div class=”ChapterContextInformation”>
23. Surgical Reconstruction of Post-TURP Urethral Strictures
Keywords
TURPUrethral strictureProximal bulbar urethra23.1 Introduction
Lower urinary tract symptoms (LUTS) secondary to benign prostatic hyperplasia (BPH) affect men as early as the fifth decade of life, and the prevalence of symptoms increases with age [1]. Most patients are initially treated with medical therapy consisting of alpha blockers and/or 5-alpha reductase inhibitors. Patients with persistent symptoms, despite optimal medical therapy, are candidates for surgical intervention. Additionally, surgical intervention is indicated for patients with urinary retention, renal failure, recurrent urinary tract infections, bladder stones, and recurrent hematuria.
Transurethral resection of the prostate (TURP) is the gold standard for the surgical management of benign prostatic obstruction. As with any surgical intervention, there are risks for complication including urethral stricture disease. The incidence of urethral stricture disease after transurethral resection of the prostate can be as high as 9.8% [2.2–9.8%] [2]. According to Rassweiler et al., the most common locations for strictures after TURP are the fossa navicularis and the bulbar urethra. The etiology of these strictures are related to either the difference in size between the fossa navicularis and the resectoscope or thermal injury due to leak of current causing urethral injury that later results in a stricture [3]. A recent multivariate analysis by Tao et al. demonstrated that urethral mucosa rupture and continued infection were also risk factors for urethral stricture after TURP leading to possible panurethral strictures [4, 5].
23.2 Evaluation
Patients with recurrent obstructive LUTS (weak urinary stream, straining to void, hesitancy and incomplete bladder emptying) within the first year after TURP merit evaluation for urethral stricture disease as the cause of their symptoms. Initial evaluation should consist of a complete history and physical exam with emphasis on surgical history, urethral instrumentation, and any significant factors that may represent a contraindication for surgical intervention and buccal graft harvest. Use of the International Prostate Symptom Score (IPSS) questionnaire and uroflowmetry at the time of initial evaluation are also helpful tools to better characterize the patient’s symptoms.
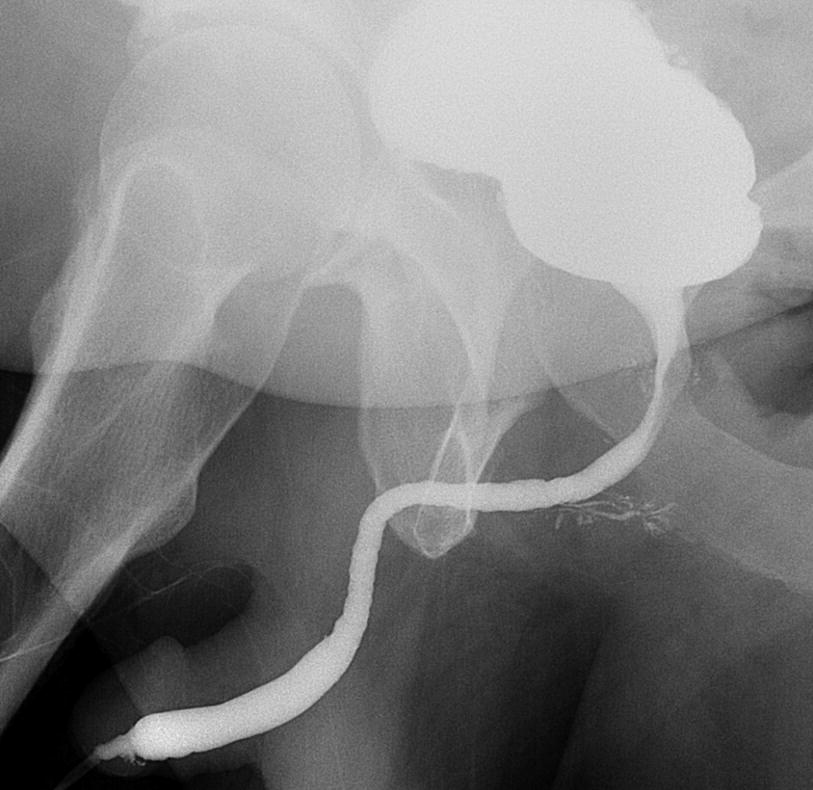
VCUG showing a tight fossa navicularis with mild irregularities within the bulbar urethra. (Imaging courtesy of Joseph Pariser, MD)
23.3 Surgical Reconstruction Techniques
As stated before, patients with urethral stricture after TURP pose a diagnostic and management challenge due to the possibility of multifocal strictures, the proximity of proximal bulbar strictures to the striated sphincter and/or in some cases, involvement of the entire anterior urethra. It is important to recognize that proximal bulbar strictures have been misnomered in the past as true membranous urethral strictures when in fact stenosis that affects the membranous urethra is uncommon in the absence of radiation [6].
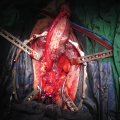
There is a risk of incontinence associated with the surgical repair of proximal bulbar strictures, and it is relatively high since urinary continence in men after TURP is mainly achieved by the striated sphincter. Any dissection near the sphincter theoretically increases the incidence of iatrogenic incontinence. Some authors have suggested a sphincter-sparing technique, as described by Gomez, is the ideal technique for short post TURP proximal bulbomembranous strictures [7]. Recently, Kulkarni et al. suggested that a ventral approach was technically better for post TURP strictures because it provides the ability to incise the mucosa without affecting the sphincter. This is the approach we use at our institution [8].
Although the most common locations for post TURP strictures are within the fossa navicularis or the bulbar urethra, patients can develop strictures anywhere along the urethra [8]. Most of the surgical techniques used at our institution for strictures after TURP are single-stage procedures that are used for idiopathic urethral strictures. Staged procedures are reserved for cases with extensive spongiofibrosis or recurrent strictures. Most of the techniques used are reviewed in previous chapters, thus we will briefly discuss the techniques used at our institution and provide some surgical pearls.
23.4 Urethral Meatus and Fossa Navicularis Strictures
Most patients with isolated stenosis or stricture of the distal penile urethra will describe their symptoms as an obstruction near the glans. If preoperative evaluation reveals an area of stricture 1 centimeter (cm) or less, patients are initially treated with a meatotomy. At 3 months, voiding symptoms and satisfaction with the cosmetic results are reassessed. If patients are not satisfied with the cosmetic results of their primary surgery, a staged repair with buccal graft can be considered.
Surgical steps/pearls for meatotomy |
|---|
Urethral meatus is incised ventrally with excision of the fibrotic tissue if necessary |
Neomeatus is calibrated to 24 French (Fr) to ensure urethral patency |
Mucosal edges are approximated with interrupted 4-0 Polyglactin sutures |
Pearl: Patients are allowed to void per urethra in the immediate postoperative period and do not require an indwelling catheter |
Surgical steps/pearls for a transurethral ventral onlay for fossa navicularis strictures |
|---|
A transurethral ventral urethrotomy is performed after adequate exposure is created with traction sutures at the 12, 4 and 8 o’clock positions on the glans penis |
Once the ventral urethrotomy is performed, the fibrotic tissue is removed between the 4 and 8 o’clock position. This is done until the proximal lumen is at least 24 Fr |
Pearl: Removal of the fibrotic tissue is essential to create the space necessary for the buccal graft |
A buccal mucosal graft is parachuted into the defect and fixed transurethrally using 6-0 Polydioxanone sutures |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree