IN THIS CHAPTER
- •
Introduction 115
- •
Patient selection 115
- •
Preoperative history and considerations 117
- •
Operative approach 117
- •
Postoperative Care 119
- •
Reverse abdominoplasty with continuous progressive tension suture 121
Reverse abdominoplasty is an unusual yet useful option for abdominal contouring in patients who have primarily upper abdominal soft-tissue laxity. The advantage of reverse abdominoplasty in these patients is that the resection is in the region of the upper abdominal laxity and fullness, and therefore it is more effective in correcting it. The final scar is ideally hidden within the inframammary fold. In addition, the umbilicus rarely needs to be released and re-inset, as the upward pull generated from the reverse abdominoplasty lifts and rotates the umbilicus and periumbilical soft tissue to their original position. The procedure can be combined with breast augmentation, mastopexy/reduction, or with upper and middle back contouring procedures such as a bra-line back lift (see Chapter 13 , Ancillary Procedures).
Introduction
With the exception of endoscopic abdominoplasty, most abdominoplasty procedures involve resection of transverse skin and soft tissue inferiorly and placement of the final scar below or within the bikini or underwear line. Vertical soft-tissue laxity is thus corrected and the final scar is well hidden. Because most patients present with soft-tissue laxity and striae in the lower half of the abdomen, the standard abdominoplasty technique is very effective. Some patients, however, do not fit the classic abdominoplasty body habitus description. These patients may present with mild to significant upper abdominal soft-tissue laxity, relatively little or no lower abdominal laxity, and good lower abdominal skin quality with absence of striae ( Fig. 10.1 A, B ). Upper abdominal tissue resection is more effective at correcting the specific abdominal contour deformity in these patients, and does so by placing the final scar in the inframammary fold, hidden in the inferior border of the bra ( Fig. 10.2 ). This chapter will review important clinical and operative points of reverse abdominoplasty.



Introduction
With the exception of endoscopic abdominoplasty, most abdominoplasty procedures involve resection of transverse skin and soft tissue inferiorly and placement of the final scar below or within the bikini or underwear line. Vertical soft-tissue laxity is thus corrected and the final scar is well hidden. Because most patients present with soft-tissue laxity and striae in the lower half of the abdomen, the standard abdominoplasty technique is very effective. Some patients, however, do not fit the classic abdominoplasty body habitus description. These patients may present with mild to significant upper abdominal soft-tissue laxity, relatively little or no lower abdominal laxity, and good lower abdominal skin quality with absence of striae ( Fig. 10.1 A, B ). Upper abdominal tissue resection is more effective at correcting the specific abdominal contour deformity in these patients, and does so by placing the final scar in the inframammary fold, hidden in the inferior border of the bra ( Fig. 10.2 ). This chapter will review important clinical and operative points of reverse abdominoplasty.



Patient Selection ( Box 10.1 )
Patients who are good candidates for reverse abdominoplasty have skin laxity or poor skin quality in the upper half of the abdomen, or have a significant amount of soft-tissue redundancy in the upper half of the abdomen that will not be adequately addressed by a full abdominoplasty technique. Poor lower abdominal skin quality and the presence of striae is a common reason for patients requesting more traditional abdominoplasty procedures. In most patients the striae are located in the lower half of the abdomen, extending superior to or just above the umbilicus. Much less commonly seen are those patients who present with skin and soft-tissue laxity primarily located in the upper half of the abdomen. These patients are ideal candidates for reverse abdominoplasty, bearing in mind that direct excision is the most effective treatment for soft-tissue laxity.
The relative contraindications for reverse abdominoplasty are in addition to those that pertain to the standard abdominoplasty patient (see chapters on full, extended, and circumferential abdominoplasty).
- •
Excess upper abdominal adiposity without significant soft-tissue laxity
- •
Significant lower or global abdominal soft-tissue laxity
- •
Previous surgery with low subcostal scars that cannot be excised during the reverse abdominoplasty
- •
Poor skin quality with extensive lower abdominal striae
- •
History or concern of hypertrophic/keloid scars in the sternal or parasternal area
- •
Umbilical shape and position that would benefit from umbilicus release and inset with a standard abdominoplasty
Patients with significant lower as well as upper abdominal skin and soft-tissue laxity are best served by a traditional full abdominoplasty, to be followed in the future by a reverse abdominoplasty only if necessary. The full abdominoplasty is usually sufficient to correct both lower and upper abdominal skin and soft-tissue laxity and excess adiposity. We recommend that the staged procedure, if upper abdominal laxity persists, is performed at least 6 months between procedures.
Additional procedures can also be combined with the reverse abdominoplasty. The most common involve procedures performed with reverse abdominoplasty the breasts and those that allow contouring of the upper and middle back. Various breast procedures, including breast lift with or without augmentation, can be performed in combination with a reverse abdominoplasty, as the two procedures will share a common final transverse scar at or above the level of the inframammary fold. Contouring of the upper and middle back can also be combined with a reverse abdominoplasty in the form of a bra-line back lift (see Chapter 12 ). This procedure resects the excess soft tissue of the upper and middle back and places the final scar within the confines of the posterior bra line. This allows correction of the soft-tissue laxity of the middle and upper back that cannot be achieved by the posterior component of a circumferential abdominoplasty because of the strong fascial attachments of the midline zone of adherence. The final scar is placed within the bra line, and the lateral extent of the incision in this case is joined with the inframammary scar from the reverse abdominoplasty.
An additional advantage of the reverse abdominoplasty is that the umbilicus usually does not need to be released and re-inset, as the upward pull is directly opposite to the natural downward drift of the aging process. The force and vector created by the reverse abdominoplasty naturally contributes to the rejuvenation of the umbilicus by raising and rotating the umbilicus and periumbilical soft tissue closer to their original position. When a reverse abdominoplasty is performed with complete myofascial plication from the symphysis pubis to the xiphoid, the umbilical stalk can be divided and then reattached in the ideal position following muscle plication.
Preoperative History and Considerations ( Box 10.2 )
Preoperative evaluation of the reverse abdominoplasty candidate is similar to that for the other abdominoplasty procedures discussed. Fortunately, most candidates are healthy, and are unlikely to be overweight or have a history of massive weight loss. Nevertheless, specific health issues should be addressed as discussed in previous chapters. In particular, smoking, diabetes, pulmonary function, anticoagulation medications, a personal or family history of DVT/PE, and future plans for pregnancy are relative contraindications and must be discussed before proceeding with surgery.
Most abdominoplasty and abdominal contouring patients benefit from a standard preoperative workup. Fortunately, reverse abdominoplasty patients tend to be middle-aged and fairly health conscious.
- •
Smoking cessation/avoidance of nicotine exposure for 6 weeks prior to surgery
- •
Multivitamin daily
- •
Stop aspirin/other blood thinning products with primary care doctor’s permission
- •
Abstain from all dietary/herbal supplements not approved by the surgeon
- •
Basic laboratory work should be tailored to each patient. It may include CBC, Chem 7, and PT/PTT/INR. Nutritional values, including albumin, may be warranted, especially for gastric bypass patients
- •
Medical clearance if needed
- •
Wearing abdominal binder for 2 weeks before surgery
- •
Shower with a gentle antimicrobial soap the night before and day of surgery
Operative Approach
Preoperative photographs are taken with the patient in nine cardinal views, as performed for other abdominal contouring procedures, and markings are made with the patient standing. The midline of the abdomen and the inframammary folds are marked bilaterally. The desired final scar placement should be approximately at the level of the inframammary fold. To achieve this, the upper incision should be placed approximately 1–2 cm above the fold, anticipating some descent of the scar postoperatively.
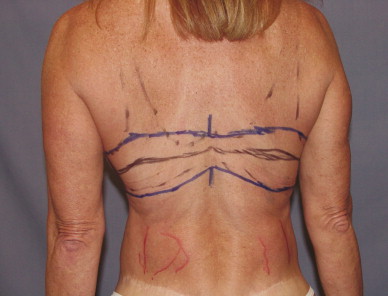
Using the bimanual pinch method, the amount of soft-tissue resection is estimated ( Fig. 10.3 ). This is performed at several points along the incision line, including the anterior axillary point, the mid-portion of the inframammary line, and the midline. The final markings are usually two symmetric ellipses of soft tissue that connect to a narrow area of resection in the midline. The actual length of the transverse resection will be determined by the amount of soft-tissue laxity present. The lateral resection is carried out to the extent needed to prevent dog-ears. If a bra-line back lift is performed concurrently with the reverse abdominoplasty, the lateral and posterior resections should be designed to leave the final scar within the bra line ( Fig. 10.4 A, B ). Outlining the border of the bra is helpful ( Fig. 10.5 ).


The procedure is performed in the supine position unless a bra-line back lift or other posterior procedure is also planned. If a posterior procedure is planned, it is performed first with the patient in the prone position and the patient is repositioned supine for the reverse abdominoplasty. Standard intraoperative precautions are taken, including lower extremity sequential compression devices, warm air blanket, appropriate padding and positioning, and intravenous antibiotics.
With the patient in the supine position, the incision lines are infiltrated with lidocaine containing epinephrine. If abdominal liposuction is planned, tumescent infiltration is performed prior to prepping and draping to allow sufficient time for vasoconstriction to be achieved. Abdominal liposuction is performed first if it is needed. If concurrent breast procedures are planned, these are usually performed before the reverse abdominoplasty.
The incisions for the reverse abdominoplasty are made with a number 10 scalpel into the dermis. The excess soft-tissue laxity in the upper abdomen outlined preoperatively can be de-epithelialized or resected ( Fig. 10.6 ). It is important to note that proper anchoring of the abdominal flap is critical to prevent poor scar formation, as well as descent of the scar below the inframammary fold onto the abdomen. To help ensure this, a segment of de-epithelialized tissue 1 or 2 cm wide along the entire length of the inframammary fold is preserved. This will preserve the inframammary fold architecture and also provide a stronger anchor point for the abdominal flap.

Dissection of the abdominal flap is performed in a manner comparable to standard abdominoplasty techniques except in reverse. The intercostal and subcostal vessels should be protected to maintain this important blood supply to the flap. The soft tissues are elevated off the abdominal wall fascia using electrocautery, and dissection is performed to the umbilical stalk, which is usually preserved. More inferior dissection can be performed if visualization permits, but is usually unnecessary. The superficial epigastric and circumflex vessels are preserved with this technique unless an inferior abdominal resection is also performed.
Myofascial plication is performed in similar fashion to other abdominoplasty techniques using a size 1 or 0 looped nylon suture on a tapered needle. Most candidates for reverse abdominoplasty do not have the global myofascial laxity seen in standard abdominoplasty patients. Nevertheless, myofascial plication is performed as needed from the pubic symphysis to the xiphoid. This is the reverse of the normal abdominoplasty xiphoid-to-pubic-symphysis plication. The generous incision at the inframammary fold allows for excellent myofascial visualization to the level of the pubic symphysis without the need for other access incisions. Should one be necessary, however, it can be made at the level of pubic symphysis or in the mons pubis to conceal the scar. During myofascial plication, the umbilical stalk can be left in place or released and reattached for better visualization.
The upper abdominal soft tissue can be resected at the beginning of the procedure by following the preoperative markings, as is the case when de-epithelialization of the segment is performed, or it can be done near the completion of the procedure using demarcation. A Jackson Pratt drain and a pain pump catheter are used routinely. These usually exit through the mons region, but can be brought out at the lateral extent of the inframammary line if necessary.
Incision closure begins with suspension and anchoring of the abdominal flap using number 0 or 1 Vicryl or polydioxanone (PDS). These sutures anchor the superficial fasciae of both the abdominal flap and the upper incision to the underlying dense fibrous structures of the inframammary fold and periosteum or perichondrium at the level of the fold. Using a longer-lasting suture and strong anchoring techniques is beneficial in reverse abdominoplasty, as the abdominal flap is suspended against gravity compared to the standard abdominoplasty techniques. The skin is closed with 2/0 Vicryl interrupted deep-dermal buried sutures placed every centimeter. Final closure is achieved with running intradermal 4/0 Monocryl. Tissue adhesive is used as a water-impermeable dressing.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








