37 Restoration of upper extremity function in tetraplegia
Synopsis
 For people with tetraplegia, restoration of independence is the primary goal.
For people with tetraplegia, restoration of independence is the primary goal.
 Treatment must be individualized because neurologic deficits vary greatly between patients and within individuals (one arm is different from the other).
Treatment must be individualized because neurologic deficits vary greatly between patients and within individuals (one arm is different from the other).
 The hands of people with tetraplegia represent a critical residual resource.
The hands of people with tetraplegia represent a critical residual resource.
 Restoration of function requires a multifaceted approach combining physical therapy, assistive devices, and surgery. including tendon transfer, tenodesis, functional electric stimulation and arthrodesis.
Restoration of function requires a multifaceted approach combining physical therapy, assistive devices, and surgery. including tendon transfer, tenodesis, functional electric stimulation and arthrodesis.
 These procedures have been shown to improve functional independence.1,2
These procedures have been shown to improve functional independence.1,2
 These procedures are underutilized.3
These procedures are underutilized.3
 Strengthening connections between spinal cord injury specialists and upper limb surgeons represents an opportunity to improve access to this care.
Strengthening connections between spinal cord injury specialists and upper limb surgeons represents an opportunity to improve access to this care.
Introduction
Surgery on the upper limb of people with tetraplegia requires special consideration because the hand represents a critical residual resource.4 Their upper limbs take on new functions different from any other patient in that they must “walk on their hands.” Given the importance of the upper limb, surgery must be carefully planned and be the culmination of a long rehabilitative process involving a team. The patient must understand what can be accomplished and realize that the functional improvements will not result in a “normal arm” but as Dr Sterling Bunnell, the father of upper limb surgery in the United States said, “for those who have nothing a little is a lot.”5
Basic science/disease process
Though the upper limb surgeon often does not participate in the initial management of the SCI patient, the acute rehabilitation focuses on the upper limbs. Special care is taken to prevent the onset of contractures of fingers, wrist, or elbow. Even a relatively mild elbow contracture can inhibit independent transfers.6 Fortunately, well-educated therapists are aware of the need for protective splinting right after injury. The shoulder must also be protected as the patient learns to adjust to their injury. Pulling patients, poor posture, or falls can result in shoulder injuries that ultimately limit independence. Indeed the majority of people with tetraplegia have shoulder pain at the end of their acute rehabilitation.7 Early attention to the upper limb provides the best long-term function.
Classification of the tetraplegic upper extremity
Cervical spinal cord injury has been classified in many ways, including by the skeletal level of injury or according to the most distal remaining functioning cervical root. However, this classification system is too general for hand surgeons because no two patients are exactly alike. Injury pattern can differ between those with the same skeletal level of injury and each patient often has different function between the right and left arm. In order to develop useful recommendations for treatment of the upper limb, it was necessary to develop a more precise method for classifying the upper limb in the tetraplegic patient. From these needs arose the International Classification, which is based on the limb’s remaining useful motor and sensory resources (Table 37.1). The motor function assesses the number of strong muscles under volitional control below the elbow. To be counted, the muscle must have grade 4 or 5 Medical Research Council strength. The grade 4 level was chosen because a grade 4 muscle can be transferred with the expectation that it will be able to perform useful work. A grade 3 muscle loses so much of its power in transfer that it cannot be reliably expected to do useful work after transfer.
Table 37.1 International classification for surgery of the hand in tetraplegia
| Sensibility | Motor | Description |
|---|---|---|
| O or Cu group | Characteristics | Function |
| 0 | No muscles below elbow suitable for transfer | Flexion/supination of elbow |
| 1 | Br | |
| 2 | ECRL | Extension of wrist (weak or strong) |
| 3 | ECRB | Extension of wrist |
| 4 | PT | Extension and pronation of wrist |
| 5 | FCR | Flexion of wrist |
| 6 | Finger extensors | Extrinsic extension of fingers, partial or complete |
| 7 | Thumb extension | Extrinsic extension of the thumb |
| 8 | Partial digital flexors | Extrinsic flexion of the fingers, weak |
| 9 | Lacks only intrinsics | Extrinsic flexion of the fingers |
| X | Exceptions |
Caution: it is not possible to determine ECRB strength without surgical exposure. Br, brachioradialis; ECRL, extensor carpi radialis longus; ECRB, extensor carpi radialis brevis; PT, pronator teres; FCR, flexor carpi radialis.
Moberg8,9 also encouraged a consideration of remaining sensory resources as well. If sufficient proprioception remains in any part of the hand (typically the thumb and index fingers), the patient can control his hand without having to keep it in view. If the hand lacks proprioception, the patient can rely on his eyes to direct his hands. However, lack of proprioception limits the patient in performing bi-manual activities. Today static 2-point discrimination of less than 12–15 mm is acknowledged as indicating the presence of proprioception. The International Classification recognizes the presence or absence of proprioception by including codes to indicate whether afferent control resides in the hands, termed “cutaneous, or Cu” or only in the eyes of the patient, termed “ocular, and abbreviated as “O.”
Later, the International Classification scheme was extended to include a determination of the presence or absence of active elbow extension. This system was adopted by the International Federation of Hand Surgery Societies10 and it is used by essentially all surgeons involved in the care of the upper extremities of these patients.
Patient presentation and patient selection
Forming a team
Moberg stressed the need to develop a “critical mass” of likeminded professionals into a team that should include physiatrists involved in the rehabilitation and long-term care of people with tetraplegia. Critical to the success of an upper limb team are well-trained therapists, either physical therapists or occupational therapists (preferably both). The hand and upper extremity surgeon provides the technical expertise. Others including social workers and psychologists may offer additional support to the team. The patient’s support group including family or attendant is the key to success. The central member of the team is the patient.11–13
The hand and upper extremity team should become part of the routine evaluation of even newly injured patients. The cervical cord injured patient arrives at a rehabilitation facility or spinal cord injury unit usually with fairly supple upper limbs though with no or only minimal volitional movement. Once the patient’s vertebral injury has become stabilized and the patient can be up in a wheelchair, an assessment by the upper extremity team takes on new meaning. By the 3rd or 4th month following injury, the eventual functional level is usually clearly established for the majority of patients.14 At this time, the patient’s upper limb function is assessed and the therapist help decide what assistive devices are appropriate.15–17 For some patients early use of a functional orthosis such as a wrist-driven flexor hinge splint will advance the rate of rehabilitation. For patients with early but weak recovery of wrist extension, the wrist-driven flexor hinge splint represents an excellent exercise therapy directed towards strengthening wrist extensors so that they may eventually actuate a surgically reconstructed pinch or grip.
Hand or upper extremity surgery is rarely indicated during the initial months of rehabilitation following injury. The patient needs time to experience neurologic, psychologic, and social stability. From a practical standpoint, there are simply too many more important rehabilitation activities going on. On the other hand, a dogmatic philosophy embracing tired dicta such as “never operate on a patient before 12 months” has no basis in science. Some patients are clearly candidates for surgery prior to this calendar date. For example, early surgical intervention to relieve the pathologic effects of a fixed elbow flexion contracture may allow a patient to participate more vigorously in necessary rehabilitation activities.6 Early release of a fixed elbow flexion contracture can be done with a simultaneous transfer of the contracted biceps muscle to the triceps. This removes a pathologic or deforming force and reinforces or restores some power to the antagonist. Botox is another important tool in the early rehabilitation armamentarium. It is especially helpful for patients with concomitant brain injury who may not comply with splinting or therapy and have increased tone.
Once the patient has achieved neurological and psychological stability, a formal evaluation to establish the appropriateness of upper extremity surgery can be accomplished by the team. The evaluation should focus on both tangible evidence of recovery by assessing remaining motor and sensory resources and the important intangibles such as motivation and intelligence. There is increasing recognition of the co-occurrence of traumatic brain injury with spinal cord injury and the impact of brain injury on rehabilitation.18 Cognitive deficits need to be understood before embarking on upper extremity reconstruction given the intensive post-surgical therapy. The initial patient assessment should include an evaluation on how the patient accomplishes tasks of daily living with particular attention to how he or she performs transfers and pushes a wheelchair (Fig. 37.1). Tendon transfers may alter the position of the hand and fingers. After reconstruction wheel chair propulsion and bed transfers must be performed in a safe manner to prevent stretching of the repairs (Fig. 37.2). It is best for patients to learn safe transfer and propulsion techniques before surgery.
The upper limb examination includes assessment of residual motor groups as well as the identification of pathologic conditions such as contracted, painful, or unstable joints. There is also a sensory evaluation, which includes measuring 2-point discrimination in the digits to assess proprioception. The currently used grip patterns are assessed (Fig. 37.3). Occasionally, spinal cord injured patients will have focal areas of severe neuropathic pain that will make the exam painful and potentially limit surgical results.
Treatment/surgical technique
General guidelines for reconstruction
Four surgical procedures are applicable for improving upper limb function in tetraplegia:
1. Arthrodesis: permits stabilization of joints lacking muscle stabilization
2. Tenodesis: performed either to stabilize a joint or more commonly so that another, typically more proximal movement, e.g., wrist extension, will result in the tightening of the tenodesis and movement of a more distally located joint
3. Tendon transfer: the transfer of the power of an expendable muscle-tendon unit under good volitional control to compensate for the absence or ineffectiveness of function of another muscle-tendon unit.
4. Functional electrical stimulation or FES: this technique utilizes the residual contractile properties of upper motor neuron paralyzed muscles when stimulated by an extra neural source. FES allows for more the use of more residual muscles in the reconstructive plan. At this time, FES is not commercially available.
Surgical reconstruction
Elbow extension
Without active elbow extension, the tetraplegic’s hands frequently fall into his face when lying supine, which makes eating and daily hygiene challenging (Fig. 37.4). One cannot push a manual wheelchair up any incline without triceps function. Even as simple a task as turning on a room light switch may be impossible without active elbow extension. There are two surgical procedures advocated for restoring active elbow extension, biceps to triceps and deltoid to triceps transfer.
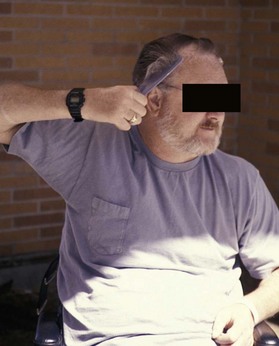
Fig. 37.4 Postoperative elbow extension allowing for stabilization of the arm to assist with combing the hair
Biceps to triceps transfer
This procedure19–21 has become increasingly popular.22 It is the procedure of choice when there is a pre-existing flexion contracture of the elbow greater than 45°. In this case, the biceps is usually a deforming force that must be addressed. The advantages of biceps to triceps transfer include no need for an interposition graft and only one tendon repair site. Disadvantages include a more challenging rehabilitation program and the potential for loss of elbow flexion strength.
Surgical technique
The biceps tendon is detached from its insertion on the greater tuberosity of the radius, the muscle-tendon unit routed either medially23 or laterally,24,25 and the tendon attached to the triceps aponeurosis or directly into the olecranon.
The incisions that are employed depend in large measure on whether a wide exposure to the anterior aspect of the elbow joint is needed to allow adequate release of contracture. The distal extent of the incision should allow complete dissection of the tendon of the biceps so that it can be detached as close to its point of insertion on the bicipital tuberosity of the radius (Fig. 37.5A).
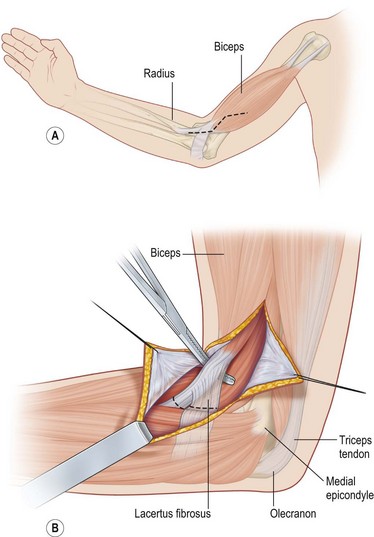
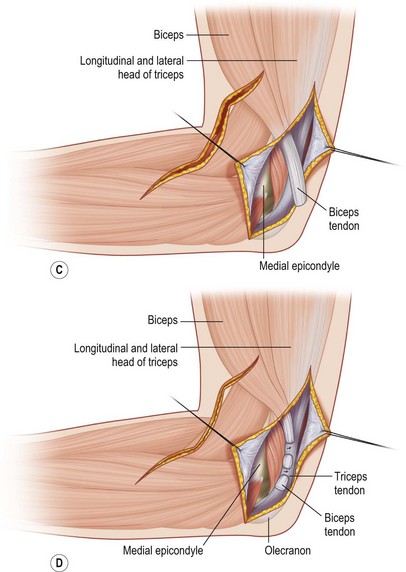
Fig. 37.5 Biceps to triceps transfer by the medial route (A–D).
(Redrawn from Hentz V, Leclercq C. Surgical Rehabilitation of the Upper Limb in Tetraplegia. London: Harcourt Health Sciences; 2002, with permission.)
The incision is carried through the subcutaneous tissue, protecting the large tributaries of the basilic and cephalic veins. The soft tissues overlying the lacertus fibrosis are elevated and the lacertus is either divided off the primary tendon or dissected distally as far as possible to provide another point of fixation to the triceps (Fig. 37.5B).
A second incision located posteromedially is made in order to expose the medial aspect of the triceps insertion. Through this incision, the medial border of the triceps is elevated and dissected to its insertion on the olecranon. The biceps muscle and tendon are then passed from the anterior to the posterior incision through the widely dissected subcutaneous tunnel (Fig. 37.5C). The anterior incision may be closed at this point.
The biceps tendon typically just reaches the tip of the olecranon but there is infrequently sufficient tendon length to permit a strong attachment into the olecranon. Instead, the tendon of the biceps is woven into the medial border of the triceps tendon and anchored in multiple locations with stout sutures (Fig. 37.5D). We have judged that the proper tension is achieved when the biceps is pulled distally enough to permit the end of the tendon to touch the olecranon with the elbow in about 20° of flexion. Once the tendon-to-tendon junctures are made, the elbow is fully extended to relax the site of approximation.
Postoperative care
The initial cast is left undisturbed for 3.5 weeks if the elbow had essentially normal passive extension preoperatively. If the elbow had a preoperative flexion contracture between 15° and 30°, the elbow is extended as much as possible at the time of surgery and casted in that position. This cast is removed between 10 and 14 days postoperatively. Great care must be taken to keep the elbow extended during this maneuver. Typically, the elbow can then be further extended at this time by slow stretch and the arm is recasted, now typically in near full or even full extension. After removal of the cast, the elbow is exercised for several additional weeks by allowing progressively greater elbow flexion in a specially designed flexion-stop brace (Fig. 37.6). Although the biceps seems to be an antagonist to elbow extension, by teaching the patient to conjointly supinate the forearm and extend the elbow, the patient can be reeducated to use the supinator function of the biceps to extend the elbow. Electrical stimulation and biofeedback therapy has been used on occasion with improved results. Some months of cautious use are necessary to prevent overstretching of the transfer and many months pass before maximal strength is obtained.
Deltoid to triceps transfer26
Surgical technique
Hints and tips
1. Detach the deltoid from the humerus with as much fascia and fibrous insertion as possible, including some of the fascial origin of the brachialis muscle.
2. Attach the deltoid to the triceps at maximum tension with the shoulder abducted 30° and the elbow flexed at 30°
3. Cast elbow in full extension and keep the arm abducted at the shoulder during healing.
The surgical landmarks (Fig. 37.7A) at the level of the shoulder include the tip of the acromion superiorly, the interval between the posterior margin of the deltoid and the triceps muscle posteriorly, and the estimated point of insertion of the deltoid on the humerus. The landmark at the level of the elbow is the tip of the olecranon. The surgeon should keep in mind the neurovascular anatomy of the region including the course of the axillary nerve and the circumflex humeral artery and the radial nerve and its relationship to the insertion of the deltoid (Fig. 37.7B).
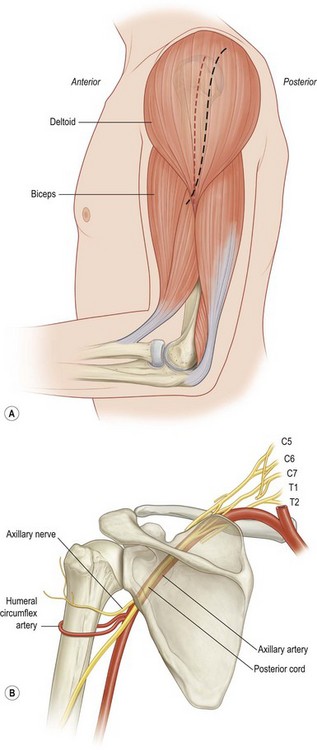
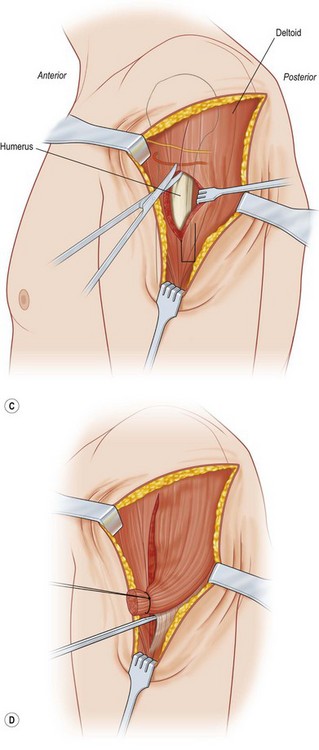
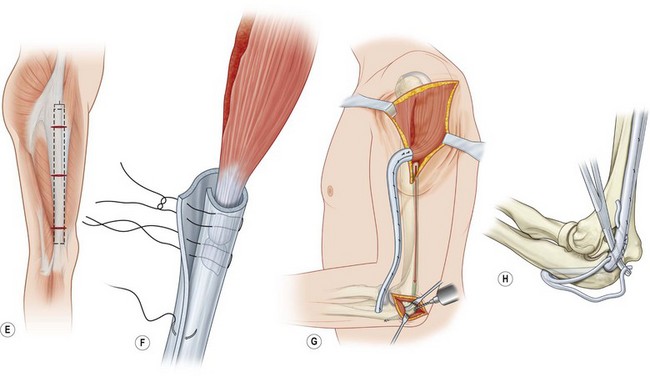
Fig. 37.7 The author’s preferred technique for deltoid to triceps transfer (A–H).
(Redrawn after Hentz V, Leclercq C. Surgical Rehabilitation of the Upper Limb in Tetraplegia. London: Harcourt Health Sciences; 2002, with permission.)
The upper incision is centered half way between the mid-axial line of the humerus and the posterior margin of the deltoid (Fig. 37.7A). The skin incision is carried to the level of the muscle fascia and the skin and subcutaneous tissues are elevated anteriorly to just past the mid-axial line of the humerus. Posteriorly, the skin flap is elevated to the confluence of deltoid and the long head of the triceps (Fig. 37.7C). The plane between these two muscles is developed by sharp or finger dissection. As the finger strikes the humerus, the fingertip tip can be insinuated upward through the fibers of the deltoid, separating the muscle into relatively equal anterior and posterior halves.
A suture is placed in the fibrous origin of the posterior half of the deltoid muscle and the dissection is carried superiorly until the branches of the axillary nerve are visualized (Fig. 37.7D). The superior dissection should stop at this point.
• Autogenous tendons such as toe extensors,27 tibialis anterior tendon,9 or extensor carpi ulnaris28
• A turned up strip of the central part of the triceps tendon with synthetic reinforcement29
We prefer the patient’s own fascia lata, especially in the patient whose triceps tendon is relatively short or insubstantial.32
The fascia is harvested through several transverse incisions placed over the iliotibial band (Fig. 37.7E). The ideal width is about 2.5 cm. The fascia lata is encircled about the fibrous insertion of the deltoid using mattress sutures of nonabsorbable braided suture (Fig. 37.7F), tubed over its remaining length and tunneled subcutaneously to the olecranon.
The olecranon is exposed just distal to the insertion of the triceps. The triceps tendon is split longitudinally to further expose the tip of the olecranon and a 5 mm drill bit is used to create an oblique tunnel through the olecranon (Fig. 37.7G). A Bunnell tendon-stripper is a useful instrument to “polish” this channel so that the tubed fascia lata can be passed smoothly in a proximal to distal direction (Fig. 37.7H).33 The fascia lata is passed into the distal exposure, separated into two tails and the tails are passed through the bone channel.