupid’s bow is identified and marked on the normal side. The height of the lip, from the alar base to the peak of the Cupid’s bow at rest and without tension on the noncleft side, is measured using a caliper or is just estimated.
The height to be achieved on the cleft side is usually 6 to 11 mm and averages 7 mm in the 3-month-old.
The midline nadir, or lowest point, of the Cupid’s bow is identified and marked. An equal distance, from the height of Cupid’s bow on the noncleft side to the midline of Cupid’s bow, is used to identify the peak of the new Cupid’s bow on the cleft side and is marked on the vermilion-cutaneous junction.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree