24 Repair of bilateral cleft lip
Synopsis
 A child born with bilateral cleft lip should not have to suffer because of an ill-conceived and poorly executed primary repair. The operative principles for synchronous nasolabial repair are established:
A child born with bilateral cleft lip should not have to suffer because of an ill-conceived and poorly executed primary repair. The operative principles for synchronous nasolabial repair are established:
 The techniques based on these principles are within the repertoire of a well-trained surgeon whose practice is focused on children with cleft lip. Only the philtral columns and dimple seem just beyond the surgeon’s craft.
The techniques based on these principles are within the repertoire of a well-trained surgeon whose practice is focused on children with cleft lip. Only the philtral columns and dimple seem just beyond the surgeon’s craft.
 Preoperative dentofacial orthopedic manipulation of the premaxilla is necessary to permit synchronous closure of the primary palate. The surgeon must repair the bilateral cleft lip and correct the nasal deformity in three-dimensions based on knowledge of anticipated changes in the fourth-dimension. Modifications of the techniques used in repair of the most common complete form are needed for the less common bilateral variants, such as, binderoid, complete with intact secondary palate, symmetrical incomplete, and asymmetrical complete/incomplete.
Preoperative dentofacial orthopedic manipulation of the premaxilla is necessary to permit synchronous closure of the primary palate. The surgeon must repair the bilateral cleft lip and correct the nasal deformity in three-dimensions based on knowledge of anticipated changes in the fourth-dimension. Modifications of the techniques used in repair of the most common complete form are needed for the less common bilateral variants, such as, binderoid, complete with intact secondary palate, symmetrical incomplete, and asymmetrical complete/incomplete.
 Outcomes can be assessed using preoperative and serial photography and documentation of revision-rates. Direct anthropometry is the “gold-standard” for quantification of the changing nasolabial features; however, it requires training and experience. Intraoperative anthropometry is used to record baseline dimensions and repeated as the child grows. Two-dimensional photogrammetry is applicable for certain linear and angular measurements if properly scaled. Computerized three-dimensional photogrammetry is a new methodology for quantifying nasolabial appearance. It is both accurate and reliable, and someday could be employed in intra- and inter-institutional comparative studies.
Outcomes can be assessed using preoperative and serial photography and documentation of revision-rates. Direct anthropometry is the “gold-standard” for quantification of the changing nasolabial features; however, it requires training and experience. Intraoperative anthropometry is used to record baseline dimensions and repeated as the child grows. Two-dimensional photogrammetry is applicable for certain linear and angular measurements if properly scaled. Computerized three-dimensional photogrammetry is a new methodology for quantifying nasolabial appearance. It is both accurate and reliable, and someday could be employed in intra- and inter-institutional comparative studies.
Introduction
James Barrett Brown and his colleagues wrote that a bilateral cleft lip is twice as difficult to repair as a unilateral cleft and the results are only half as good.1 Now, over one-half century later, many surgeons still seem resigned that the appearance of their patients after bilateral cleft lip repair cannot match those with repaired unilateral cleft lip. Too many infants born with bilateral cleft lip undergo old-fashioned, often multistaged, procedures, and later have to endure sundry revisions throughout childhood and adolescence. Despite the surgeon’s efforts, the stigmata of the repaired bilateral cleft lip and nose remain painfully obvious – even at a distance.
To the contrary, I have written that the appearance of a child with repaired bilateral cleft lip should be comparable to, and in many instances surpass, that of a repaired unilateral complete cleft lip.2 This optimistic statement is based on two major advances in management of bilateral cleft lip over the past quarter century. First, is the recognition of the need for preoperative manipulation of the protuberant premaxilla. Second, is the acceptance of the principles and techniques of bilateral labial repair and especially the importance of synchronous correction of the nasal deformity.
Principles
Surgical principles, once established, usually endure, whereas surgical techniques continue to evolve. The following principles for repair of bilateral cleft lip were induced based on study of the literature and observations of residual deformities:3
1. Maintain nasolabial symmetry. Even the slightest differences between the two sides of the lip and nose will become more obvious with growth. Symmetry is the one advantage a bilateral cleft lip has over its unilateral counterpart.
2. Secure muscular continuity. Construction of a complete oral ring permits normal labial function, eliminates the lateral bulges, and minimizes later distortion of the philtrum and interalar widening.
3. Design the philtral flap of proper size and shape. The philtrum rapidly elongates and widens, particularly at the columellar-labial junction.
4. Construct the median tubercle using lateral vermilion-mucosal elements. There is no white roll in the prolabium. Retained vermilion lacks normal coloration and fails to grow to full height.
5. Position the slumped/splayed lower lateral cartilages and sculpt excess soft tissue in nasal tip and columella. These maneuvers are necessary to establish normal nasal projection and columellar length/width.
Principles 1–4 needed definition, interpretation, and confirmation. Principle 5, primary correction of the nasal deformity, was a fundamental change in surgical strategy. The so-called “absent columella” is an illusion; nearby labial tissue need not be recruited to build it. “The columella is in the nose” became this surgeon’s shibboleth. The columella can be exposed by anatomic positioning and fixation of the lower lateral cartilages and sculpting expanded skin in the soft triangles and upper columella.4
Third and fourth dimensions
Farkas and colleagues used direct anthropometry to document the normal patterns of nasolabial growth in Caucasians from age 1–18 years.5 Fast-growing nasolabial features attain more than 75% of adult dimensions by age 5 years. For example, nasal height and width develop early, reaching a mean of 77% and 87% of adult size, respectively, by age 5 years. All labial landmarks grow rapidly, reaching approximately 90% of adult proportions by age 5 years. In contrast, tip protrusion and columellar length are slow-growing features; they attain a mean of only two-thirds of adult size by 5 years of age. These differences in nasolabial growth explain the well-recognized nasal stigmata and labial misproportions of a repaired bilateral cleft lip. The fast-growing features become overly long or too wide, i.e., interalar distance and philtral length and width. For example, in an early study of a small number of patients, it was determined that from time of initial closure to age 5 years, the philtrum had widened by a factor of 2.5 at the top and expanded two-fold between the peaks of Cupid’s bow.3 In contrast, nasal tip protrusion and columellar length remain abnormally short following conventional repair.
Applying a posteriori reasoning, the nasolabial features programmed for rapid growth in early childhood must be crafted on a small scale, whereas slow-growing features should be made slightly larger than the normal dimensions for an infant. Construction of the median tubercle is the exception to these guidelines. This normally fast-growing feature reaches 87% of adult height by age 5 years, but after bilateral cleft lip repair, the tubercle lags behind. Therefore, it must be fashioned to be as full as possible, anticipating insufficient growth.2,6,7 There is also the unpredictable fourth-dimensional factor of central incisal show. Despite the surgeon’s effort to craft a full median tubercle, augmentation may be necessary after eruption of the permanent central incisors and after the maxilla is in normal sagittal position.
Historical review
The premaxilla
The projecting premaxilla has long been the stumbling block to closure of the bilateral complete cleft lip. From the Renaissance until the early 20th century, some aggressive surgeons would resect the protruding intermaxillary bone, either preserving the prolabium, shifting it upward to elongate the columella, or dispensing with it altogether. In an effort to retrude the premaxilla, Gustav Simon introduced the technique of paring the edges of the prolabium and construction of bilateral labial adhesions. His method is probably the source of the dubious eponym “Simonart’s bands”.8 Premaxillary “set-back” by vomerine resection was described in the 19th century and continued to be practiced well into the 20th century by Veau,9 Brown, McDowell and Byars,1 Browne,10 Cronin,11 and Monroe.12 The history of this procedure is detailed by Millard in Vol. II of Cleft Craft.13
Labial closure
Techniques for labial repair of the bilateral deformity were adapted from those used for the more common unilateral cleft lip. Textbooks and articles well into the mid-20th century recommended staged bilateral repair: one side of the cleft (usually the widest) and then the other side. Conspicuous asymmetry was the predictable result. Surgeons believed that the diminutive prolabial element lacked the potential for full growth, and, therefore, had to be lengthened. Thus, various techniques employing rectangular-shaped lateral labial flaps inserted beneath the cutaneous prolabium were described by König, Hagedorn, Mirault, and later by Barsky.13 Insertion of cutaneous lip below the prolabial flap resulted in an unnaturally long lip; this iatrogenic deformity was not well-appreciated until the mid-20th century. Alternatively, triangular flaps from the lateral labial elements were interdigitated into the prolabial segment to increase philtral height.1,14–18 LeMesurier transposed bilateral quadrilateral flaps below the prolabium; however, later he utilized the entire prolabium without interdigitating flaps.19 All these methods resulted in curious geometric labial scars (which were often asymmetrical, especially if one side was closed first), a vertically long lip, and a tight lip from side-to-side. In time, surgeons began to recognize that the philtrum has a remarkable capacity for vertical growth once it is attached to the lateral labial elements.20–22 Eventually, minor variations on a straight-line type (Veau III) labial closure became the standard design.11,23 Although this method diminished elongation of the central lip, the result was typically an abnormally wide, shield- or keystone-shaped philtrum. This was attributed to the failure to attain muscular continuity and to properly design the philtral flap in expectation of growth, especially in the transverse dimension.3
There has been a longstanding dispute about how to form the median tubercle. The alternatives are either to preserve the prolabial vermilion (resulting in a scar on each side of the median tubercle), retain a tiny strip of central vermilion or excise it completely and build the tubercle from lateral vermilion-mucosal flaps. If the prolabial vermilion-mucosa is preserved, the free margins of the lateral labial elements tend to hang like swags, flanking a deficient median tubercle that is covered by a thin strip of vermilion and exposed chapped mucosa (“whistling lip deformity”). In profile, the upper lip is flat or convex, lacking a pout. This abnormal contour is further accentuated by an everted lower lip and weak chin. The “cleft lip lower lip deformity” is caused by the child’s struggle to obtain bilabial closure over a protrusive, retroclined and vertically-elongated premaxilla.24
Muscular closure
Little attention was given to closure of the orbicularis oris muscle until the middle half of the 20th century; the early advocates were Schultz,20 Browne10 and Glover and Newcomb.25 Manchester held to the traditional belief that joining muscle from the lateral elements across the midline would inhibit premaxillary growth.26 He sutured the orbicularis oris to the central subcutaneous tissue to minimize tension on the premaxilla. Without muscular continuity, whenever the child puckers, a bulge appears on each side of the lip. Primary muscular closure is necessary to minimize fourth-dimensional distortions, i.e., lateral drift of the alar bases and widening of the philtrum. Perhaps equally important, the child is unhappy being unable to whistle.
With increasing attention to muscular closure in the unilateral deformity, reports began to underscore the importance of orbicularis oris repair in bilateral clefts.13,27–31
Nasal inattention
Bilateral labial closure produces and accentuates the “bilateral cleft lip nasal deformity.” The nasal tip is overly broad. The medial crura are pulled into an inferoposterior position; this further dislocates the splayed alar domes and causes the genua to buckle (“recurvatum deformity”) and the alae nasi to flare (“cat’s knees” deformity). The caudal margin of the drooping lower lateral cartilages protrudes into the lateral vestibules producing an oblique ridge or web. Without amends for the vertically long lateral labial elements and normal muscular attachments to the alar bases, an unnatural elevation of the alae nasi occurs, which becomes more pronounced whenever the child smiles.32 In short, conventional bilateral labial repair worsens the nasal deformity. Furthermore, the deformed and displaced lower lateral cartilages are more difficult to correct secondarily.3
Secondary nasal correction
Conventional teaching was that the columella was lacking in a bilateral cleft lip. Numerous secondary procedures were devised to elongate the “short columella.”33 There were two major technical strategies, and curiously, both were published in 1958. The first in print, the Cronin method, involves rotating bipedicled strap flaps from the nostril sills.34 This procedure results in modest columellar length, and there is a tendency for loss of the initial gain in height. The second method is the forked flap procedure, devised and popularized by Millard.13,35 There are two variations on the forked flap theme. For infants with a wide prolabium, the tines of the forked flap can either be transposed directly into the columella or banked below the sills and “cashed in” later in early childhood. Alternatively, if the prolabium is relatively narrow, Millard preferred three-stage columellar lengthening: (1) bilateral labial adhesions to expand the prolabium; (2) elevation, rotation, and banking the tines while narrowing the philtrum (around age 18 months); (3) retrieval of the prolabial prongs and elevation, along with the medial crura, to lengthen the columella (at age 2 years).
Millard’s forked flap, like all secondary procedures, causes tertiary distortions peculiar to the particular technique.4 Most secondary methods introduce a nexus of scars across the columellar-labial junction. This scarring causes a transverse nasolabial crease that deepens with smiling and is extremely difficult to surgically correct. There is a circumferential philtral scar that has a tendency to cause a bulge rather than a dimple. Secondary recruitment of tines from each side of the philtrum in an older child usually results in thickened and wide philtral scars. Even in skilled of hands, the forked flap procedure results in an unusual appearing nose. The characteristics include: (1) rectangular columella with a broad base and absent waist; (2) sharp columellar-labial angle; (3) abnormally elongated/enlarged nostrils; (4) columellar over-elongation with a disproportionate ratio of nostril length-to-nasal tip; (5) downward drift of the columellar base.4,36,37 Furthermore, the medial crura becomes unnaturally positioned in the nasal tip, resulting in a slight break at the columellar-lobular connection. Thus, some surgeons began to wonder whether labial skin really belongs in the columella. Others questioned whether the columella was really deficient at all. Maybe it would be possible to correct the nasal deformity along with the labial closure. About this same time, nasal correction during repair of unilateral cleft lip was becoming more credible.
Primary repair of the bilateral cleft lip nasal deformity
Nasal dissection of stillborn infants with bilateral labial clefting revealed that the alar domes and middle crura are splayed and subluxed from their normal moorings to the upper lateral cartilages.32 The columella only appears short because of the malpositioned lower lateral cartilages. Furthermore, the investing domal skin is expanded; there is no reason to bring in more tissue. Broadbent and Woolf described a case of primary medial advancement of the alar domes combined with excision of skin from the broad nasal tip.38 But it was McComb who led the advance toward primary columellar elongation. Initially, he tried first elevating a forked flap, followed by second-stage labial closure.39 He published a follow-up assessment 11 years later, including measurements of columellar growth.40 However, by this time, he had become disenchanted with this strategy and presented a new two-stage technique for columellar construction using the tissue in the splayed nasal tip for repair – without a forked flap.37 In the first stage, he used an external incision (“flying bird”) to open the nasal tip and to appose and suspend the splayed genua. His tip incision, which extended almost to the columellar base, was closed V-to-Y fashion, thus shifting the alar margin into the tip and lengthening the upper columella. Long bilateral labial adhesions were part of his first operation; 1 month later, the lip was reentered for definitive repair. The columellae looked near normal in McComb’s longitudinal assessment at 4 years41 and equally good at 18–19 years, although the slight depression caused by the nasal tip scar is noticeable.42
The author was also focussed on early positioning of the lower lateral cartilages. Influenced by Millard’s teachings, he banked the tines of the forked-flap below the sills during bilateral labial repair. The second stage was a critical departure from Millard: the banked tines were transposed intranasally to allow the genua and medial crura to ascend. A vertical nasal tip incision was used to appose the domes, and bilateral rim incisions were used to suspend and secure the lateral crura. Anthropometric measurements in these children showed that nasal length, tip protrusion and columellar length were within normal limits.4 However, the interalar dimension was overly wide, the mid-columella was broad, and the upper lip was too long. The alar domes often buckled slightly, and there were two instances of nostril stenosis related to the intranasal transposition of the tines. By 1987, it had become obvious that prolabial tines were unnecessary, and soon thereafter, the vertical incision in the nasal tip was also abandoned. Primary columellar lengthening and normal nasal tip projection were achieved solely by apposition of the genua, elevation and fixation of the lower lateral cartilages to the ipsilateral upper lateral cartilages, and sculpting tissue from the soft triangles and upper portion of the columella.4,32
Other surgeons were also on the trail to primary repair of the primary palate. Trott and Mohan were working in Malaysia where socioeconomic factors made multistaged bilateral cleft lip repair impractical. They devised a single-stage nasolabial repair using an open rhinoplastic exposure of the dislocated lower lateral cartilages.43 The prolabial-columellar flap was based on the paired columellar arteries. The flap was dissected on the ventral surface of the medial-middle crura. Cutting and associates described another variation on the open-tip approach following presurgical stretching to elongate the columella and nasal lining.44 The prolabial-columellar flap is incised along the membranous septum, leaving the medial-middle crura in the flap; the genua and medial crura are apposed by transfixion mattress sutures.
McComb offered a delightful anatomic explanation for the diminutive columella: “… it has been unzipped and its component parts lie within the broad nasal tip”.37 The old, non-anatomic techniques that involved secondary recruitment of prolabial skin into the columella were wrong. Instead, the lower lateral cartilages should be placed and fixed in anatomic position followed by trimming and redraping the soft tissues of the nasal tip. No longer would columellae be overly elongated with (often hair-bearing) labial skin, nor would the nasolabial junction be transgressed by scar that completed encirclement of the philtrum.
Presentation
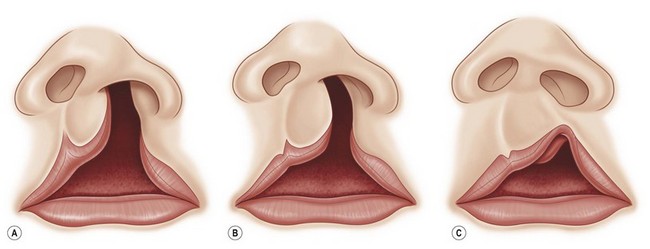
Bilateral cleft lip presents in three major anatomic forms: bilateral symmetrical complete (50%); bilateral symmetrical incomplete (25%), and bilateral asymmetrical (complete/incomplete) (25%).45 The extent of the palatal cleft usually corresponds to the severity of the labial clefts. Bilateral complete cleft of the primary palate (lip and alveolus) is almost always associated with a bilateral complete cleft of the secondary palate. Bilateral symmetrical incomplete cleft lip is usually seen with minor or absent notching of the alveolar ridge with an intact secondary palate. There is more variation in palatal clefting in the asymmetrical bilateral forms: the palate can be either bilateral complete or unilateral complete on the major side.
Terminology for the contralateral bilateral asymmetric cleft lip requires further refinement. In general, the term “incomplete” cleft lip usually denotes that there is cutaneous continuity between the medial (nasomedial process) and the lateral (maxillary process). Incomplete cleft lip presents in a spectrum. At the severe end, there is a thin cutaneous band that some would argue constitutes a “complete” cleft lip. At the other end of the spectrum are the lesser-forms of incomplete cleft lip. Yuzuriha and Mulliken classified and defined these lesser-forms as minor-form, microform, and mini-microform as determined by the degree of disruption at the vermilion-cutaneous junction.46
This detailed subcategorization of the contralateral side in an asymmetrical bilateral cleft lip is important because the extent of vermilion-cutaneous disjunction determines the operative strategy. Synchronous bilateral nasolabial repair is indicated for a contralateral incomplete cleft lip, including a minor-form. Correction of a contralateral microform or mini-microform is usually deferred until closure on the greater side. The type of contralateral (lesser-form) cleft lip not only guides the primary repair, it also foretells what revisions are likely to be necessary (Fig. 24.1).45
Preoperative dentofacial orthopedics
There are two dentofacial orthopedic strategies: passive and active. A passive molding plate is retained by undercuts and maintains the transverse width of the maxillary segments. An external force is needed to retract the premaxilla, such as adhesive tape from cheek-to-cheek or an elastic band attached to a headcap. Bilateral labial adhesions have been tried since the mid-19th century; however, they often dehisce because of tension and the absence of prolabial muscle. Cutting and Grayson have popularized a more sophisticated version of a passive plate and taping called “nasoalveolar molding” (NAM).44,47,48 Their plate produces differential pressure on the maxillary segments by selective reduction on the inner surfaces and addition of soft acrylic on the outer surfaces. After the alveolar gap is reduced to 5 mm, nasal molding begins. The nostrils are pushed upward by a bilobed acrylic nubbin on stainless steel prongs that are attached to the palatal plate. A soft denture material is added across the nasolabial junction and a vertical tape is placed from prolabium-to-appliance to give a downward counterforce to the upward force applied to the nasal tips that stretch the columella. The premaxilla is gradually retracted by serial application of tape across the outrigger to the cheeks or to the labia. These tapes are changed daily by the parents. The apparatus must be adjusted weekly to modify the alveolar molding plate so as to narrow the maxillary segments. Although usually effective, NAM is labor-intensive and slow. There is no expansion of the maxillary elements with NAM; it is difficult to retract the premaxilla into alignment with the lesser segments. Unless there is adequate space in the arch, the premaxilla will abut the labial surface of the segments.
Complications with “NAM” include inflammation of the oral and nasal mucosa, blistering of the cheeks, trouble in feeding the infant, and difficulty in centralizing a badly torqued premaxilla. The skin of the columellar-labial junction can ulcerate if the horizontal prolabial band is too tight. There is also a potential risk that the molding plate could become dislodged and obstruct the airway; infants are obligatory nasal breathers until about age 3 months. A 5 mm diameter hole is placed in the center of the molding plate to minimize the possibility of this complication.49
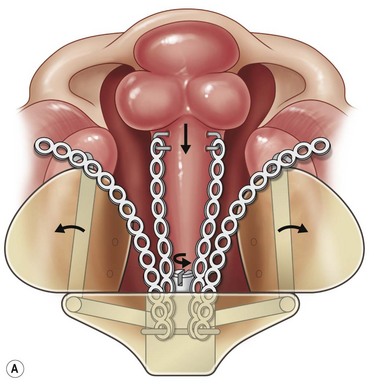
The active-type dentofacial orthopedic device in current use is based on the protypic design by Georgiade and associates,50 later refined and popularized by Millard and Latham.51 The Latham appliance is constructed from a plaster cast of the upper jaw taken in the office. In the past, the appliance was fabricated in London, Ontario, Canada. A local, skilled prosthetist can also fabricate the custom-device. The appliance is pinned to the maxillary shelves with the infant under general anesthesia. An elastic chain on each side is connected to a transvomer wire that is looped under a roller in the posterior-superior section of the appliance and attached to cleats at the anterior edges of the maxillary plate. The parents turn the ratcheted screw daily to expand the anterior palatal segments. Visits are necessary at 1, 3, and 5 weeks to assure appropriate fit and to adjust the bilateral elastic chains that retrocline the premaxilla. The process normally takes 6–8 weeks. The Latham appliance is effective in correcting premaxillary position in the sagittal plane; however the movement is more retroclination than retroposition. The appliance can also rectify premaxillary rotation, through differential traction, although there is little effect on vertical position (Fig. 24.2).
The merits of passive versus active dentofacial orthopedics continue to be debated by proponents of each approach. Critics of active premaxillary orthopedics argue it causes midfacial retrusion.52,53 Others have failed to document such an effect beyond that expected inhibition of vertical and forward maxillary growth in children with repaired bilateral cleft lip/palate and followed through the age of the mixed dentition.54 There is also recent controversy about a possible deleterious effect of alveolar gingivoperiosteoplasty.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree