23 Repair of unilateral cleft lip
Synopsis
 Presurgical nasoalveolar molding.
Presurgical nasoalveolar molding.
 Modification of surgical techniques
Modification of surgical techniques
 Postoperative maintenance of over-correction with silicone nasal conformer.
Postoperative maintenance of over-correction with silicone nasal conformer.
Introduction
Central and foremost, the multidisciplinary approach is essential to the satisfactory treatment of the cleft patients.1 This includes surgeons, orthodontists, speech pathologists, pedodontists, prosthodontists, otolaryngologists, social workers, psychologists, as well as a photographer. In addition, the center’s coordinator serves to coordinate all these specialties for the benefit of the patient as well as for gathering and recording vital information. All of these contribute to the care of cleft patients from infancy to adulthood. This is a time when lasting friendships and care contribute to the psychological, aesthetic, functional, and spiritual development of the person. The techniques presented here are based on the experience of the members of the Chang Gung Craniofacial Center over a period of 30 years in a Chinese population. They have also been tested in other racially diverse centers. The improved outcomes result from an integrated approach with presurgical management, surgical refinements and postsurgical maintenance.
Basic science/disease process
Prenatal diagnosis
Ultrasound examination for the diagnosis of prenatal anomalies and problems is common in many countries, and is helpful in the identification of serious fetal problems as well as cleft lip or palate. Prenatal diagnosis of cleft lip is usually made after 16–20 weeks’ gestation. The detection rate has increased in recent years.2–4 With the advancement of three-dimensional ultrasonography, visualization of the cleft lip has become more accurate.5,6 The three-dimensional image is helpful for prenatal counseling because parents can visualize the face of the fetus clearly. It is important for the surgeon to take time and provide information regarding the treatment protocol and outcomes to the parents. In addition to professional counselors, cleft patients or their parents can personally explain how children with clefts can become normal functioning persons in society.
Genetics
The genetics of orofacial clefting are only partially understood; however, they are of great importance when counseling affected families. It is generally believed that isolated cleft palate is a genetic entity distinct from unilateral cleft lip with or without cleft palate.7–9 This conclusion arises from both epidemiologic studies and the fact that embryologic events leading to cleft lip/palate and cleft palate occur at somewhat different times (3–7 weeks versus 5–12 weeks). It has long been assumed that both genetic and epigenetic factors play important roles in the etiology of clefts, and this is supported by the varying incidence of clefting with ethnicity, geographic location, and socioeconomic conditions.10–12 Twin studies have clearly demonstrated a genetic basis for cleft lip/palate, with a 43% pairwise concordance rate in monozygotic twins versus a 5% concordance in dizygotic twins.7,13,14
The incidence of cleft lip/palate in white newborns is approximately 1 in 1000 (Table 23.1); isolated cleft palate occurs in about 0.5 in 1000. Annual reports in Taiwan indicate an incidence of 0.81–1.62 per 1000 for cleft lip with or without cleft palate and 0.47–0.66 per 1000 for isolated cleft palate.10 While there are more than 250 syndromes associated with orofacial clefting,11 most cases occur as an isolated abnormality; so-called nonsyndromic cleft lip/palate.10 Given the incomplete understanding of the genetics of orofacial clefting and the imprecision in employing nonsyndromic versus syndromic nomenclature, estimates vary regarding the frequency of other malformations in children with clefts. In a large review of their center’s experience, Rollnick and Pruzansky16 identified other malformations in 35% of cleft lip/palate patients and 54% of cleft palate patients. Cleft lip/palate has an unequal gender distribution, favoring boys over girls, whereas this relationship is reversed in cleft palate only.17 Cleft lip/palate affects the left side more often.18,19
Table 23.1 Incidence of cleft lip/palate in differing ethnic groups
| Ethnicity | Incidence per 1000 births |
| Amerindian | 3.6 |
| Japanese | 2.1 |
| Chinese | 1.7 |
| White | 1.0 |
| African-American | 0.3 |
Data from Wyszynski DF, Beaty TH, Maestri NE. Genetics of nonsyndromic oral clefts revisited. Cleft Palate Craniofac J 1996; 33:406–417.15 and Vieira AR, Orioli IM. Candidate genes for nonsyndromic cleft lip and palate. ASDC J Dent Child 2001; 68:229, 272–279.12
Unaffected (i.e., noncleft) parents who have one child with cleft lip/palate have an estimated recurrence risk of 4%, which rises to 9% with two affected children. If one parent is affected, the risk of having a child with cleft lip/palate is also 4%, increasing to 17% if there is already both an affected parent and an affected child.20 As the degree of familial relationship increases, recurrence risk decreases: first-, second-, and third-degree relatives have 4%, 0.7%, and 0.3% risk, respectively.15 Recurrence risk increases with the severity of the cleft.21
The most appropriate genetic model for the inheritance pattern of nonsyndromic cleft lip/palate is a matter of considerable debate, and consensus has not been achieved. Classically, Fogh-Anderson proposed the idea that cleft lip/palate was transmitted by a gene of variable penetrance that could act dominantly or recessively, depending on the individual.7,15 Multifactorial and multifactorial/threshold models have been widely advanced22 and have predominated; others believe there is little evidence to support the concept of transmission as a discontinuous threshold trait.10 In the past decade, the prevailing method of genetic analysis of cleft lip/palate has been by allelic association, whereby “candidate” genes are selected on the basis of functional properties, expression pattern, chromosome location, or mouse homologues.22 Numerous studies of this type have found significant association to the transforming growth factor-α (TGFA),23 transforming growth factor-β3 (TGFB3),24 retinoic acid receptor-α (RARA),25 homeobox gene MSX1,24 and BCL3 proto-oncogene26 loci. Although such studies are useful, their results must be interpreted with caution; it is not clear whether the ever-increasing implicated loci are truly representative of a large number of genes involved in the etiology of cleft lip/palate or whether this type of analysis has the ability to produce false-positive results.15,22 The subtleties of the interplay between genes and environment in cleft lip/palate are yet to be uncovered, and new tools such as sophisticated linkage disequilibrium approaches may be needed to unravel these complexities.15,22
Classification of the clefts
Veau27 suggested that all clefts be classified into four groups: group 1, cleft of the soft palate only; group 2, cleft of soft and hard palate; group 3, unilateral cleft of lip and palate; and group 4, bilateral cleft lip and palate. This simple classification has ignored the clefts of primary palate only and failed to separate the incomplete from the complete clefts of lip and palate.
Kernahan28 reported the Y classification. The upper limbs represent right and left sides of the primary palate, that is, the lip, the alveolus, and the hard palate anterior to the incisive foramen. The lower limb represents the hard and soft palate posterior to the incisive foramen. The limitation of the Kernahan Y classification is that clefts of the secondary palate cannot be classified into right or left sides. The Y classification was modified (Fig. 23.1) into a better numeric system that allows a more accurate recording of all left or right clefts of the primary and secondary palate and is easily adapted to the computer.29,30 In the modified Y classification, each right or left limb is assigned a number, 1–5 or 11–15, for the primary palate and 6–9 or 16–19, for the secondary palate, with 10 being a submucous cleft palate.
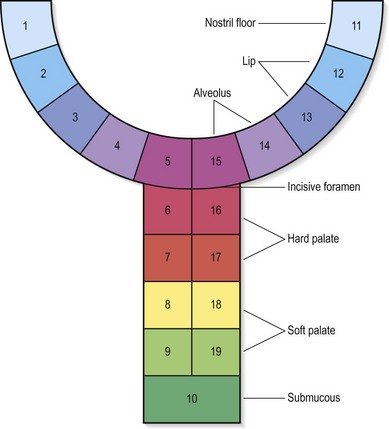
(From Noordhoff MS, Huang CS, Wu J. Multidisciplinary management of cleft lip and palate in Taiwan. In: Bardach J, Morris HL, eds. Multidisciplinary Management of Cleft Lip and Palate. Philadelphia: WB Saunders; 1990:23.29)
All clefts in the illustrations of patients in this chapter are classified according to the letter method and the modified Y numeric method. The numeric method is more accurate in recording partial clefts. Any combination of numbers can readily record the finer degrees of partial clefts. Examples of classification are shown in Figures 23.2–23.5.
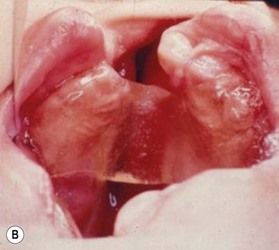
Diversity of the cleft pathology
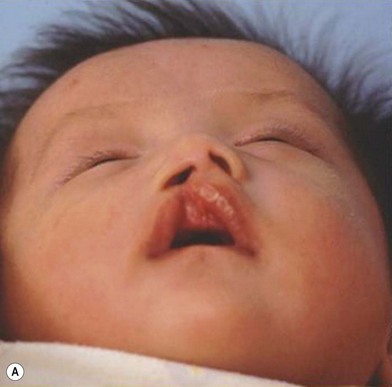
Deficiencies of soft tissue, cartilage, and bone in cleft patients are difficult to evaluate accurately. There is an obvious difference in the availability of soft tissue among the following examples: (1) Left incomplete cleft of the primary palate (microform cleft lip, LPI, 13–14; Fig. 23.2); (2) Right incomplete cleft of the primary palate (incomplete cleft lip, RPI, 2–4; Fig. 23.3); (3) Left complete cleft of the primary and secondary palate (unilateral cleft lip and palate; LPC and LSC; 11–19; Fig. 23.4) and 4. Median facial dysplasia patient31 (Fig. 23.5). The surgeon can make an overall impression of cleft width, alar cartilage distortion, soft tissue deficiencies including the thickness and amount of orbicularis muscle, and underlying bony framework. Although impressions are useful, they cannot be quantitatively recorded.
Linear lip measurements of anthropometric marks provide a means of evaluating lip deficiencies. The quality and deficiency of the alar cartilage are impossible to evaluate accurately without a “cadaver-like” dissection. Deficiencies of bone can be recorded with three-dimensional computed tomographic scans, an accurate method of evaluating bone deficiencies but not practical in all patients. The computed tomographic scans (Figs 23.2–23.5) show a wide spectrum of bone deficiency that is present in the maxilla and alveolus. There is evident piriform deficiency in the occult cleft of Figure 23.2. There is a progressive deficiency of bone in the piriform area and maxilla, as shown in Figures 23.3–23.5. These patients demonstrate a wide variety of bone, cartilage, and soft tissue deficiencies. This helps support the concept that all clefts are different, and the potential for normal growth probably varies considerably from patient to patient, in part because of these deficiencies.
Diagnosis/patient selection
Simple measurements with a caliper of important anthropometric points provide an inexpensive and accurate assessment of soft tissue deficiencies.32 Measurements, on the basis of the anthropometric marks, are made at the time of surgery and recorded.
Lip measurements and markings
Cupids bow and vermillion
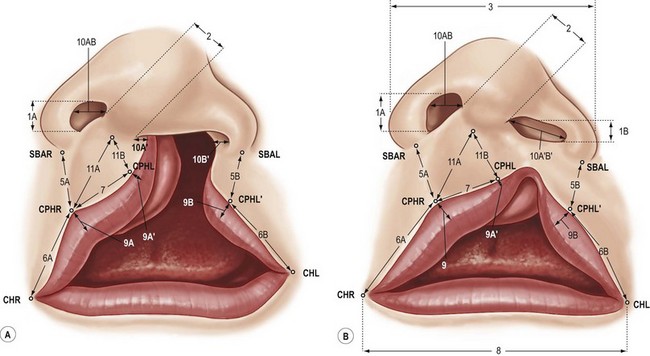
The points of the Cupid’s bow (CPHR, IS, CPHL) are marked on the epidermis-vermillion junction line, the white skin roll (WSR), as identified by Millard.33 The vermillion-mucosa junction line, the red line,34 is also marked. This clearly defines the intervening vermillion and also helps identify the deficient vermillion beneath the cleft-side Cupid’s bow. Other points marked are the base of the ala (SBAR, SBAL) and the commissure (CHR, CHL) (Fig. 23.6).
The base of the cleft-side philtral column
The base of the cleft-side philtral column (CPHL′) is a definite anatomic point but somehow difficult to identify. The red line always converges and meets the white skin roll medially. There is frequently a distinct point where the white skin roll changes directions and makes a slight curve about 3–4 mm before it meets the red line.35,36 The base of the cleft-side philtral column is where the white skin roll changes direction and where the vermillion first becomes widest, usually 3–4 mm lateral to the converging point of red line and white skin roll. This is an important anatomic point for the cleft-side philtral column and should seldom be moved unless there is a severe discrepancy in horizontal or vertical measurements between the cleft side and noncleft side lips.
Evaluation of tissue deficiency or excess
Pool36 noted areas of vital concern to the surgeon: the amount of tissue medial to the base of the ala and the vertical height of the lateral lip. In addition, the horizontal length of the lateral lip and the epidermal extension from the columella onto the premaxilla are important.
Peaking of Cupid’s bow
The discrepancy between the height from the central point of the base of columella to the two peaks of the Cupid’s bow (CPHR and CPHL) is critical for leveling of the Cupid’s bow. It was advocated that if the discrepancy is over 4 mm, it will be difficult to level the Cupid’s bow with rotation-advancement technique.33
Lateral lip length and height
The short horizontal length on cleft side (HL) can be lengthened by moving point CPHL′ medially, but this would shorten the vertical length (VL). Vertical length is more important aesthetically compared with the horizontal length. Therefore, vertical length is seldom sacrificed for horizontal length. The short vertical length can be increased by moving point CPHL′ laterally, but this would result in an even shorter horizontal length that is already short. Extending the upper rotation-advancement incision around the ala can also increase the short vertical length. However, this results in an unacceptable perialar scar and should be avoided. It is stressed that point CPHL′ is an anatomic point34–36 similar to other anatomic points. It is not moved until all incisions, muscle dissection, and reconstruction are completed. The reason for this is that an increased vertical length of up to 4 mm can be achieved by adequate muscle dissection and redraping of the skin over the muscle, thus eliminating the need of perialar incisions or moving the point CPHL′.35,37,38 In incomplete clefts, it is quite often to see a vertically long lateral lip. However, the measurements usually show the vertical height of the cleft side lip is similar to the noncleft side which means the cleft side lateral lip and the alar base are downward displaced. The vertically long lateral lip in incomplete clefts is just an illusion. Adequately mobilization of the cleft side alar base and lateral lip then advance the whole lateral complex superiorly and medially can always level the Cupid’s bow thus vertical shortening of the lateral lip is seldom needed.
Columella and nasal floor skin
If the columella is narrow, a Mohler’s rotation incision39 would result in a very narrow columella base and should be avoided.37 If there is deficient skin lateral to the base of the columella, use of C flap tissue to elongate the columella could result in a small nostril. In addition, it is advocated that increased vertical length of the advancement flap can be obtained by use of vestibular skin.40 The disadvantage of vestibular skin is that it often includes hair follicles, which are unattractive. When there is deficient skin lateral to the base of the columella, the use of vestibular skin for increasing the length of the advancement flap would result in a small nostril. Careful evaluation of skin lateral to the columella and medial to the alar base is important to prevent a small nostril.
Deficient vermillion beneath the Cupid’s bow
The vermillion beneath the cleft-side Cupid’s bow is always deficient compared with the counterpart vermillion width on the noncleft side (Fig. 23.6).35 Inadequate reconstruction of this deficient vermillion will result in free border deformities as seen in a straight-line vermillion closure.34 The vermillion medial to the base of the philtral column (point CPHL′) fits into the deficient vermillion beneath the Cupid’s bow.
Treatment/surgical technique
Overall cleft treatment plan in the Chang Gung Craniofacial Center
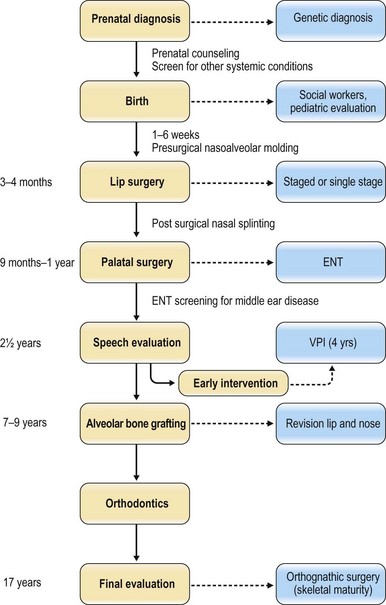
A genetic diagnosis and evaluation for other systemic conditions should be done at the time a prenatal diagnosis of the cleft is made. The newborn cleft baby should have a pediatric evaluation. Parents are counseled about feeding and given information for subsequent care and treatment. Presurgical nasoalveolar molding is started at 2 weeks or even earlier. It usually takes 3–4 months before the completion of the nasoalveolar molding (Fig. 23.7).37
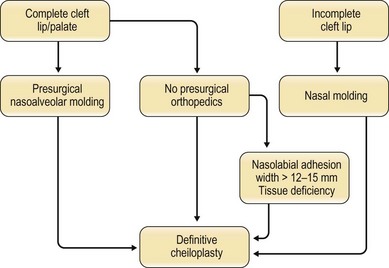
The surgical approach
There are several different treatment plans leading to the surgical correction of the deformity (Fig. 23.8).37 With effective presurgical nasoalveolar molding, a definitive cheiloplasty is done at the age of 3–5 months, when the alveolar gap is narrowed and nasal deformity is improved. Whenever presurgical orthopedics is not available or if the child is older than 3 months, a definitive cheiloplasty with nasal correction is done because presurgical orthopedics is usually not effective after 3 months. If there is a wide cleft (>12–15 mm) and an associated tissue deficiency, a nasolabial adhesion cheiloplasty is done at 3 months, followed by a definitive cheiloplasty at about 9 months.
Treatment after lip repair
A two-flap palatoplasty, with a Furlow technique for the soft palate, is done at 9–12 months. In most instances, a complete closure of all operative areas is attempted. Timing of alveolar bone grafting relates to the eruption of the central incisor and canine. It is determined by the orthodontist. This is usually at the age of 7–11 years. Speech evaluation starts at the age of 2.5 years. Early intervention for velopharyngeal insufficiency is done as soon as possible on the basis of speech evaluation and nasopharyngoscopy. With continued improvement in the primary nasal reconstruction, secondary correction of nasal deformities can usually be delayed until facial growth is complete. However, if there is a significant nasal or lip deformity, or psychological reasons that warrant correction, secondary correction is done before the start of school. Orthodontic treatment during primary dentition is not done except for functional problems that can be corrected in a short time. Orthodontic treatment during mixed dentition is done to correct an anterior crossbite or align deviated incisors before alveolar bone grafting. Continuous orthodontic treatment in the mixed dentition is avoided. For most patients, a fixed orthodontic appliance is used to improve dental occlusion during permanent dentition. Orthognathic surgery is considered for maxillary hypoplasia associated with malocclusion at the time of skeletal maturity (Fig. 23.7).37
Presurgical alveolar and nasoalveolar molding
Alveolar molding: external taping with or without dental plate
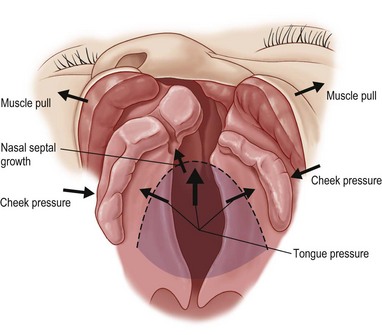
The external taping (nonsurgical lip adhesion) is the simplest technique for both presurgical molding of the maxillary halves and approximation of the alveolus. A strip of Micropore tape is placed across the cleft to approximate the upper lips. The objective of the tape is to simulate effects of an adhesion cheiloplasty and reposition the maxillary segments into proper alignment.37,41 The external taping transfers the tension caused by the approximation of the cleft lip into an inward molding force on the premaxillary alveolus of the greater segment, gradually approximating the separated alveolus (Fig. 23.9). A dental plate used in conjunction with the external taping keeps the tongue out of the cleft and prevents uncontrolled collapse of the dental arches. The central forces of the tongue pushing into the cleft and lateral muscle pull contribute to the cleft deformity (Fig. 23.10). The dental plate is gradually ground out on its inner surface for controlled movement of the maxillary segments into their proper position.
Nasoalveolar molding
Liou’s method
This method utilizes a molding bulb attached to a dental plate as an outrigger to mold the nose along with external taping of the lip. The device is held to the palate with dental adhesives. The force from taping and counterforce from the molding bulb provide the combined force necessary to bring the alveolus into proper position. The nasal molding and alveolar molding are done at the same time, taking approximately 3 months.37,42
Overstretching of the nasal cartilage on the cleft side should be avoided. Nasal projection and the dental plate are modified or adjusted every 1–2 weeks until the arch and nose are properly positioned (Fig. 23.11). A new molding device, with spring mechanism, is used at the Chang Gung Craniofacial Center in recent years. It can greatly lengthen the duration between each clinical visit from 1 week to 1 month, thus significantly reducing the burden of care for parents (Fig. 23.12).
Grayson’s method
Grayson43,44 performs the nasal molding after alveolar approximation to avoid overstretching the nasal cartilage. The appliance consists of an acrylic or resin plate which fits over the maxillary dental arch (alveolar ridges), an acrylic retention arm or button, and a nasal stent. The nasal stent consists of a wire extending from the plate intranasally forming a kidney bean shape. This bilobed potion of the nasal stent is covered with soft acrylic. Alternatively, the nasal stent can be formed entirely from acrylic. Micropore tape applied to the lips and connected with orthodontic elastics hold the dental plate to the palate. Gradually adding soft resin on the inner surface of the buccal flange and grinding out the palatal surface of the dental plate approximates the alveolar shelves. The nasal projection is added and adjusted underneath the deformed cartilage. This technique should be started within the first 2 weeks after birth; careful monitoring is required every 1–2 weeks for a period of 3–6 months to complete it (Fig. 23.13).
Discussion of presurgical orthopedics
The primary objective of presurgical orthopedics is to correct the skeletal deformities of the cleft maxilla before surgery.45–51 Keeping the tongue out of the cleft and replacing the pulling force from the separated lip muscle by tape traction across the lip accomplishes this purpose (Fig. 23.9). Regardless of no improvement to facial growth,52,53 presurgical orthopedics provides a better bony framework with a narrower cleft. Most surgeons, given a choice, would like a closely approximated cleft alveolus at the time of surgery.54,55 It is also noted that there is a statistically significant increased narrowing of the cleft when the infant sleeps on the side compared with sleeping on the back.56 Presurgical nasoalveolar molding can greatly improve the nasal shape before operation, thus facilitating nasal reconstruction.43,44,57–59
Surgical technique
Adhesion cheiloplasty: two-staged repair
The use of the adhesion cheiloplasty was first credited to Johanson.60 The adhesion cheiloplasty is used as a routine part of the primary repair at some centers,61–64 whereas it is used selectively at other centers.35,65,66 A number of techniques are used. They vary from a simple type of lip adhesion67,68 or a nasolabial adhesion,62 to a more complex nasolabial adhesion used at the Chang Gung Craniofacial Center.35,37 The incidence of dehiscence varies from 2–22%.62,67,69 The incidence of nasolabial adhesion cheiloplasty decreased from 37% in 1986 to 1% in 1999 in the Chang Gung Craniofacial Center.37 Factors contributing to a decreased incidence are more experienced cleft surgeons, improved presurgical orthopedics, and changing the sleep position from the supine to the prone or side position, thus decreasing cleft width.56
The advantages and disadvantages of a two-stage nasolabial adhesion cheiloplasty
The advantages of a two-stage cheiloplasty are frequently stated to be narrowing of the cleft, decreased tension across the maxilla, easier correction of nasal deformity and development of more muscle or elongation of a short lip before definitive cheiloplasty.70 If a preliminary nasolabial adhesion is warranted, it should produce better results with fewer secondary revisions and less disturbance of growth than a single-stage cheiloplasty.
In an evaluation of a two-stage procedure, Mulliken and Martinez-Perez62 reported that 75% required nasal revision and 21% a revision of the lip. There are too many variables to determine whether an initial two-stage procedure or one-stage cheiloplasty gives a better result. In both instances, there will be a need for secondary procedures. This question relates to the surgeon’s confidence in the ability to correct the problem, the timing of the procedure, and the desires of the patient or family.
Tension could possibly be decreased in a two-stage procedure, but even with an adhesion cheiloplasty, there is a muscular sling that causes increased tension, which molds the maxillary segments into position in a more gentle fashion.71 There is no evidence to support the theory that a staged repair is better than a one-stage repair because of less tension.72–77 Obtaining a better nostril with a two-stage procedure is also questioned.62
The biggest disadvantage of an adhesion cheiloplasty is the scarring. This makes dissection and mobilization of the tissues more difficult than in a one-stage procedure. It is suggested that after lip adhesion, there is an increase in the vertical lip length and muscle volume, thus making the subsequent cheiloplasty easier and delivering a better result. A 10% increase in vertical height after nasolabial adhesions is reported, and this is an insufficient reason for advocating a preliminary adhesion cheiloplasty.78
Nasolabial adhesion cheiloplasty: surgical technique
An adhesion cheiloplasty is done in less than 1% of all clefts after the use of nasoalveolar molding in the Chang Gung Craniofacial Center. Current indications for a nasolabial adhesion cheiloplasty are: (1) An alveolar cleft >12–15 mm wide with an associated discrepancy of >5 mm in the vertical height between SBAR-CPHR and SBAL-CPHL′; (2) a complete cleft of the primary palate in which there is a prominent protruding premaxilla resulting in a long sagittal discrepancy between the premaxilla alveolus and maxilla.37 Tissue deficiencies are more important than cleft width as a criterion in decision-making for a nasolabial adhesion cheiloplasty.
Markings
Standard markings and measurements for an adhesion cheiloplasty are similar to those of the complete unilateral clefts. However, vital landmarks CPHL and CPHL′ and the vermillion medial to the base of the cleft-side philtral column (point CPHL′) must not be violated (Fig. 23.14).
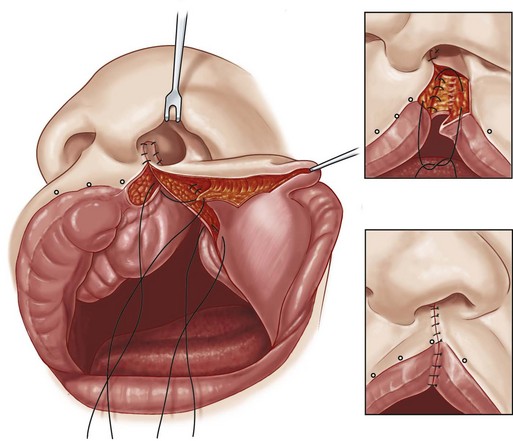
Elevation and insertion of C flap mucosa
An incision is made on the free edge of skin and mucosa on the noncleft side lip and extended posteriorly to the junction of columella skin and septal mucosa. All skin overlying the premaxilla is preserved. The mucosal C flap, based on the premaxilla, is incised and elevated. It is rotated and inserted behind the columella. This allows mobilization of the medial lip. There is no dissection of muscle (Fig. 23.14).
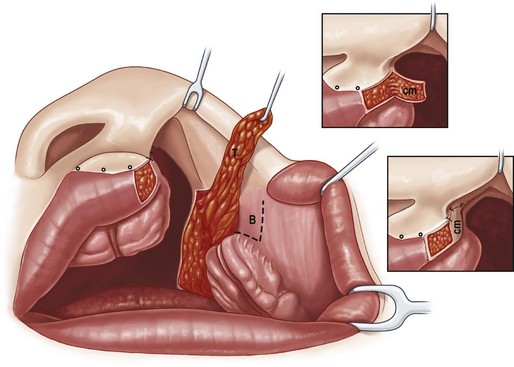
Lateral lip incisions
The buccal mucosal flap and inferior turbinate (T) flap are elevated based on vestibular skin. The free edge of the lateral lip is opened, preserving the vermillion medial to CPHL′ on the lateral lip. There is no muscle dissection. The fibrous attachments between the lower lateral cartilage (LLC) and piriform rim are released for mobilization of the alar base and LLC (Fig. 23.15).
Mucosal flaps
With traction on a suspension suture through the dome of the upper lateral cartilage (ULC), the LLC is advanced and with its lateral crura sutured to the ULC. The T flap is rotated and sutured to the piriform rim. The buccal mucosal flap is folded on itself and sutured to the edge of the T flap (Fig. 23.15).
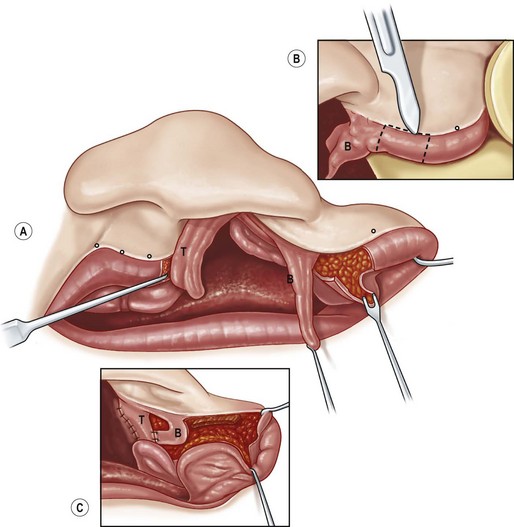
Nostril floor closure
The leading edge of the folded buccal flap is advanced and sutured to the periosteum of the premaxilla. The buccal lip mucosa is advanced and sutured to the bridging mucosal flap and to the periosteum and mucosa of the premaxilla (Fig. 23.16).
Definitive cheiloplasty after adhesion
The adhesion cheiloplasty changes a complete cleft into an incomplete cleft. The definitive cheiloplasty can be performed around 6 months later after scar maturation. The technique described below is the technique used since the late 1990s in the Chang Gung Craniofacial Center. The rotation-advancement is more of a straight-line type of incision from the cleft side of the Cupid’s bow to the base of the columella. The C flap is usually brought laterally, and the advancement flap is incised and advanced medially (Fig. 23.17)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree