Key points
• Thorough analysis of the whole face and the nose, along with full understanding of the nasal dynamics, are required for planning a successful rhinoplasty outcome.
• An optimal rhinoplasty outcome requires congruity between the nose and the rest of the face, as well as harmony among the different aesthetic units of the nose; thus, a circumspect analysis of the entire face is essential.
• Augmentation of the radix on someone who has a narrow, borderline, or even normal intercanthal distance should be avoided.
• A columellar graft advances the subnasale, straightens the distorted medial crura, and rotates the tip cephalically.
• Analysis of life-size images provides a meaningful way of matching the nose to the rest of the face by using soft tissue cephalometric principles.
• When the dorsum is narrow, the eyes may appear closer to each other and widening of the nose may provide an impression of widened distance between the eyes.
• Augmentation of the anterior nasal spine advances the subnasale caudally, resulting in a shortened upper lip, increased tip projection, and a widened nasolabial angle.
• Approximation of the footplates will narrow the base of the columella, widen the nostril opening, advance the base of the columella caudally, and rotate the tip cephalically.
Introduction
The form and dimensions of the nose have an impact on the perception of other features of the face. It is beyond the scope of this book to discuss rhinoplasty in detail; however, it is important for the surgeon to have a thorough understanding of the impact the nose has on the perception of facial form. Planning rhinoplasty is unlike planning of any other procedure in plastic surgery. Unquestionably, the nose is the most unforgiving structure of the face because even a quarter of a millimeter can make a major difference in the outcome of surgery. Another complicating factor in designing successful rhinoplasty is the dynamics of the maneuvers, and this plays a cardinal role in making rhinoplasty enormously challenging. The third factor is the plethora of flaws that can mar the nose; the surgeon requires experience and a keen sight to detect these imperfections. In the order of complexity, the dynamics of rhinoplasty is the most tasking one. However, planning starts with a vigilant analysis. If the flaws are not detected, they cannot be corrected. In this chapter, we will discuss these elements and their details.
Facial assessment for rhinoplasty
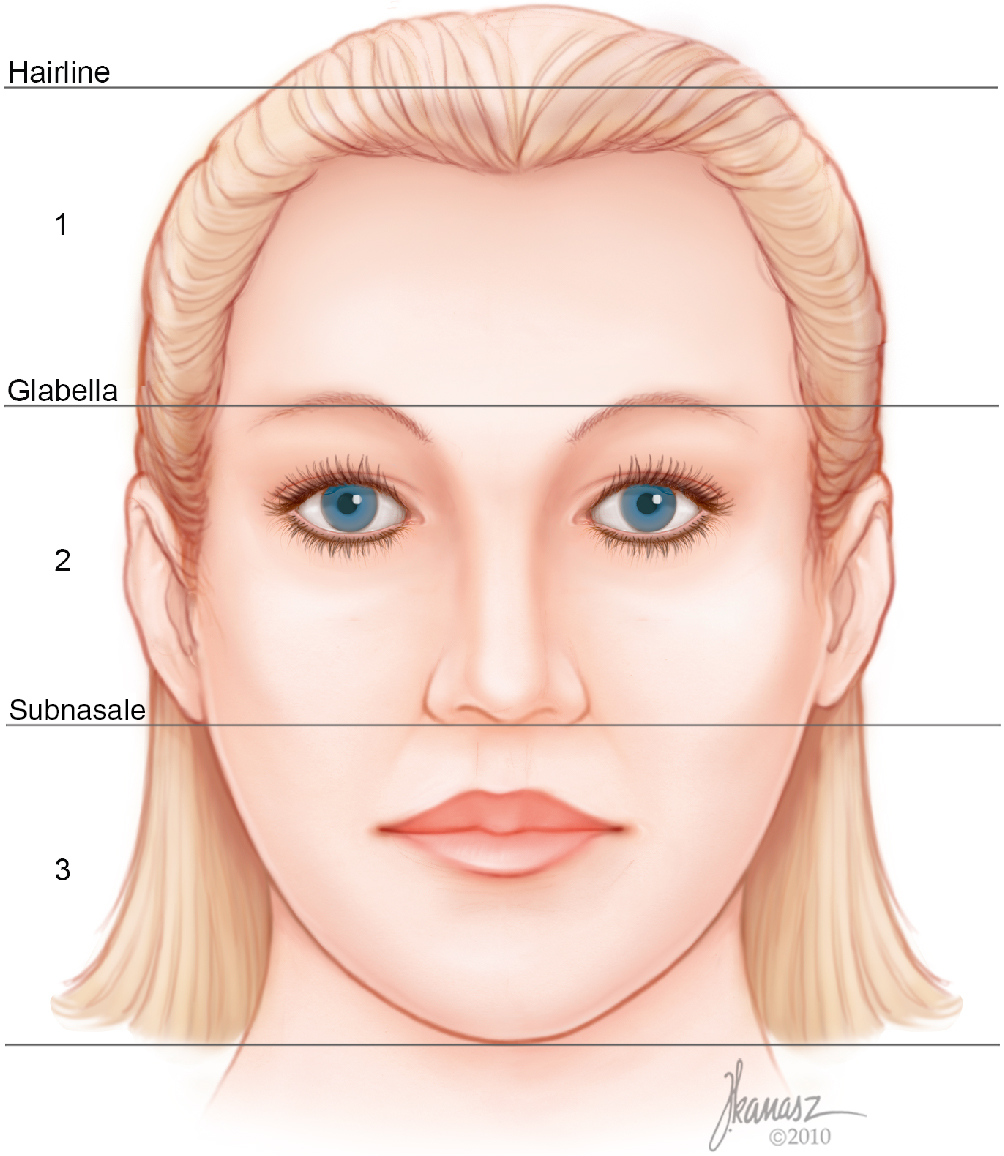
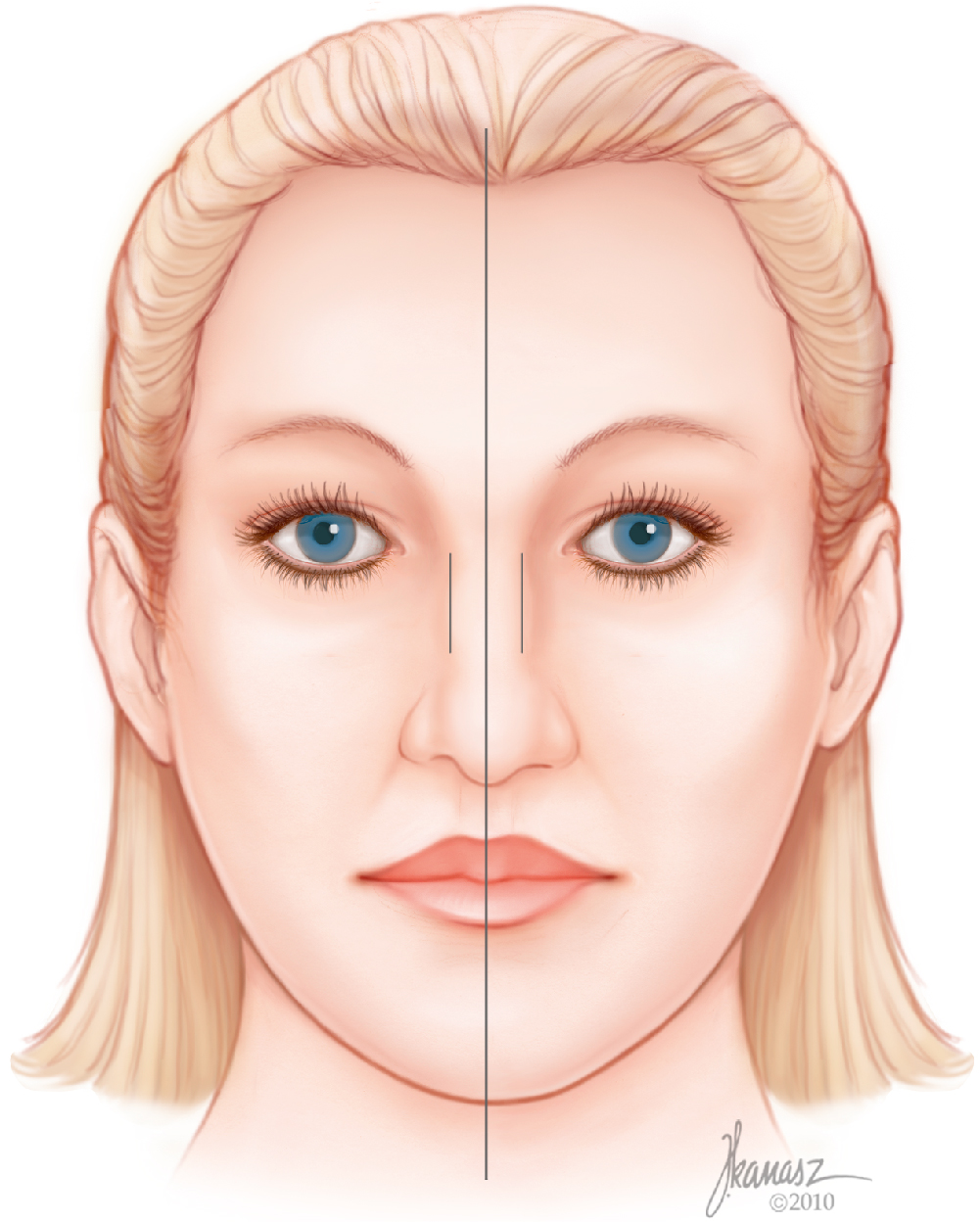
A methodical facial analysis for rhinoplasty requires a systematic and organized analysis of the face leading to detection of other facial as well as nasal flaws. The general features of the face, such as skin quality, color, and consistency, are observed first. Planning rhinoplasty for someone who has thin skin is going to be different from planning one for someone with thick skin. An optimal rhinoplasty outcome requires congruity between the nose and the rest of the face, as well as harmony among the different aesthetic units of the nose. It is for these reasons that a circumspect analysis of the entire face is essential. To ensure careful scrutiny of each segment of the face, one must divide the face into three different zones—upper, middle, and lower—and examine each segment starting from the cranial zone and continuing to the caudal portion of the face. These three zones then are compared with each other ( Fig. 28.1 ). This analysis of the three zones is completed both in the front view and the profile. Because many patients with deviated noses pluck their eyebrows differently, it is important to not use the point bisecting the distance between the eyebrows as a reference point for the facial midline or at least to pay attention to ensure that the eyebrows have not been plucked differently. Patients who have a narrow intercanthal distance should not have radix augmentation because it will produce the appearance of a reduction in the intercanthal distance. Conversely, patients who have an abnormally wide distance between the two canthi would have a positive change resulting from the dorsal and radix augmentation.
The lip position and the amount of incisor show are assessed next because some rhinoplasty maneuvers will influence the show of the incisors and gum. While examining the patient and throughout the visit, the patient is watched to see if the lips are closed on repose or whether they remain open. Many patients who have nasal breathing abnormalities do not realize that they are mouth breathers, and they assume that breathing through the mouth is physiologic and natural. Often, these patients have long face deformity as a result of chronic obstruction of the airway and breathing through the mouth; these factors result in relaxation of the mandible and allows the maxilla to grow excessively and the mandible to rotate posteriorly.
The alignment of the lower face with the midface is also observed and recorded. Patients commonly have lower face asymmetry, which renders proper orientation of the nose with the rest of the face very difficult unless the jaw or chin asymmetry is corrected at the same time through sliding genioplasty, orthognathic surgery, or a combination of both. This observation of facial asymmetry should be brought to the patient’s attention so that optimal alignment of the nose with the other facial structures is not one of the patient’s expectations, should the patient decline correction of this asymmetry. The Reidel’s line is the most reliable reference line for assessment of the chin projection in relation to the lips on the profile. In an ideal relationship, this line touches the most projected portions of the upper and lower lips and the chin.
The submental flaws, such as excess adipose tissues or redundant skin, can adversely impact the outcome of an otherwise properly performed rhinoplasty. It would be logical to point out these imperfections to the patient and explain the rationale for the discussion. However, if the patient is not concerned about them after the discussion, insistence on correcting these should be avoided. It is only after thorough review of the entire facial structures that attention is directed to the nose.
Analysis of the nose
An organized review of the different nose units prevents missing any correctable flaw. The first crucial observation is the aesthetic dorsal lines for width, symmetry, and direction. The width of the radix and the nasal bones will have a substantial role in planning the type of nasal bone osteotomy. For patients who have narrow or normal dorsal lines, it is not necessary to remove a wedge between the nasal bone and the septum. However, this becomes a crucial maneuver in patients with excess distance between the septum and the nasal bones. Otherwise, it would be impossible to move the nasal bones medially.
Asymmetry of the nasal bone is often a reflection of a deviated septum, and in this group of patients, septoplasty may become mandatory even in the absence of posterior deviation of the septum. Anterior deviation of the nose without posterior septal deviation is exceedingly rare. Whenever there is anterior deviation of the nose, there is also some degree of posterior deviation of the septum to the opposite side of the external deviation of the nose. Additionally, the inferior and, sometimes, the middle turbinates ipsilateral to the external deviation are enlarged.
Observation of the mid- and lower vaults may disclose an inverted-V deformity, which invariably denotes medial shift of the upper lateral cartilages, with or without prior surgery. This observation will lead to the proper choice of spreader graft or spreader flap to correct or reduce the potential for the internal valve malfunction. Internal valve dysfunction can be confirmed by asking the patient to breathe through the nose with or without the support of the nostril. The patients will experience increase in the airflow with the support of the valve whenever there is dynamic or static narrowing of the internal valve.
The width, symmetry, and orientation of the lower lateral cartilage are observed in detail. An astute and experienced examiner can predictably visualize the anatomy of the lower lateral cartilages with observation of the surface anatomy and thus plan the corrective maneuvers. Noting the tip width and symmetry is an important part of successful rhinoplasty planning. The amount of nostril exposure is checked on this view and is evaluated in more detail on the profile view. Nostril width and symmetry are carefully examined in all dimensions. It is of paramount importance to observe the nostril width and location in repose and while smiling. Nostril asymmetry, both in size and position, is extremely common and should be detected. In patients with cephalically-malpositioned alar bases, it is important to check the depth of the nasolabial fold. Many patients with higher positioned nostrils have deeper nasolabial fold due to the overactive muscles on that side. This kind of keen observation will assist in planning the release of the levator muscle to improve symmetry and minimize patient dissatisfaction postoperatively. A hanging columella will shorten the upper lip and disturb the harmony of the nasal base.
Examination of the profile of the nose begins with observation of the depth of the radix. However, before making any judgment about radix dysmorphology, it is important to make sure that the forehead is not too prominent (frontal bossing) or receding (often as a result of childhood craniosynostosis). The radix should be about 4 to 6 mm deeper than the glabella, and the deepest portion is often located at the supratarsal crease level. Augmentation of the radix in someone with a narrow, borderline, or even normal intercanthal distance will result in the narrower appearance of the intercanthal distance, and this is invariably is detrimental to facial congruity, except in patients who have a wider-than-ideal intercanthal distance.
The size of the hump and its extent are observed. In patients with asymmetry in the front view, it is prudent to observe the profile from both sides because the hump may appear different on each side in this group of patients. The size of the hump is important because if, on the surgeon’s estimate, it is large enough to necessitate going through the thickness of the nasal roof during its removal, use of spreader grafts or spreader flaps will become mandatory. The larger the size of the cartilaginous hump, the more likely is the use of the upper lateral cartilage as a spreader flap.
The relationship between the tip and the anterocaudal septum is extremely important. Ideally, the tip should be slightly above the dorsum, producing a supratip break. Lack of this break is extremely unfavorable to the tip aesthetics. When the tip falls below the dorsal line in the profile on repose or animation, it is a clear indication that the patient is going to need a columellar strut, tip graft, or tip suspension suture, depending on whether the deficiency is in the columella or the infratip lobule and the amount of the incisor show.
The alar–columellar relationship is enormously important to the nasal accord. , A line extending from the anterior to the posterior limits of the narrow oval outline of the nostril on the profile should create two equal spaces between this line and the caudal border of the alar rim and the caudal border of the columella, each measuring about 2 mm in diameter. If the alar rim distance from this line bisecting the oval is increased, it denotes alar retraction. Increase in the distance between this line and the columella depicts a hanging columella. When this distance is reduced in the cephalic half, it indicates the presence of a hanging ala. When the distance is reduced in the caudal half, it represents a retracted columella. When the footplates are divergent, it results in retraction of the posterior columella only.
It is important to view the nose through the basal view, with the head tilted back. During this examination, one checks the size, form, and symmetry of the nostrils; the direction of the columella, its width, and symmetry; and the projection of the domes. Additionally, in planning the rhinoplasty, it is important to compare the size of the lobule and its proportion to the length of the columella. Ideally, the lobule length should be about 40%, and the columella should be approximately 60% of the distance from the anterior portion of the tip to columella–labial junction. When the lobule is short, the choice for the augmentation is a tip graft. A columellar strut or a tip suspension suture is more suitable when the columella is short. The nostril size should be observed while the patient is asked to inhale forcefully. Often, patients with cephalically-oriented lower lateral cartilages will demonstrate collapse of the lateral nostril wall and thus the external valve.
Furthermore, the internal valve function is checked by asking the patient to inhale, with and without support of the lateral nasal valve with a speculum or a cotton tip, and the difference in the airflow is reported by the patient.
Examination of the face while the patient smiles is crucial. On the front view, the drooping of the tip, asymmetry in width, vertical position of the nostrils, shift of the tip to one side, excessive gum show or inadequate incisor show, and appearance of a horizontal line in the upper lip can be identified. These are invaluable pieces of information that will play a prodigious role in planning rhinoplasty. On the profile view, caudal drooping of the tip is observed while the patient smiles. The tip should remain above the anterocaudal septal angle when smiling. Should the tip fall below this point, it is a clear indication of the need for additional support in the form of a columellar strut, in a patient with an excessive amount of gum show and a short columella. A tip suspension suture or the Fred technique can be used in the patient who has inadequate incisor show.
Analysis of the life-size images provides a meaningful way of matching the nose to the rest of the face using soft tissue cephalometric principles. This helpful tool immeasurably assists in detection of the flaws in the other facial features that may have deleterious effect on the outcome of the rhinoplasty, should they remain undetected and uncorrected. Additionally, the prototype nose phenomenon will be prevented. Figs. 28.2 through 28.9 and Figs. 28.11 through 28.19 show the steps that we use to analyze the life-size images in preparation for rhinoplasty. Figs. 28.10 and 28.20 demonstrate the clinical application of this method of analysis.

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree