Relapsing Polychondritis: Introduction
|
Epidemiology
The incidence of RP has been estimated to be 3.5/million in Rochester, Minnesota.1 The peak age for disease onset is the fifth decade; however, development of the disease may occur in young children and in the elderly.2 The male to female ratio has been estimated from 1.1 to 1.3.3 Although most cases have been reported in Caucasians, there is no evidence supporting the role of ethnic or geographical factors.
Etiology and Pathogenesis
Several lines of evidence have been accumulated that suggest the role of autoimmunity in RP. More than 30% of patients have an associated disease, mainly of autoimmune origin.
The role of the humoral immune response was based on the presence of antibodies to collagen type II in the acute phase of RP. Antibody titers seemed to correlate with the severity of symptoms. Other antibodies were secondarily detected in patients with RP: antibodies to collagen type IX and type XI, minor collagens which represent 5–10% of cartilage collagens, antibodies to matrilin-1, an extracellular matrix protein, predominantly expressed in upper respiratory tract cartilage, and antibodies to cartilage oligomeric matrix protein, other cartilage proteins expressed in auricular, tracheal and nasal cartilage. Several animal models have been published in which immunization with these various cartilage proteins induced a variety of chondritis manifestations that mimic those seen in patients.4 A role for immune complexes and subsequent activation of the complement system is suggested by examination of tissue lesions that usually show the presence of granular deposits of immunglobulins and the C3 component of complement associated with CD4+ lymphocytes and plasma cells. The influence of T cells in RP pathogenesis, although less investigated, has also been demonstrated in patients and in animal models with specificity against the same cartilage proteins. T-cell clones isolated from an RP patient were found to be specific for a peptide corresponding to residues 261–273 of the type II collagen and were restricted to either the DRBI*0101 or the DRBI*0401 allele.5 A significant near two fold increase in DR4 antigen frequency was found in RP patients as compared to that in healthy controls, but the genotyping of DR-4 positive patients and controls did not show a predominance of any DR4 subtype. Genetic susceptibility was also confirmed by animal models.6
Clinical Findings
Disease onset is usually sudden with characteristic chondritis, and/or less frequently arthritis or ocular inflammation. Nonspecific initial symptoms such as fever or weight loss are rare.
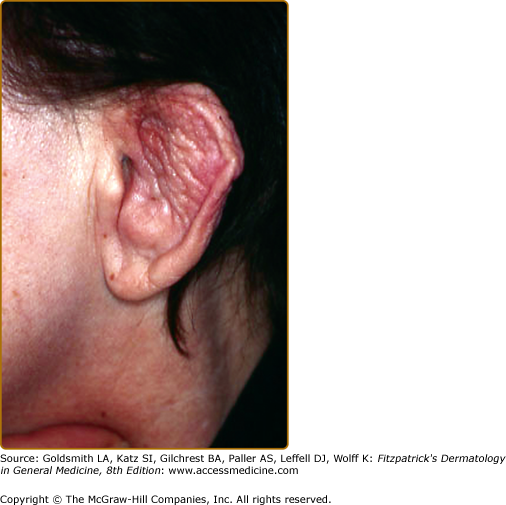
Attacks of chondritis usually occur in a relapsing and remitting pattern. Inflammatory episodes generally last a few days or weeks and may subside spontaneously or after treatment is initiated; recurrences after weeks or months occur and result subsequently in cartilage destruction. Auricular chondritis is the most frequent (85%), causing pain, redness, and swelling of the cartilaginous portion of the pinna, sparing the noncartilaginous lobe (Fig. 159-1). Biopsy of the auricular cartilage is not usually necessary to make a diagnosis. The histology shows perichondrial inflammation and the loss of the normal cartilaginous basophilia. After several attacks, the pinna may become soft and floppy with a cauliflower appearance (Fig. 159-2); sometimes it is stiff due to calcifications. Nasal chondritis (65%) is less inflammatory, presenting with nasal pain, stuffiness, rhinorrhea, and sometimes epistaxis. The characteristic saddle-nose deformity (Fig. 159-3) may appear secondarily or without previous inflammatory episodes. Respiratory tract chondritis, though uncommon at presentation, occurs in up to 50% of patients, and may be lethal. This results in complaints of hoarseness, nonproductive persistent cough, dyspnea, wheezing. Complications include upper airway collapse, obstructive respiratory insufficiency and secondary infections. Costochondritis (35%) induces parietal pains, which may also compromise respiration.
Joint pain is a common presenting feature (30%). Large and small joints of the peripheral or axial skeleton may all be affected (>70%). Arthritis is intermittent, migratory, asymmetric, seronegative, and usually nonerosive.