IN THIS CHAPTER
- •
Introduction 33
- •
Patient Selection 34
- •
Preoperative History and Considerations 34
- •
Operative Approach 35
- •
Concurrent Liposuction 37
- •
Umbilical Considerations 39
- •
Muscle Plication 40
- •
Tissue Demarcation and Closure 42
- •
Postoperative Care 43
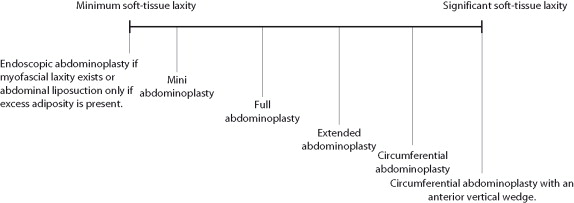
The mini abdominoplasty procedures is highly variable, depending on the clinical findings and patient desire. Such procedures usually encompass a shortened scar, a smaller skin excision, and no umbilical transposition as in a full abdominoplasty. Mini abdominoplasty is ideal for younger patients with lower abdominal soft-tissue laxity that is not significant enough to allow a full abdominoplasty skin resection. Thorough abdominal liposuction is usually an important component of this procedure, as well as strong myofascial plication.
Introduction
The mini or short scar abdominoplasty is an important procedure for patients with mild to moderate skin laxity, excess adiposity, and muscular diastasis. The term mini abdominoplasty is often used to refer to any abdominoplasty procedure where the length of the transverse incision is smaller than that typically used in a full abdominoplasty, as well as avoiding the use of umbilical translocation. The option of a short scar is very appealing, especially to younger women. Even with a short scar, however, excellent myofascial plication and concurrent thorough liposuction can be performed to achieve a very desirable result. The umbilical stalk may be released during undermining and secured or repositioned to the rectus fascia. The umbilicus may be left intact, but this makes supraumbilical myofascial plication more difficult. With this procedure, no external umbilical scar is created and the vertical position of the umbilicus is minimally changed at the completion of the case. The exact length of the transverse incision that designates a mini abdominoplasty is somewhat variable and based on clinical findings, patient desires, and surgeon preference. A mini abdominoplasty involves the removal of a smaller amount of skin and subcutaneous tissue than a full abdominoplasty.
This procedure is much less commonly performed than full abdominoplasty because most patients presenting for abdominal contouring have gained significant weight and/or have had several pregnancies, resulting in significant excess skin laxity, striae, and muscular diastasis. The mini abdominoplasty represents a spectrum of surgical procedures depending on the deformity present.
Introduction
The mini or short scar abdominoplasty is an important procedure for patients with mild to moderate skin laxity, excess adiposity, and muscular diastasis. The term mini abdominoplasty is often used to refer to any abdominoplasty procedure where the length of the transverse incision is smaller than that typically used in a full abdominoplasty, as well as avoiding the use of umbilical translocation. The option of a short scar is very appealing, especially to younger women. Even with a short scar, however, excellent myofascial plication and concurrent thorough liposuction can be performed to achieve a very desirable result. The umbilical stalk may be released during undermining and secured or repositioned to the rectus fascia. The umbilicus may be left intact, but this makes supraumbilical myofascial plication more difficult. With this procedure, no external umbilical scar is created and the vertical position of the umbilicus is minimally changed at the completion of the case. The exact length of the transverse incision that designates a mini abdominoplasty is somewhat variable and based on clinical findings, patient desires, and surgeon preference. A mini abdominoplasty involves the removal of a smaller amount of skin and subcutaneous tissue than a full abdominoplasty.
This procedure is much less commonly performed than full abdominoplasty because most patients presenting for abdominal contouring have gained significant weight and/or have had several pregnancies, resulting in significant excess skin laxity, striae, and muscular diastasis. The mini abdominoplasty represents a spectrum of surgical procedures depending on the deformity present.
Patient Selection ( Box 5.1 )
The ideal patient for a mini abdominoplasty is usually a young woman between the ages of 25 and 50, who has had a number of children but never suffered from significant weight gain. These patients often have mild to moderate excess adiposity, mild to moderate skin laxity, and striae. They are generally relatively thin and their abdominal skin is usually in good condition. Any striae present are usually located in the inferiormost portion of the infraumbilical skin. Myofascial laxity in this patient population is variable.
- •
The ideal mini abdominoplasty candidate has isolated soft-tissue laxity of the lower (infraumbilical) abdomen
- •
These patients may have variable amount of excess adiposity and myofascial laxity, but the skin at and above the umbilicus is usually free of striae
- •
Many mini abdominoplasty candidates may be reasonable candidates for other abdominal contouring procedures, such as abdominal liposuction, endoscopic abdominoplasty, or full abdominoplasty, depending on the degree of soft-tissue laxity and the presence of excess adiposity and myofascial laxity
- •
Appropriate evaluation and discussion with the patient about the anticipated final result and the scars associated with the abdominoplasty are especially important for the mini abdominoplasty candidate
Patients with moderate excess soft-tissue laxity may be candidates for either mini or full abdominoplasty. Because the soft-tissue resection will not incorporate the umbilicus, a full abdominoplasty resection will result in a vertical midline scar (previous umbilical location) at or near the low transverse incision ( Fig. 5.1 ).
Preoperative History and Considerations ( Box 5.2 )
In general, candidates for mini abdominoplasty are usually younger, healthier, and fitter than patients requiring more extensive procedures. However, with all forms of abdominoplasty that include myofascial plication, any personal or family history of deep vein thrombosis (DVT) and/or pulmonary embolism (PE) is very important, and standard precautions should be taken. If this is noted, laboratory testing should be performed to rule out a hypercoagulable state. Basic or specific preoperative laboratory tests may be obtained as indicated by each patient’s medical history. For a healthy patient taking no medications, basic preoperative laboratory analysis should be considered and may include a pregnancy test, complete blood count (CBC), basic metabolic panel (BMP/Chem7), and standard coagulation profiles (PT/PTT/INR). Patients taking birth control medication are at an increased risk of DVT/PE. Discontinuation of such medication 2 weeks before surgery will reduce or perhaps even eliminate this increased risk.
- •
The preoperative evaluation for mini abdominoplasty is comparable to that performed for full abdominoplasty
- •
Although these patients are usually younger and relatively fit, standard preoperative tests are recommended, and additional tests and clearances should be obtained as appropriate
- •
Smoking cessation is important for all abdominoplasty procedures. If the mini abdominoplasty candidate cannot stop smoking preoperatively, omission of concurrent abdominal liposuction should be considered
- •
PE/DVT precautions are the same as for all of the other abdominoplasty techniques. Any history of PE/DVT or other blood clotting disorders should be properly evaluated by a specialist prior to the abdominal contouring procedure
Smoking cessation is an important part of all abdominoplasty procedures, and should be begun several weeks before and continue after the procedure. Cessation of 6 or more weeks is probably ideal; however, patients with a long smoking history will still be at increased risk of ischemia. Those who do not stop smoking should be deferred, or the procedure should be performed in a more conservative fashion, for example a lipoabdominoplasty procedure (see Chapter 6 ).
Patients must understand that although this is a ‘mini’ procedure compared to a full abdominoplasty, the recovery can often be very similar. Oral and transdermal medications are suggested to help prevent postoperative nausea and vomiting.
Operative Approach
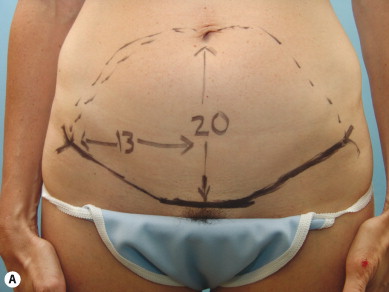
Standard preoperative photographs in nine cardinal views are suggested with the patient standing ( Fig. 5.2 ). The incision for a mini abdominoplasty should be kept as low as possible because there is no concern about removing all of the infraumbilical skin. Whenever possible, the incision should be placed inferior to existing scars so as to eliminate them with the skin resection. The location and length of the incision are negotiable between the patient and surgeon and agreed upon prior to surgery. Normally the patient is asked to forcefully lift the lower abdominal skin and the inferior incision is marked at the level of the symphysis pubis ( Fig. 5.3 ). It then courses laterally toward the anterior superior iliac crest in a natural skin fold. The patient can also be asked to wear revealing swimwear, and the incision can be marked appropriately so that it will be hidden by the garment ( Figs 5.4 and 5.5 ). Preoperative markings should be reviewed by the patient in a mirror before surgery, to be certain that the position and length of the final scar is acceptable.








The primary variable for this procedure is the length of the incision. Patients almost always desire the shortest scar possible, yet their anatomy will often dictate the incision length. Some patients request a short scar abdominoplasty but have moderate skin laxity. A short incision combined with removal of significant amounts of skin can easily be associated with lateral dog-ears, which are undesirable and should be avoided. A physical demonstration of this by bimanual palpation of the lower abdominal skin will demonstrate to the patient the need for a longer incision. Seeing this demonstrated on their own skin is very educational and helps the patient understand the limitations of short scar abdominoplasty. In general, patients tolerate a longer incision in order to achieve an excellent result ( Fig. 5.6 ).

Patients should be counseled that a mini abdominoplasty may not be the ideal procedure for them and a longer incision, or possibly full abdominoplasty, would be more appropriate. If this option is properly presented, patients who could benefit from a full abdominoplasty may become more accepting of the scar, particularly if it can be placed low, where it can be hidden by swimwear or clothing.
Another important consideration for patients requesting mini or short scar abdominoplasty, but who really would benefit from a more significant procedure, is to disclose preoperatively that if the results of a mini abdominoplasty are undesirable, conversion to a full abdominoplasty is possible. Preoperative discussion of the necessary additional costs, recovery, and risks and complications is recommended ( Box 5.3 )
- •
The extent of the abdominal soft-tissue dissection and undermining for a mini abdominoplasty depends directly on the source of the abdominal contour irregularity and the desired aesthetic result
- •
Elevation of the abdominal soft tissue up to the level of the xiphoid is almost always appropriate for proper myofascial plication. Myofascial plication is one of the most important components in achieving a desirable outcome for the mini abdominoplasty
- •
When there is significant abdominal wall laxity, full myofascial plication from xiphoid to pubic symphysis is performed. To accomplish this, the umbilical stalk should be released and dissection completed up to the xiphoid and costal margins
If the degree of abdominal skin laxity is minimal and the majority of the excess adiposity and skin laxity can be corrected by a minimal excision, the incision can be kept short. This is an unusual scenario most commonly seen in younger patients who have never been significantly overweight. Most patients’ deformity in the category of excess adiposity and mild to moderate skin laxity is usually secondary to changes following pregnancy.
Concurrent Liposuction
Once the incision line is drawn, marking should be made for concurrent liposuction that will address all areas of excess adiposity and usually include the entire abdomen, lateral breasts, flanks, and mons area ( Fig. 5.7 ). Liposuction is a key element in the majority of mini or short scar abdominoplasties. Rarely will a patient present without excess adiposity where liposuction will not be a significant benefit. A thorough liposuction of this subcutaneous fat will significantly enhance the final outcome.


Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








