10Reconstruction of the Eyelids and Eyebrows
Abstract
Periocular cutaneous malignancies occur in up to 10% of all skin cancers, while approximately 14% of Mohs defects affect the lower forehead and the brow area. Hence, Mohs surgeons need to be familiar with this highly specialized area of the face. This chapter discusses a variety of techniques utilized for the reconstruction of eyelids, eyebrows, and the periorbital region after Mohs excision. After anatomical considerations of the eyelids and eyebrows, different reconstructive options are discussed and summarized in the algorithm for closure depending on the defect size, location, and thickness. A strict understanding of anatomic relationships and thorough knowledge of the principles of decision making when performing surgery in this area will enable the Mohs surgeon to achieve optimal cosmetic and functional results. Despite challenges that may require the assistance of oculoplastic surgeons, the majority of periocular repairs will have excellent results with proper globe protection and restoration of eyelid integrity.
Keywords: Eyelid anatomy, anterior lamella, posterior lamella, canaliculus, lacrimal system, medial canthus, lateral canthus, canthal tendon, primary closure, fullthickness skin graft, composite graft, wedge-excision, Tenzel semicircular flap, cross-eyelid flap, Hughes tarsoconjunctival flap, brow anatomy, brow reconstruction
Capsule Summary and Pearls
•Normal upper and lower eyelid structure is critical for globe protection and visual function.
•Restoration of eyelid integrity is critical for optimal functional and cosmetic reconstruction.
•The defects of the anterior and posterior lamella must be individually evaluated in order to choose the appropriate repair technique.
•If defects of medial canthi involve the lacrimal system, they may be assessed and repaired in consultation with an oculoplastic specialist.
•Brow reconstruction should consider aesthetic position of the brows, retention of brow symmetry, and the direction of the growth of the hair follicles.
10.1 Introduction
The eyes, eyebrows, and periocular area are the central aesthetic unit of the face. The functional and aesthetic importance of this region cannot be overestimated.
“The beauty of a woman must be seen from in her eyes, because that is the doorway to her heart, the place where the love resides.”
—Audrey Hepburn, British Actress (1929–1993)
Reconstruction1,2 of the eyelids is one of the most challenging areas in reconstructive surgery. No other region has such a delicate interaction of anatomy, function, and aesthetics. The primary goal in eyelid reconstruction is to restore a functional eyelid to protect the eye and permit normal vision. Proper eyelid function is required to maintain a normal tear film to avoid corneal irritation, desiccation, or perforation. The repaired eyelids should have normal appearance due to its critical importance in social relationships (secondary goal). Surgical objectives in the reconstructive process are1,2,3,4:
a)Align conjunctiva (nonkeratinized mucosal epithelium against the eye).
b)Provide support with firm connective tissue frame to appose the globe.
c)Enable adequate protractor muscle function and supple thin skin to facilitate and permit normal eyelid movements.
d)Obtain stable eyelid margin to prevent inappropriate turning of eyelids (ectropion, entropion, trichiasis) and irritation of the cornea and the globe.
The goal of this chapter is to present several reliably effective techniques that will address the majority of common defects to be encountered in the daily practice of Mohs surgery. Mohs micrographic surgery is ideal for skin cancer removal in the eyelid area as a cost effective, tissue-sparing procedure with the highest rate of cure.2,3 Recent reports by Clark et al5 showed that the safety profile of reconstruction after Mohs surgery performed under local anesthesia is comparable to ones performed by oculoplastic surgeons under general anesthesia.
10.2 Surgical Anatomy of the Eyelids and Eyebrows
The surgical anatomy of the eyelids and periocular area is one of the most complex parts of the head and neck.6–8 Before one embarks on performing a variety of simple or more complicated reconstructive procedures in periocular area, thorough knowledge of surgical anatomy is mandatory. The purpose of this text is not just to reacquaint the leader with well-documented gross morphology of the eyelids and brows, but also to review newer concepts of eyelid anatomy relevant for clinical practice.
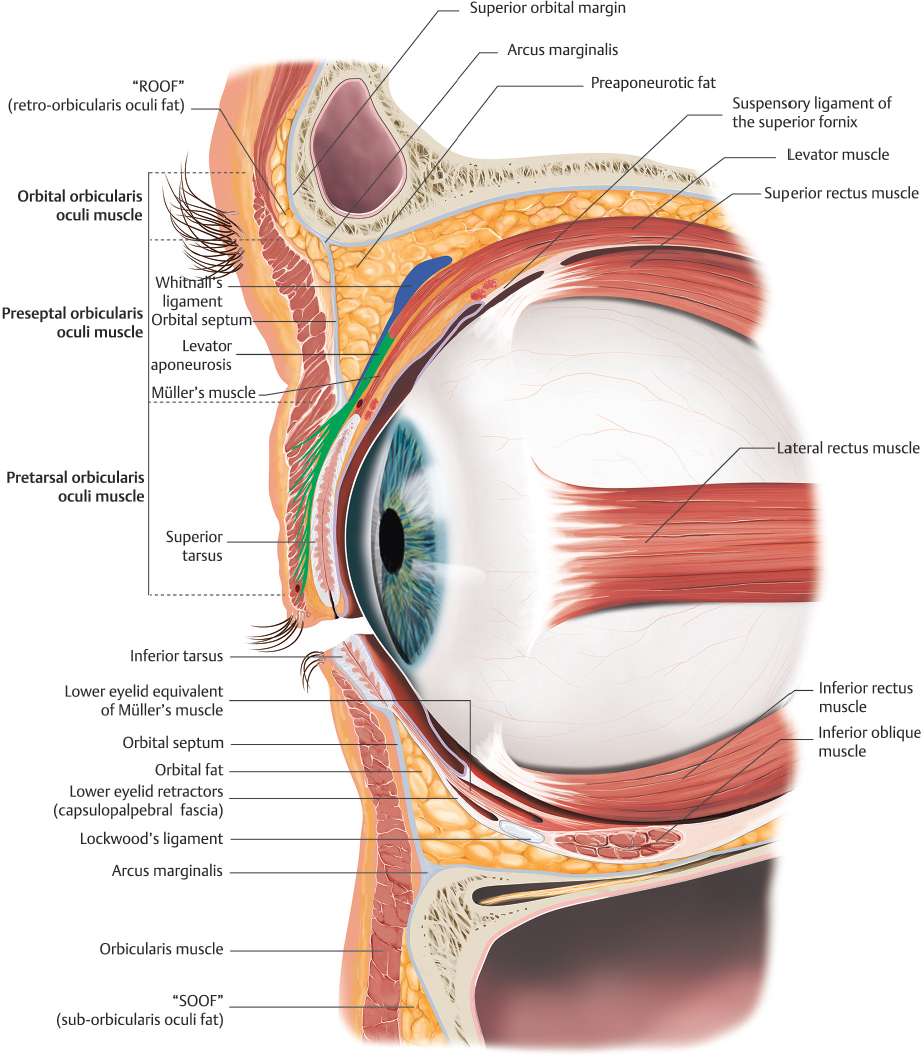
10.2.1 Superficial Topography of the Lids and Eyebrows (Fig. 10.1)
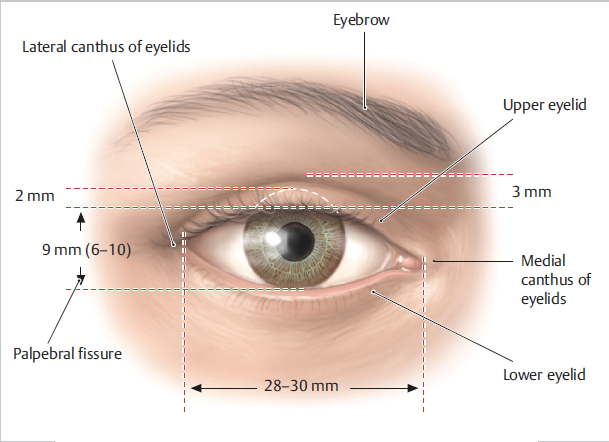
Fig. 10.1 Topography of the right eyelid. The highest point of the brow is at, or lateral to, the lateral limbus. The inferior edge of the brow is typically 10 mm superior to the supraorbital rim. Average palpebral height (10–12 mm), width (28–30 mm), and upper lid fold height (8–11 mm) vary with gender and racial differences. Note that the lateral canthus is 2 to 4 mm higher than the medial canthus. Intrapalpebral distance measures 10–12 mm. (Reproduced from Baker E, Lopez E, Schünke M, et al. Anatomy for Dental Medicine. Illustrations by M. Voll and K. Wesker. 3rd ed. New York: Thieme; 2020.)
The eyelids are complex lamellar structures responsible for globe protection and integrity of the ocular surface. The architecture of the eyelids must be respected to provide satisfactory repairs, both functionally and aesthetically.9–12 The eyelids are for practical purposes divided into anterior (skin and muscle) and posterior (tarsus and conjunctiva) lamella (Fig. 10.2). The orbital septum (OS) is considered a “middle lamella” by some authors due to its surgical and anatomic importance as a boundary between the preseptal soft tissues and postseptal content of the orbit. Of note, septum should not be repaired directly (aka “self-healing” layer), since it leads to tethering and lid retraction. For reconstruction purposes it is essential that at least one lamella have an intact blood supply.8
The eyebrows are approximately 4.5 to 5 cm long and slightly differ in female and male patients8,13,14 (Table 10.1). The female eyebrows are typically arched, with the highest point projecting at, or slightly lateral to the limbus, approximately 1 cm from the orbital rim, 1.5 cm and 2.5 cm from upper lid crease and pupil, respectively. The male eyebrow is less peaked and is positioned more closely to the orbital rim. The position of the brows is the result of opposing forces of brow elevator (frontalis muscle) and brow depressors (orbicularis oculi, procerus, and corrugators muscles). The soft tissue of the eyebrows consists of four layers8,13: (a) skin and subcutaneous tissue; (b) muscle; (c) retroorbicularis oculi fat (ROOF); and (d) periosteum. The lateral brow is firmly attached to temporalis fascia, which is also more prominent in males.13
Table 10.1 Anatomic and topographic differences of male vs. female upper face
Male | Female | |
Forehead | > Width and height (avg. 6 cm) | < Width and height (avg. 5 cm) |
Glabella | > Width and projection | < Width and projection |
Orbit | Larger | Smaller and more oval |
Orbit/skull ratio | Smaller | Larger |
Brow | Thicker, positioned at the level of the rim, flat with none to minimal arching, no prominent peak or lateral tapering | Medially club shaped, positioned above the rim, ascend and arch laterally to its peak, tapers laterally |
Upper eyelid | 8–9 mm crease height, fuller with minimal pretarsal show | 9–12 mm crease height, moderate pretarsal show |
Lateral canthus | Neutral to slightly positive tilt | Neutral to positive tilt |
The eyebrow hair is thinner in Asians, and thicker in Caucasians and comprises 200 to 400 follicular units (FU), each containing single hair shaft or rarely two, in contrast to the scalp hair, where four shafts can be found per FU.8,14,15 In addition, the eyebrow hair follicle direction needs to be well understood and is of utmost importance when designing brow incisions, orienting flap repairs, or using hair transplant techniques or composite grafts to restore lost supercilia. Centrally (brow body) and laterally (brow tail) the hair follicles are directed inferiorly, while medially (brow head) hairs and ones on the lower brows are directed superiorly (see following text). Eyebrows’ hair shafts lie quite flat on skin surface since they exit at very acute angle of 30 degrees. Eyebrow hair typically regrows within 6 months following plucking; however, repeated damage to eyebrow FU can result in traction alopecia and reduce growth over time. The three types of hair in the eyebrow are (a) fine, vellus hair; (b) the slightly larger and lightly pigmented hair; and (c) the large terminal hair, also known as the supercilia. The fine vellus hairs form an effective moisture barrier to keep sweat from running downward into the eye. The fluid flow is redirected medially and laterally, away from the eye.8,15
The eyelid skin is among the thinnest in the body and lacks underlying fat, which facilitates mobility but results in disproportionate redundancy with aging.6,9 Relatively abrupt transition from thicker malar and brow skin renders the eyelids distinct and it should be respected when developing the reconstructive plan. Advancement and transposition flaps using lid skin provide the best color, thickness, and texture match. The adult palpebral fissure measures on average 10 to 12 mm vertically (midpupillary line) and 28 to 33 mm horizontally (horizontal palpebral aperture), with the upper eyelid covering upper limbus 1 to 2 mm, and the lower eyelid margin typically resting at the inferior limbus. The distance from the lateral canthus to the orbital rim is approximately 5 mm, and it is positioned approximately 2 to 4 mm higher than medial canthus. The upper and lower eyelid meet at an angle of ~60 degrees.6,7,8,9 The highest point of the upper eyelid is just nasal to the midpupillary line, while the lowest point of the lower eyelid is lateral to the midpupillary line. The lateral canthus stabilizes the eyelid in direct apposition to the globe, while the medial canthus is more anteriorly located and is intimately associated with lacrimal sac.6,9
The upper eyelid crease (formed by the attachment of levator aponeurosis [LA] which interdigitates with orbicularis oculi at the superior tarsal margin) is typically 7 to 8 mm above the lid margin in men, and 10 to 12 mm in women. In Asians, the upper lid crease is much lower or absent due to lower insertion of the septum or lower or absent insertion of the LA (2–3 mm above the lid margin).10,11 This anatomical arrangement allows the preaponeurotic fat to extend further into the eyelid. In the lower eyelid, septum fuses with capsulopalpebral fascia about 5 mm inferior to the tarsus forming the lower eyelid crease which is less visible and presents approximately 3 to 4 mm below the central and 5 to 6 mm below the lateral third of the lower lid margin, respectively.8,9
Interpalpebral distance of 10 to 12 mm can be further divided to margin-to-reflex distance (MRD) 1 (superior) and 2 (inferior) or MRD1 and MRD2. This is measured from the center of the pupil to the inferior edge of the upper eyelid, or superior edge of the lower eyelid, respectively. Its practical importance is the assessment of ptosis or eyelid retraction. Decreased intrapalpebral distance with a smaller MRD1 or MRD2 represents ptosis that can cause visual field obstruction. Increased interpalpebral distance with a higher MRD1 or MRD2 may mean eyelid retraction that causes exposure or ectropion.8,9,16 The contour of the eyelid needs to be respected in any reconstructive procedure to ensure naturally appearing lid margins and optimal aesthetic result.
The eyelid margin, when closely inspected, has multiple linear structures including lashes (anteriorly), Meibomian glands (posteriorly), and the gray line (in-between).6,8,9 Meibomian glands present the transition of anterior skin to orbital conjunctiva. Gray line is also known as the muscle of Riolan, which presents the most superficial extent of pretarsal orbicularis oculi muscle. This line presents important surgical landmark in tarsal strip procedure for reconstruction of the lateral canthus since it marks an anatomical separation of the anterior skin-muscle lamella from the posterior tarsus-conjunctiva lamella. The gray line also enables bloodless surgical dissection down to the septum and approach to the superior and inferior orbital margin.6,9
The most important differences between topography of the upper face in males vs. females are summarized in Table 10.1.
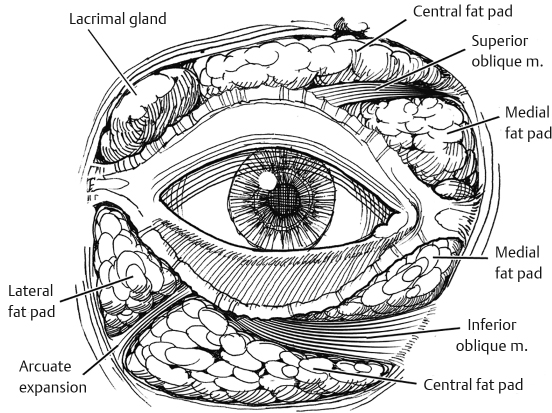
10.2.2 Orbicularis Oculi Muscle (OOM)6,8,9 (Fig. 10.3 and Fig. 10.4)
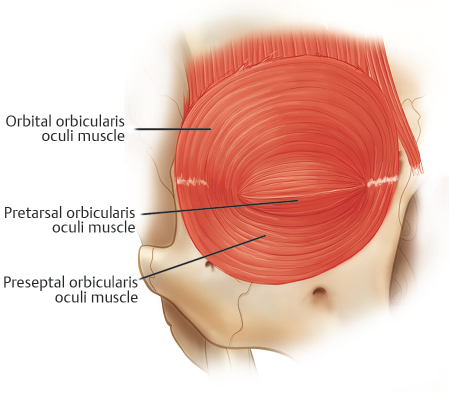
Fig. 10.3 Orbicularis oculi muscle. The muscle is traditionally divided into orbital and palpebral portions. The orbital portion arises from the anterior aspect of the MCT (medial canthal tendon) and the periosteum above and below it. The palpebral portion is further subdivided into pretarsal and preseptal portions, each lying over the tarsal plate or orbital septum, respectively. (Reproduced from Codner M, McCord C. Eyelid & Periorbital Surgery. 2nd ed. New York: Thieme; 2016.)
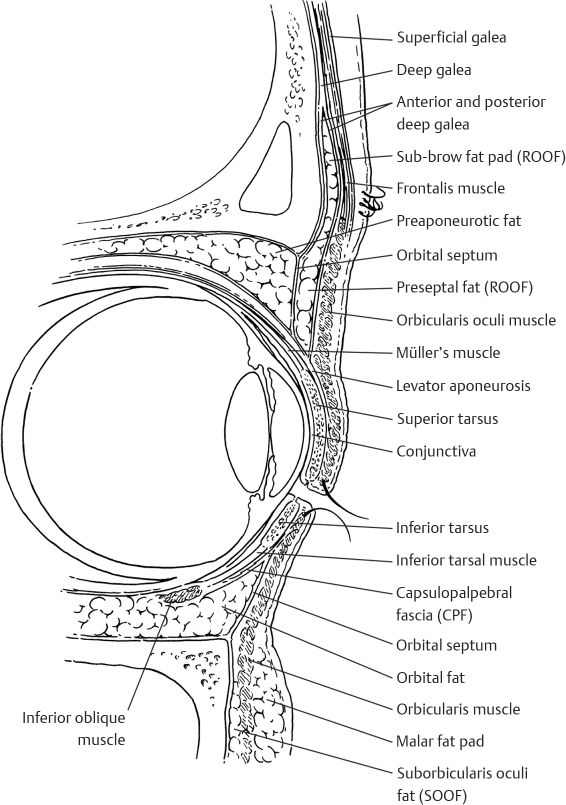
Fig. 10.4 Cross-sectional anatomy of the upper and lower lids and brows. The capsulopalpebral fascia and inferior tarsal muscle are retractors of the lower lid whereas Müller’s muscle, the levator muscle, and its aponeurosis are retractors of the upper lid. Note the preseptal positioning of retroorbicularis oculi and suborbicularis oculi fat (ROOF and SOOF, respectively). The orbitomalar ligament arises from the arcus marginalis of the inferior orbital rim and inserts on skin of the lower lid, forming the nasojugal fold. (Reproduced from Papel I, Frodel J, Holt R, et al. Facial Plastic and Reconstructive Surgery. 4th ed. New York: Thieme; 2016.)
The orbicularis oculi is a contiguous muscle composed of pars palpebralis (pretarsal and preseptal) and pars orbitalis. This is the main eyelid protractor involved in blinking or voluntary winking (palpebral part) or forced eyelid closure (orbital part). The upper and lower pretarsal segment originate from deep and superficial heads of the medial canthal tendon (MCT) and then extend laterally over upper and lower tarsal plate in a horizontal fashion to form the lateral canthal tendon (LCT). Preseptal part originates from the borders of MCT and overlays OS in both upper and lower lid and ends near the lateral horizontal raphe. Apart from helping with blinking reflex (corneal reflex) pretarsal part assists the lacrimal pump (medial pretarsal portion of OOM, aka as tensor tarsi or “Horner’s muscle”), maintains position of the canthal angle, and tightens the eyelid against the globe.
Posterior to OOM and anterior to OS lies the postorbicular fascial plane, which provides avascular plane for easy dissection and identification of the OS in ocular reconstruction. In this plane, there is also adipose tissue known as retroorbicularis oculi fat (ROOF) and suborbicularis oculi fat (SOOF). The ROOF is present beneath the ciliary portion of the brow and extends inferiorly under the orbital part of OOM. It contributes to eyebrow volume and helps mobility of lateral brow and eyelid. The SOOF continues inferiorly below the orbitomalar ligament which starts from arcus marginalis of bony orbit and inserts on the skin of the lower lid passing through fibers of OOM. The skin attachments of this ligament contribute to nasojugal and malar folds, respectively. Ptosis of the SOOF can lead to “malar bags” and contour deformities because the inferior orbital rim becomes exposed. In conjunction with the prolapse of the orbital fat (see following text), it can create characteristic “double contour” deformity of the lower eyelid. Hence, reposition of the SOOF is an important consideration in rejuvenation of the midface (Fig. 10.4).6,9
10.2.3 Orbital Septum (OS) and Postseptal Fat Compartments (Fig. 10.4 and Fig. 10.5)
The orbital septum is a thin sheet of fibrous multilayered connective tissue which arises circumferentially from the arcus marginalis of the orbital periosteum. It encircles the orbit as a continuation of the orbital fascial unit. The OS is very resistant to traction since it is firmly attached to arcus marginalis and as such can be easily identified during surgical procedure. In young patients it is relatively thick, while in older can be thin and dehiscent. Functionally, the OS acts as a barrier to infection and hemorrhage. In Caucasian upper lid, OS usually fuses with the LA approximately 3 to 5 mm above the tarsus, although it can vary from 0 to 15 mm from the superior tarsal edge. The fusion is more inferior or absent in Asian lids. In the lower lid OS fuses with capsulopalpebral fascia about 5 mm below the inferior tarsal plate.8,9
The postseptal orbital fat compartments (preaponeurotic fat pads) are divided in superior and inferior ones. Superior compartments comprise medial or nasal and central or preaponeurotic pads. The medial and central fat pads are separated by the trochlea, the tendon of superior oblique muscle and the median horn of the LA along with thin fascial strands of Whitnall’s ligament (superior transverse ligament), which further extends laterally over the lacrimal gland (located in the lateral upper eyelid postseptal compartment) to the superior edge of the rectus muscle. This ligament lies deep to the levator, forms a sleeve around levator palpebrae superioris, and acts as a pulley for this muscle. The medial fat pad is firmer and paler and is intimately adjacent to the medial palpebral artery and supratrochlear nerve. The preservation of the trochlea is of utmost importance in ptosis surgery, since its damage may result in superior oblique palsy or Brown’s syndrome.11,12
The inferior orbital fat pads are divided into lateral, central, and medial pads. The inferior, central, and lateral compartments are continuous, separated anteriorly by Lockwood’s ligament (suspensory ligament of the eye) (arcuate extension of capsulopalpebral fascia and inferior oblique muscle) while inferior, oblique muscle separates medial and central pads. The Lockwood’s ligament is actually condensation of capsulopalpebral fascia (see following text) and serves as supportive sling for the globe. The lower eyelid medial fat pad is firmer and paler as the nasal one in the upper eyelid. It is important to avoid damage of the inferior oblique muscle when exploring or manipulating the medial fat pad, since that may result in diplopia and strabismus. Weakening of the OS can produce prolapse of postseptal fat anteriorly in both upper and lower eyelids; since the fat itself is intact these are called pseudoherniations. Prolapse of the lacrimal gland should not be mistaken for fat pad in the upper eyelid, and one should avoid excising it accidentally. The lacrimal gland can be differentiated from preaponeurotic fat by its firm, tan color, vascular, lobulated structure to avoid perioperative injury.6,9
Central preaponeurotic fat pads in both upper and lower eyelid are important surgical landmarks since they lie anterior to eyelid retractors and immediately posterior to OS. The lateral fat pad in the lower eyelid extends superiorly between the OS and the LCT and acts as a bursa during eyelid movements (Eisler’s pocket).9 The OS should not be sutured or repaired directly without traction of the eyelid in the opposite direction since there is a risk of significant eyelid retraction and lagophthalmos. Conversely, it is of utmost importance to identify eyelid retractors (levator aponeurosis or capsulopalpebral fascia) and separate it from OS before advancing one or the other in the eyelid reconstruction. Otherwise, significant shortening of the repaired eyelid may develop and result in lagophthalmos.9
10.2.4 Tarsoligamentous Sling (Fig. 10.6)
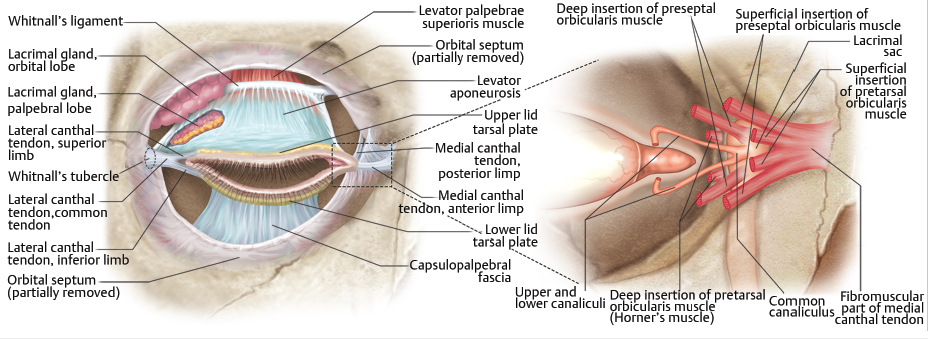
Fig. 10.6 Major retractors of the upper and lower eyelids (left) and medial canthal tendon structure (right): superior tarsal plate, lateral horn of levator aponeurosis, inferior tarsal plate, Lockwood’s suspensory ligament, Whitnall’s suspensory ligament, levator aponeurosis, medial horn of levator aponeurosis, and capsulopalpebral fascia. (Reproduced from Watanabe K, Shoja MM, Loukas M, Tubbs RS. Anatomy for Plastic Surgery of the Face, Head, and Neck. New York: Thieme; 2016.)
Tarsal plates anatomically resemble cartilaginous structures but are actually made of dense fibrous tissue which is approximately 30 mm in length and 1 mm in thickness. Along with MCT and LCT they form a tarsoligamentous sling which provides support for the eyelids, as well as lattice for the insertion of the OS and muscles of eyelid retraction. The pretarsal skin is firmly attached to the underlying tarsal plate contrary to highly elastic preseptal skin, thereby allowing intense edematous response of preseptal eyelid at the postsurgical period. The superior tarsus is approximately 8 to 12 mm high, while the inferior eyelid tarsus is approximately one-third of its height (i.e., 4–5 mm). In Asian patients the tarsus measurements differ slightly with superior tarsus being up to 8 mm and inferior 5 mm high, respectively. The underside of each tarsus is aligned by densely adherent palpebral conjunctiva. Tarsal plates contain 20 to 30 vertically aligned multilobulated Meibomian glands which secrete important component of the tear film to prevent excessive tear evaporation and “dry eye” syndrome. The glands open on the posterior eyelid margin right behind the gray line.6,8
The medial canthal tendon (MCT; Fig. 10.6) is the centerpiece of medial canthal anatomy. It has an elastic lateral portion that supports lacrimal canaliculi and then splits in the anterior, superior, and posterior limbs, all of which then blend into the lacrimal sac fascia. The thicker anterior limb inserts on the orbital process of the maxillary bone (anterior to the lacrimal crest) and is formed by superficial head of the pretarsal orbicularis muscle. The thinner posterior limb is the extension of the fascia of deep head of the pretarsal orbicularis and inserts on the posterior lacrimal crest. The superior branch extends to lacrimal sac apex and covers it anteriorly and superiorly. These arrays of fibrous bands work as an isolated soft-tissue pump of the lacrimal drainage system and insert on the orbital process of the frontal bones. The posterior head of the preseptal OOM inserts here forming the soft tissue roof of the lacrimal sac fossa.6,7,9
The lateral canthal tendon (LCT) anchors the tarsal plates and lateral regions of pretarsal/preseptal orbicularis to orbital wall posteriorly and superolaterally to Whitnall’s tubercle, 1.5 mm inside the lateral orbital margin. This unique anchoring system allows the lateral canthal angle to move in both vertical and lateral directions with the lateral gaze. Surgical manipulation of this structure is sometimes required to prevent unwanted ectropion and maintain lid globe apposition. The LCT measures 1 mm in thickness, 5 to 7 mm in length, and 3 mm in width at the point where superior and inferior crus unite. Then it broadens to 6 to 7 mm before its lateral insertion. At the superior edge, LCT blends with the lateral horn of the LA, inferolateral fibers of Whitnall’s superior suspensory ligament, and lateral portion of Lockwood’s inferior suspensory ligament (lateral retinaculum). The inferior crus of the LCT is divided in the lateral tarsal strip procedure (see following text) and for the tension release during canthotomy and cantholysis in the lower eyelid repair. The superior crus of LCT is divided for the tension release in the upper eyelid reconstruction (see following text). The intimate relationship with the lateral retinaculum (see earlier in the chapter) should be respected when performing division of the superior crus to avoid injury of this structure as well as palpebral part of the lacrimal gland.1,2,8
10.2.5 Eyelid Retractors (Fig. 10.2 and Fig. 10.4)
The primary upper eyelid retractors are levator palpebrae superioris (innervated by oculomotor nerve) and superior tarsal (Müller’s) muscle (innervated by sympathetic nervous system).7,9 The proximal (muscle portion) of levator palpebrae arises from greater wing of sphenoid bone and is 40 mm long, while the distal aponeurotic portion is 14 to 20 mm long aka levator aponeurosis (LA). This transition occurs at the region of Whitnall’s ligament (see earlier in the chapter) where the central part inserts on the anterior tarsus while the lateral horns separate lacrimal gland in orbital and palpebral portion before they insert onto the LCT. Medial portion of the aponeurosis inserts on the posterior portion of the MCT. The LA comprises actually two layers: anterior (thicker with few muscle fibers) which fuses with OS few millimeters above the tarsus and posterior (thinner, more elastic) with the attachment the both the lower third of the tarsal plate and eyelids’ subcutaneous tissue forming upper eyelid crease (see earlier in the chapter). With age, LA tends to elongate leading to involutional ptosis which can be usually corrected with the advancement of the aponeurotic attachment. Müller’s muscle attaches to the anterior edge of the tarsal plate and is bordered anteriorly by LA and posteriorly by conjunctiva. It is responsible for 2- to 3-mm upper eyelid retraction and regulates the tension of the posterior lamella. The function of upper eyelid retractors is assessed by measuring the upper eyelid excursion, i.e., the movement of the upper eyelid from extreme downward gaze to extreme upward gaze with the eyebrow fixed by the digital pressure and is typically 10 to 15 mm.6–8,11
The primary retractor of the lower lid is capsulopalpebral fascia (CPF) and the inferior tarsal muscle, both of which ultimately attach to the lower tarsal plate. The CPF arises from rectus inferior muscle (capsulopalpebral head) as dense connective tissue expansion, wraps anteriorly around oblique inferior muscle, and contributes to Lockwood’s ligament (see earlier in the chapter). At this point, the majority of fascia invests into the inferior border of the lower lid tarsal plate, with projections to the skin and the formation of the lower lid crease. It also fuses with OS several millimeters below the tarsal plate. The loss of attachments of CPF to tarsus can cause rotational instability of the lower eyelid and entropion. The inferior tarsal muscle is less developed than its superior counterpart and arises near the capsulopalpebral head, runs under the CPF, and inserts few millimeters below the inferior border of lower lid tarsus. Fortunately, disruption of this smooth muscle during surgery rarely results in eyelid malposition.6,8,11
10.2.6 Conjunctiva
The conjunctiva comprises a nonkeratinizing epithelium which lines the inner portion of the eyelid and is further divided into bulbar (covering large portion of the sclera to corneal limbus), palpebral (covering posterior tarsal surface and tarsal muscle), and forniceal (superior and inferior) covering apical interface of the eyelids and globe.7–9 Conjunctival fornices have redundant tissue, permitting eyes to move freely. A healthy conjunctiva contains copious goblet cells which produce mucin for lubrication, as well as accessory lacrimal glands. Significant conjunctival loss can result in motility deficits, lid malposition, and ocular surface damage. Conjunctiva of the superior and inferior fornix, being redundant and freely movable, could also be advanced to substitute the loss of tarsal conjunctiva during periocular reconstruction. The superior fornix is stated to be about 10 mm above the superior corneal limbus, and the inferior fornix is about 8 mm below the inferior corneal limbus. They are supported by fine suspensory ligaments deriving from levator muscle and superior rectus (superior fornix) and Lockwood’s ligament (inferior fornix). The medial canthus contains the caruncle which is modified skin with hair follicles, accessory lacrimal glands, sweat glands and sebaceous glands, and the plica semilunaris—a vertical fold lateral to the caruncle. The juncture between plica semilunaris and caruncle is surgically important as an access plane to the medial orbital wall.9
10.2.7 Lacrimal System (Fig. 10.7)
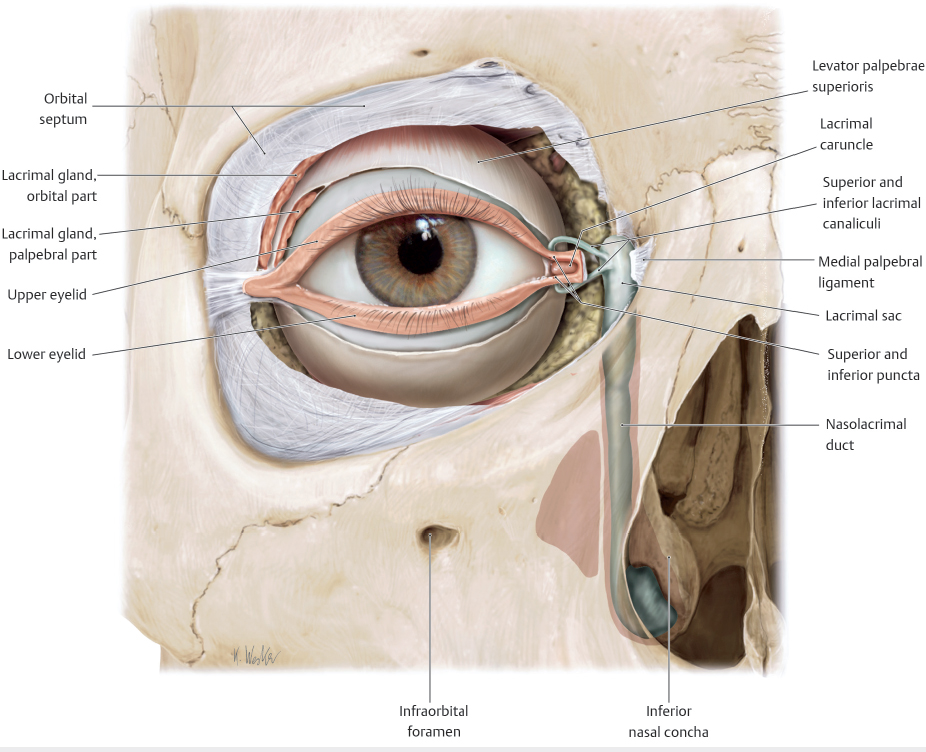
Fig. 10.7 Nasolacrimal drainage system. (Reproduced from Schuenke M, Schulte E, Schumacher U. Thieme Atlas of Anatomy: Head and Neuroanatomy. Illustrations by M. Voll and K. Wesker. 1st ed. Stuttgart: Thieme; 2010.)
The lacrimal gland9 consists of two lobes (orbital and palpebral) divided by the LA. The adjacent palpebral lobe drains aqueous tears into the superolateral fornix, where significant scarring can result in xerophthalmia (dry eye). The “wiper-blade” action of OOM and tarsal plates moves tears from laterally to medially toward the lacrimal puncta located 5 to 7 mm lateral to the medial canthal angle. Blinking creates a pump function to drain the tears through the superior and inferior canaliculus to a common canaliculus (90% of the time), passing first through their vertical segment (2 mm) and then the horizontal one (8 mm). The inferior lacrimal punctum is placed 1 to 2 mm more laterally than the superior one.6,9 The tears then drain into the lacrimal sac. The fundus of the lacrimal sac is approximately 5 mm above MCT and the body extends 10 mm inferiorly giving rise to nasolacrimal duct. The duct has intraosseous (proximal) portion and membranous (distal) portion before its termination into the nasal cavity. Canalicular disruption during eyelid surgery or punctal malposition after eyelid repair may result in epiphora. Obstruction of the lacrimal drainage system could be prevented by canaliculoplasty or silicone stent placement along with careful attention to the repair of the eyelid margin8,9 (see following text).
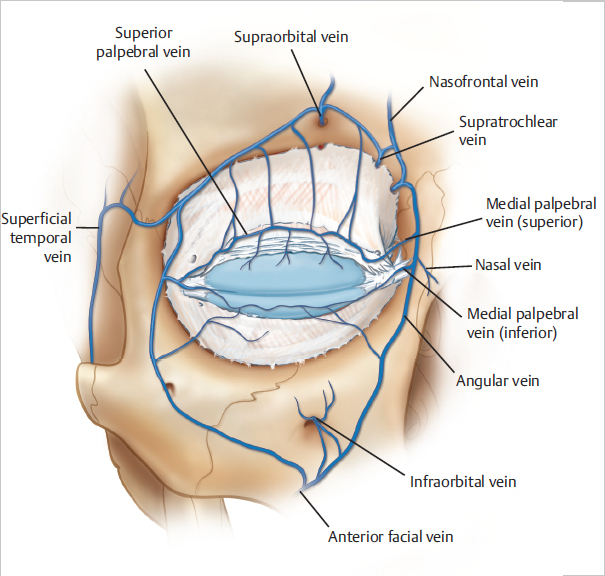
10.2.8 Neurovascular and Lymphatic System of the Lids (Fig. 10.8, Fig. 10.9, and Fig. 10.10a, b)
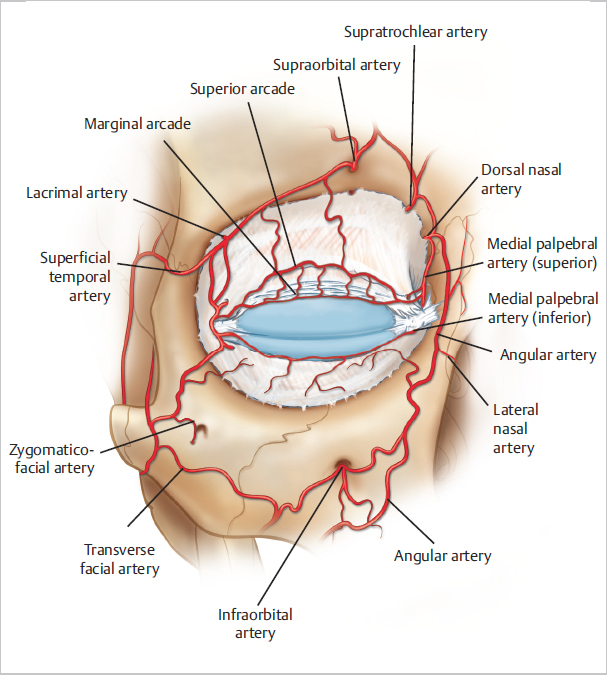
Fig. 10.8 Arterial supply to the eyelids. (Reproduced from Nahai F, Nahai F. The Art of Aesthetic Surgery: Principles & Techniques. 3rd ed. New York: Thieme; 2020.)
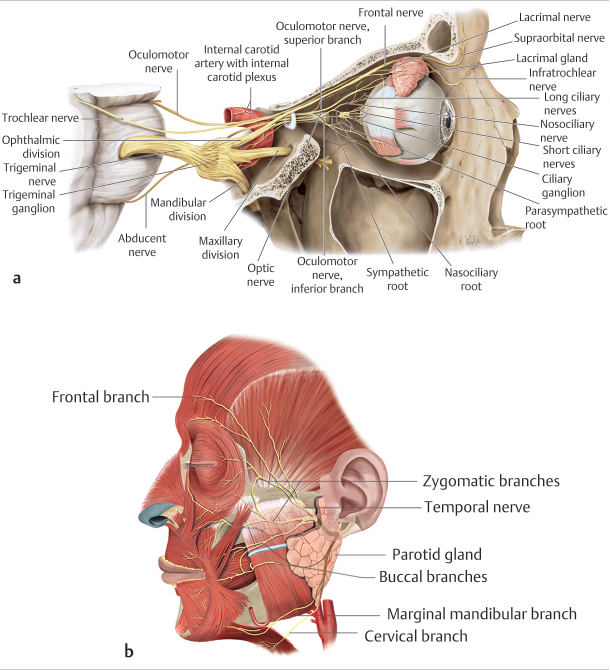
Fig. 10.10 (a) Sensory nerves from the eyelids via trigeminal nerve branches. (Reproduced from Schuenke M, Schulte E, Schumacher U. Thieme Atlas of Anatomy: Head and Neuroanatomy. Illustrations by M. Voll and K. Wesker. 1st ed. Stuttgart: Thieme; 2010.) (b) Motor innervation to the eyelid protractors from facial nerve branches. (Reproduced from Leatherbarrow B. Oculoplastic Surgery. 3rd ed. New York: Thieme; 2019.)
The main vascular supply of the lids comes from distal branches of internal and external carotid artery system.6–9 The ophthalmic artery is the first branch of the internal carotid system supplying the globe, orbital soft tissues and overlying eyelids. It continues anteromedially from orbital apex and divides into lacrimal and supraorbital artery, and then distally becomes nasofrontal artery which divides into supratrochlear and dorsal nasal arteries behind the trochlea.
The branches of lacrimal artery laterally and dorsal nasal artery medially give rise to superior and inferior lateral and medial arteries, respectively, which anastomose over the eyelids forming the superior peripheral arcade located within Müller’s muscle in the upper eyelid and the upper and lower eyelid marginal arcades. In addition, two other orbital margin arcades (deep and superficial) are formed in the superior orbit in-between the fibers of OOM (supratrochlear artery). Vascular contributions from the external carotid system are temporal superficial artery, infraorbital artery, and angular artery (terminal branch of facial artery). In 20% of cases, the lacrimal artery arises from the external carotid system.6,9
The venous system of the eyelids is developed mainly in the fornices and drains into both the anterior facial veins and veins of the intraorbital system via the superior ophthalmic vein and its tributaries (supratrochlear and supraorbital veins). Pretarsally, the angular vein drains the medial portion of the eyelid, and the superficial temporal vein drains the lateral portion of the eyelid. The superior and inferior ophthalmic veins, pterygoid plexus, and angular vein flow to the cavernous sinus and are involved in the venous drainage of postseptal structures. Another prominent structure is the supraorbital vein going along the brow’s arch and is formed by confluence of supraorbital, supratrochlear, and angular vein tributaries.6,7
The lymphatics of the eyelids can be divided into a superficial (pretarsal) plexus and deep (posttarsal) plexus. Damage to this network during surgery can produce chemosis (conjunctival edema) postoperatively. Furthermore, primary drainage from the medial lids is into the submandibular lymph nodes, while lateral lids drain into the preauricular (parotid) lymph nodes. Recent studies in primates revealed that the entire upper lid, medial canthus, and lateral lower lid drain into parotid nodes, while the central lower lid drains into the submandibular network. This pattern suggests that central upper eyelid probably has dual lymphatic drainage.2,7,8,9
Lymphatic mapping is usually required to identify the primary pathway of drainage when evaluating patients with melanoma of the eyelid as there are frequent variations to the location of the sentinel lymph node.
The motor nerve supply of the eyelids derives from the facial nerve (VII) with the zygomatic branch being the main supply for OOM (eyelid protractor) and secondary innervation from the temporal branch. The main upper eyelid retractor—levator palpebrae superioris—is innervated by the oculomotor nerve (III).7,9
The sensory supply of the eyelids derives from the ophthalmic (V1) and maxillary (V2) divisions of trigeminal nerve (V). The branches of the ophthalmic nerve which supply upper eyelid laterally to medially are lacrimal, frontal (supraorbital and supratrochlear), and nasociliary nerves. The branches of maxillary nerve which provide sensory innervation are zygomaticotemporal (lateral upper eyelid), zygomaticofacial (lateral lower eyelid), and infraorbital (central lower eyelid) nerve. The medial canthus is innervated by the infratrochlear nerve, i.e., terminal branch of the nasociliary nerve (V1). Sympathetic fibers innervate both upper and lower tarsal muscle.2,8,9
10.2.9 Orbit (Fig. 10.6 and Fig. 10.10a)
The bony orbit consists of maxilla, zygoma, sphenoid, palatine bone, ethmoid bone, lacrimal bone, and frontal bones. The lacrimal fossa is positioned in the lateral orbit formed by the frontal bone. The arcus marginalis is the outline of the outside margin of the orbit where periosteum of the orbit is fused with OS and is also the location of the attachment of the orbitomalar ligament. On the lateral orbit wall there is Whitnall’s tubercule which is the place of the attachment of the LCT.7,9
10.2.10 Eyebrow Anatomy
The eyebrow is comprised of the skin and soft tissue.7,15 The anatomic boundaries of the brow are demarcated superiorly by the first forehead crease curing above the brow skin and inferiorly at the arcus marginalis where subciliary brow ends, at the superior orbital rim, transitioning into the upper eyelid skin. Eyebrow hair follicles have different and limited growth pattern than the ones on the scalp, and once lost may be difficult to be replaced in the reconstructive procedures15 (Fig. 10.11). Deep to the follicles is a paired corrugator supercilii muscle which originates at the superior orbital rim medially and runs laterally till the lateral third of the brow along the superior orbital rim and is responsible for vertical lines on the glabella. Procerus muscle is positioned more centrally, extending distally from the nasal root and creates horizontal lines in the central glabellar region. Apart from these strong depressors, OOM and depressor supercilii muscles also augment the brow depressing function against the principal brow elevator frontalis muscle (Fig. 10.12). The vertical fibers of the frontalis muscle and the horizontal fibers of the orbicularis oculi muscles interdigitate at the eyebrow level; thus, the position of the eyebrow represents a dynamic interplay between elevating and depressing forces9,13,15 (Fig. 10.13).
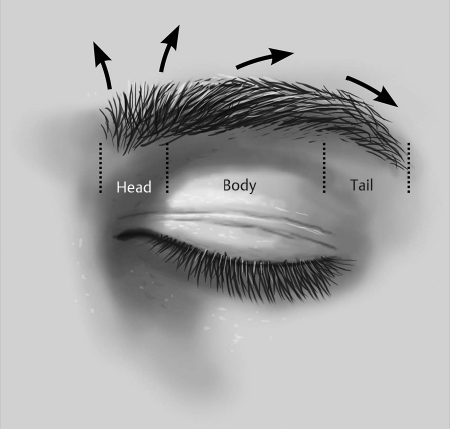
Fig. 10.11 Eyebrow segments (head, body, and tail) and multidirectional orientation of the hair growth.
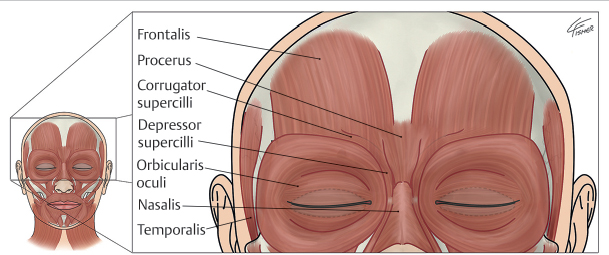
Fig. 10.12 Muscles of the forehead and temporal fossa. (Reproduced from Carniol P, Avram M, Brauer J. Complications in Minimally Invasive Facial Rejuvenation: Prevention and Management. New York: Thieme; 2020.)
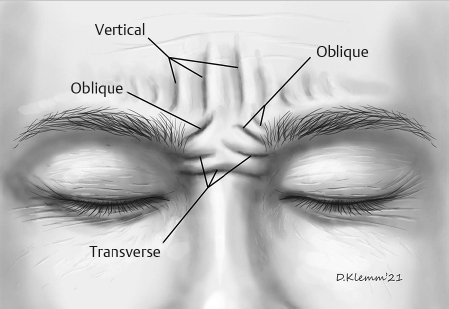
Fig. 10.13 Glabellar skin lines. Vertical skin lines are produced by action of the transverse heads of the corrugator supercilii muscles. Oblique skin lines are the result of action of three muscles: the oblique head of the corrugator supercilii, the depressor supercilii, and the medial head fibers of the orbicular oculi muscles. Action of the procerus muscle produces transverse skin line formation across the dorsum of the nose.
The frontalis muscle is a part of the occipitofrontalis musculofascial complex of the scalp, which includes the occipitalis muscle, galea aponeurotica, and frontalis muscle. The vertically oriented fibers of frontalis muscle extend from the broad fibrous tissue of the galea aponeurotica just inferior to the hairline and insert into the supraorbital dermis. Contraction of the frontalis muscle can elevate the eyebrow more than 20 mm and also causes horizontal furrows across the forehead. These furrows do not extend to the temporal hairline because the frontalis muscle thins laterally and does not extend past the temporal fusion line to the tail of the brow. The lack of frontalis pull-over of the tail of the brow explains the common temporal brow ptosis seen so often in older adults. The frontal branch of the facial nerve innervates the frontalis muscle.8,13,15
The galea aponeurosis13,15 joins the frontalis muscle anteriorly and splits around the frontalis muscle into a superficial and deep galea. The thinner superficial layer continues inferiorly as the anterior muscle sheath of the frontalis and orbicularis muscles, whereas the deep galea becomes the posterior muscle sheath. This deep galea layer divides inferiorly and encompasses the fat pad that lies beneath the interdigitation of the frontalis and orbicularis muscles of the ROOF (see earlier in the chapter).
The sensory innervation of the eyebrows derives from supraorbital and supratrochlear nerves, which also have paired arteries and veins. The supratrochlear notch projects 17.5 mm from the midline, and both nerves are branches of the trigeminal nerve (ophthalmic nerve V1). The motor innervation of paired corrugators and procerus is from frontal branches of the facial nerve. Lymphatics generally follow the neurovascular bundles and travel laterally toward the orbital rim.8
10.3 Principles and Aims of Periocular Reconstruction
Dermatologic surgeons have many surgical options to choose from for the repair of eyelid defects after Mohs micrographic surgery. The choice of the repair depends on the size and location of the defect, skin texture and color match, surrounding tissue mobility, degree of vascular compromise, and extend of the lamellae loss. All reconstruction effort should attempt to maintain the integrity of reconstructed structures by following the rules of “like for like” approximation.1 For extensive defects which require excessive mobilization of the tarsus, conjunctiva and skin consultation of experienced oculoplastic surgeon may be considered.
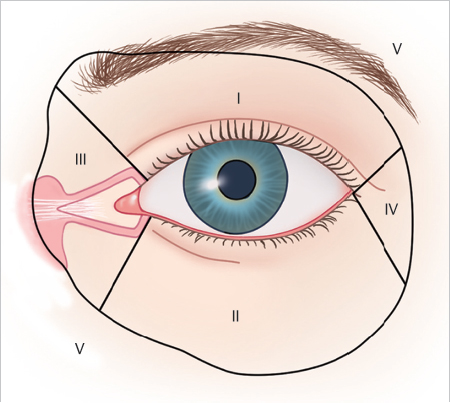
According to Spinelli,17 periocular area is divided into five anatomic units: the upper eyelid is zone 1, the lower eyelid is zone 2, the medial canthus is zone 3, the lateral canthus is zone 4, and tissue outside these zones, but still related to them is zone 5 (Fig. 10.14). According to Mutlu et al,18 the majority of skin cancers involve zone II and III (75%), which may be helpful to guide novices in the field of periocular reconstruction how and where to begin their education in surgical techniques. The defects are also classified as partial (anterior lamella, i.e., skin and OOM) or total (anterior and posterior lamella—skin, OOM, tarsus, conjunctiva, eyelid retractors); marginal (ciliary margin involvement) or nonmarginal.1,2 Furthermore, medial canthal involvement may require silicone stenting, repair of the lacrimal canaliculi, or lateral canthotomy if margin advancement is necessary. Finally, the reconstructed eyelid should match in height and shape the contralateral one, with medial and lateral canthi being positioned symmetrically on both sides.2,3,4 Taking these things into consideration is necessary to maintain both function and aesthetics of the eyelid.