Roux-en-Y Biliary Reconstruction
David Lee
Joohyun Kim
DEFINITION
Roux-en-Y hepaticojejunostomy (RYH) was described by Cesar Roux in 1926 to reconstruct drainage of the esophagus following a total gastrectomy. This configuration of the intestines has been applied for biliary reconstruction following bile duct excision. In the setting of liver transplantation, the RYH is an alternative to the choledochocholedochostomy (CC).
PATIENT HISTORY AND PHYSICAL FINDINGS
A detailed understanding of the patient’s indication for liver transplantation and medical/surgical history determine whether or not to reconstruct the biliary drainage with either CC, RYH, or hepaticoduodenostomy.
Whenever the common bile duct is compromised either by ischemia, dissection, size, or length, RYH provides a safe alternative to CC.
RYH should be used for patients with primary sclerosing cholangitis (PSC).
PSC recurrence following liver transplantation can lead to stricture formation in the remnant common bile duct.
PSC imparts an increased risk for cholangiocarcinoma in the remnant common bile duct.
Some newer evidence suggests these risks are low and CC may be a viable option in a subset of patients with PSC.
In pediatric patients with a history of biliary atresia and prior Kasai procedure, the Kasai Roux limb provides an excellent method for biliary reconstruction in transplantation.
TECHNIQUES
Five considerations need to be made when performing the RYH:
Division of the jejunum
Orientation of the Roux limb
Jejunojejunostomy
Choledochojejunostomy
External or internal drain placement
DIVISION OF THE JEJUNUM
The site of division of the jejunum should permit sufficient length for a tension-free anastomosis for both biliary reconstruction and the jejunojejunostomy.
In general, 20 to 40 cm from the ligament of Treitz is chosen for bowel division.
To minimize spillage, use a linear cutting stapler to divide the jejunum.
Invert the staple line by continuous or interrupted 3-0 or 4-0 sutures. The bowel is a potential source of bleeding in patients with portal hypertension.
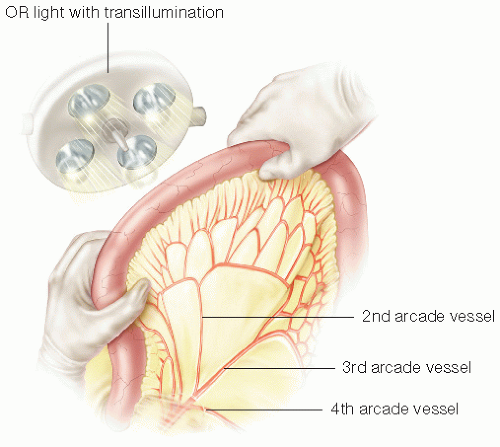
Select the site of bowel division to prevent compromising the blood supply to the bowel, usually between the second and third vascular arcade (FIG 1).
There should be no ischemic discoloration on both sides of the divided jejunum; capillary refill of the bowel wall can be used to confirm viability.
ROUX LIMB ARRANGEMENT
Place the mobilized Roux limb near the bile duct in a retrocolic fashion.
Make a 3- to 4-cm-sized window in the mesocolon to the right of the middle colic vessels. Find the avascular area by palpation, visualization, and careful dissection.
Orient the Roux limb with the antimesenteric border toward the right lateral side.
Close the mesenteric defect with a few interrupted or running 4-0 absorbable or nonabsorbable stitches to prevent internal hernia. If done using the interrupted technique, place the sutures no more than 1 cm apart. Internal hernias are more common in transplant patients due to the lack of adhesion development.
If the patient has dense small bowel adhesions, a hepati coduodenostomy may be preferable.
If the colon mesentery is not suitable for a retrocolic course of the Roux limb, an antecolic position can be used.
JEJUNOJEJUNOSTOMY
Once the Roux limb is confirmed to lay nicely in the porta without tension, perform the jejunojejunostomy.
Make the anastomosis 40 cm from the bile duct anastomosis. If the limb is too short, there is an increased risk of bile reflux and ascending cholangitis. If the limb is too long, there is an increased risk of bacterial overgrowth.
Make the anastomosis 3 to 4 cm of length.
Options for the anastomosis include end-to-side or side-to-side.
For end-to-side, excise the staple line of the proximal jejunal limb. Assure the tip of the proximal limb is oriented toward the enteric stream. The direction of chime is preferable when the tip of the proximal limb is isoperistaltic toward the distal intestine. This theoretically minimizes reflux into the biliary system.
For side-to-side, incise the antimesenteric border of the proximal jejunal limb and sew the anastomosis onto the side of the distal jejunal limb.
This enteroenterostomy can be performed per surgeon preference, although most transplant surgeons do a hand-sewn anastomosis. Anecdotally, fewer bleeding and other complications are seen with this technique. Do a two-layered hand-sewn anastomosis. Create an outer layer of seromuscular Lembert sutures with 4-0 silk stitches. Run a 3-0 monofilament absorbable sutures for the inner layer. For this layer, use a continuous interlocking technique for the posterior wall and Connell stitch for the anterior wall.
Close the mesenteric defect with a running monofilament suture to minimize the incidence of internal hernia.
CHOLEDOCHOJEJUNOSTOMY
The donor bile duct should be prepared.
Trim the bile duct back to fresh, viable tissue. Ligate the 3 o’clock and 9 o’clock bile duct vessels with an absorbable 6-0 suture.
When bile duct size is small, spatulate the duct by incising it in the midline of the anterior wall.
If there is a septum between the cystic duct and hepatic duct, divide the septum to create a single opening.
When there are two bile ducts in a partial liver graft, the two ducts may be approximated in similar fashion if they are near to each other.
Join approximately one-third of the circumference of each lumen.
If needed, spatulate one or both ducts.1
Prepare the choledochojejunostomy by orienting the jejunal limb and deciding the site of the anastomosis.
Confirm there is no tension on the anastomosis.
Make an enterotomy for the biliary anastomosis on the antimesenteric border of the Roux limb. The enterotomy should be a few centimeters from the end of the Roux limb.
When there are two bile ducts, the distance between the two enterotomies should be larger than the distance between the bile ducts.1
Make the enterotomy using a regular or needle tip electrocautery. It can be gently dilated to the appropriate size.
Create the anastomosis using an interrupted approach, sewing the back wall first using a 5-0 or 6-0 monofilament absorbable suture.
Place corner stitches inside out for both bile duct and intestine. Do not tie these sutures and place them on rubber shods. Place the posterior stitches 1 to 2 mm apart and tag them with a hemostat. This may be done by successive bisection or from one corner to the other. Tie the back wall sutures after all are placed with the knots on the inside.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree