High tibial osteotomy (HTO) is realignment surgery, which has developed for treating medial compartment osteoarthritis (OA) of the knee.7
 One of the main etiologic factors of knee OA is excessive biomechanical stress loaded on a focal area due to varus deformity of the lower limb alignment.
One of the main etiologic factors of knee OA is excessive biomechanical stress loaded on a focal area due to varus deformity of the lower limb alignment.
 Excessive biomechanical stress is loaded onto either compartment of the knee joint; consequently, such overload is more likely to give rise to degeneration of articular cartilage with aging.
Excessive biomechanical stress is loaded onto either compartment of the knee joint; consequently, such overload is more likely to give rise to degeneration of articular cartilage with aging.
 The aim of HTO is to correct malalignment of the limb, resulting in a transfer of weight bearing from the degenerated medial compartment to the relatively healthy lateral compartment.
The aim of HTO is to correct malalignment of the limb, resulting in a transfer of weight bearing from the degenerated medial compartment to the relatively healthy lateral compartment.
 Correction to appropriate knee alignment provides stability of the affected knee, subsidence of synovitis, and cease of cartilage degeneration.
Correction to appropriate knee alignment provides stability of the affected knee, subsidence of synovitis, and cease of cartilage degeneration.
 The indications for HTO include medial compartmental knee OA with or without instability and osteonecrosis of the knee.
The indications for HTO include medial compartmental knee OA with or without instability and osteonecrosis of the knee.
ANATOMY
 The proximal tibial portion for osteotomy has several important anatomic landmarks to obtain successful results and avoid complications.
The proximal tibial portion for osteotomy has several important anatomic landmarks to obtain successful results and avoid complications.
 On the anterior aspect of the proximal tibia, the tibial tuberosity is the most prominent feature. The osteotomy should be carried out at the proximal level of the tuberosity.
On the anterior aspect of the proximal tibia, the tibial tuberosity is the most prominent feature. The osteotomy should be carried out at the proximal level of the tuberosity.
 Gerdy tubercle is located at 2 to 3 cm lateral to the tibial tubercle, which is the insertion of the iliotibial tract. Gerdy tubercle is the most suitable place to place fixative devices because of the thick cortical bone.
Gerdy tubercle is located at 2 to 3 cm lateral to the tibial tubercle, which is the insertion of the iliotibial tract. Gerdy tubercle is the most suitable place to place fixative devices because of the thick cortical bone.
 On the medial aspect of the proximal tibia, there are insertions of the pes anserinus, the gracilis, and semitendinosus covered with the fascia, and on the posteromedial portion, the superficial layer of the medial collateral ligament is attached. In cases of medial soft tissue tightness, these sometimes need to be elevated subperiosteally.
On the medial aspect of the proximal tibia, there are insertions of the pes anserinus, the gracilis, and semitendinosus covered with the fascia, and on the posteromedial portion, the superficial layer of the medial collateral ligament is attached. In cases of medial soft tissue tightness, these sometimes need to be elevated subperiosteally.
 The anterior aspect of the proximal tibia and the fibula is the origin of the tibialis anterior, extensor digitorum longus, and peroneus longus muscles.
The anterior aspect of the proximal tibia and the fibula is the origin of the tibialis anterior, extensor digitorum longus, and peroneus longus muscles.
 On the lateral side, the common peroneal nerve runs on the lateral side of the neck of the fibula. On excision of the fibular head or division of the proximal tibiofibular ligament in closing wedge osteotomies, much attention should be paid to avoid nerve injury.
On the lateral side, the common peroneal nerve runs on the lateral side of the neck of the fibula. On excision of the fibular head or division of the proximal tibiofibular ligament in closing wedge osteotomies, much attention should be paid to avoid nerve injury.
 The posterior neurovascular structure, including the popliteal artery and vein and tibial nerve, should be protected while the posterior portion of the tibia is osteotomized.
The posterior neurovascular structure, including the popliteal artery and vein and tibial nerve, should be protected while the posterior portion of the tibia is osteotomized.
 The cross-section of the proximal tibia has a triangular shape. In opening wedge high tibial osteotomies (OW-HTO), the posterior portion of the osteotomized site should be opened more than the anterior portion to avoid an expected increase of the tibial slope.
The cross-section of the proximal tibia has a triangular shape. In opening wedge high tibial osteotomies (OW-HTO), the posterior portion of the osteotomized site should be opened more than the anterior portion to avoid an expected increase of the tibial slope.
 When performing fibular osteotomy in closing wedge high tibial osteotomies (CW-HTO), the fibular shaft can be resected safely at the level of about 16 cm distal to the fibular head.
When performing fibular osteotomy in closing wedge high tibial osteotomies (CW-HTO), the fibular shaft can be resected safely at the level of about 16 cm distal to the fibular head.
PATHOGENESIS
 Knee OA is a common joint disorder in elderly people that leads to progressive dysfunction of a knee joint.
Knee OA is a common joint disorder in elderly people that leads to progressive dysfunction of a knee joint.
 Knee OA develops and progresses due to risk factors including heredity, weight, age, gender, repetitive stress injury, and high-impact sports.
Knee OA develops and progresses due to risk factors including heredity, weight, age, gender, repetitive stress injury, and high-impact sports.
 Although the etiology of knee OA is multifactorial, medial compartmental knee OA reveals varus deformity, the mechanical axis passes through far medial side from a knee joint, and excessive mechanical stress loaded on the medial cartilage are considered to be main causative factors.
Although the etiology of knee OA is multifactorial, medial compartmental knee OA reveals varus deformity, the mechanical axis passes through far medial side from a knee joint, and excessive mechanical stress loaded on the medial cartilage are considered to be main causative factors.
 Excessive overload is more likely to give rise to degeneration of articular cartilage, and cartilage fragments entrapped by synovium induce synovial inflammation, resulting in further degeneration of articular cartilage.
Excessive overload is more likely to give rise to degeneration of articular cartilage, and cartilage fragments entrapped by synovium induce synovial inflammation, resulting in further degeneration of articular cartilage.
 Synovial inflammation is marked around the degenerated articular cartilage and related to joint swelling and provocation of pain.
Synovial inflammation is marked around the degenerated articular cartilage and related to joint swelling and provocation of pain.
NATURAL HISTORY
 Once a knee joint is affected by OA, the disease advances with time, and osteoblastic changes, including subchondral bone sclerosis and osteophyte formation, are clearly visible. Further cartilage degeneration occurs, resulting in joint space narrowing or obliteration.
Once a knee joint is affected by OA, the disease advances with time, and osteoblastic changes, including subchondral bone sclerosis and osteophyte formation, are clearly visible. Further cartilage degeneration occurs, resulting in joint space narrowing or obliteration.
 Range of motion (ROM) is gradually limited. Flexion contracture or restriction of the knee appears.
Range of motion (ROM) is gradually limited. Flexion contracture or restriction of the knee appears.
 However, quadriceps strengthening exercise or reducing body weight can modify the clinical course of the disease. These measures may stabilize a knee joint and reduce overload applied on the cartilage-degenerative portion, providing good relief of pain.
However, quadriceps strengthening exercise or reducing body weight can modify the clinical course of the disease. These measures may stabilize a knee joint and reduce overload applied on the cartilage-degenerative portion, providing good relief of pain.
 As the disease progresses, loss of articular cartilage brings about varus–valgus instability, so-called “lateral thrust.” This instability promotes further cartilage degeneration, producing bony wear at the medial femorotibial articulation, and varus deformity increases.
As the disease progresses, loss of articular cartilage brings about varus–valgus instability, so-called “lateral thrust.” This instability promotes further cartilage degeneration, producing bony wear at the medial femorotibial articulation, and varus deformity increases.
 Osteophytes formed around intercondylar notch and may cause anterior cruciate ligament (ACL) deficiency, and the disease expands to the lateral and the patellofemoral compartment.
Osteophytes formed around intercondylar notch and may cause anterior cruciate ligament (ACL) deficiency, and the disease expands to the lateral and the patellofemoral compartment.
 A knee joint is destructed and knee function is markedly disabled due to severe pain and limited ROM.
A knee joint is destructed and knee function is markedly disabled due to severe pain and limited ROM.
HISTORY AND PHYSICAL FINDINGS
 Diagnosis of knee OA can be made based on patient-reported symptoms and physical and radiologic examination.
Diagnosis of knee OA can be made based on patient-reported symptoms and physical and radiologic examination.
 Clinical examination of the knee should start with complete history of the symptoms; past history, including previous trauma such as fracture or meniscus tear; medical diseases, including diabetes mellitus or hypertension; and occupational history.
Clinical examination of the knee should start with complete history of the symptoms; past history, including previous trauma such as fracture or meniscus tear; medical diseases, including diabetes mellitus or hypertension; and occupational history.
 Knee pain is a crucial clinical sign of knee OA. Patients experience pain around a knee joint when standing up from a chair and starting to walk. This pain modality, called starting pain, is very specific for knee OA. Pain is also aggravated by physical activities such as descending or ascending stairs.
Knee pain is a crucial clinical sign of knee OA. Patients experience pain around a knee joint when standing up from a chair and starting to walk. This pain modality, called starting pain, is very specific for knee OA. Pain is also aggravated by physical activities such as descending or ascending stairs.
 Some patients complain of pain at night and morning stiffness.
Some patients complain of pain at night and morning stiffness.
 Asking patients about the onset of pain, the duration and frequency, and physical activities that aggravate pain is essential to help make differential diagnosis.
Asking patients about the onset of pain, the duration and frequency, and physical activities that aggravate pain is essential to help make differential diagnosis.
 The physical examination should cover posture, gait pattern, the involved limb, the joints on either side of the knee, the spine, and, particularly, the hip joint, which can also cause knee pain.
The physical examination should cover posture, gait pattern, the involved limb, the joints on either side of the knee, the spine, and, particularly, the hip joint, which can also cause knee pain.
 Observation shows that a significant varus deformity at the knee, antalgic gait, and lateral thrust in early stance phase of gait visualized joint effusion and quadriceps muscle atrophy.
Observation shows that a significant varus deformity at the knee, antalgic gait, and lateral thrust in early stance phase of gait visualized joint effusion and quadriceps muscle atrophy.
 Palpitation indicates the exact location of pain around the tibiofemoral and patellofemoral joints. Tender zones are easily determined by asking patients to point to painful sites with one finger. When joint effusion exists, a ballotable patella is noticed. Crepitation, defined as a cracking or grinding sound, is identified when the patient with knee OA experiences a sensation in the joint during physical examination.
Palpitation indicates the exact location of pain around the tibiofemoral and patellofemoral joints. Tender zones are easily determined by asking patients to point to painful sites with one finger. When joint effusion exists, a ballotable patella is noticed. Crepitation, defined as a cracking or grinding sound, is identified when the patient with knee OA experiences a sensation in the joint during physical examination.
 Pain is often provoked at the medial joint space by valgus-stressed maneuvers because more marked synovitis and osteophyte formation are present in medial compartmental knee OA.
Pain is often provoked at the medial joint space by valgus-stressed maneuvers because more marked synovitis and osteophyte formation are present in medial compartmental knee OA.
IMAGING AND OTHER DIAGNOSTIC STUDIES
 Routine radiographic examination of knee OA consists of standing (weight bearing) anteroposterior (AP) and lateral views and tangential axial views. Other views include the tunnel view, 45-degree flexed weight-bearing posteroanterior (PA) view, varus or valgus stress views, and a full-length standing radiograph (a mechanical axis view).
Routine radiographic examination of knee OA consists of standing (weight bearing) anteroposterior (AP) and lateral views and tangential axial views. Other views include the tunnel view, 45-degree flexed weight-bearing posteroanterior (PA) view, varus or valgus stress views, and a full-length standing radiograph (a mechanical axis view).
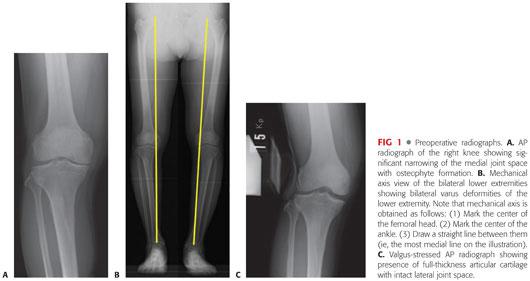
A standing AP view provides more accurate assessment of knee alignment and joint space width than one taken in the supine position (FIG 1A).
A lateral view depicts the status of the extensor mechanism, including the patella height (patella alta or baja), the quadriceps and patellar tendon, the tibial posterior slope, the distal end of the femur, and the proximal end of the tibia.
Morphologic changes of the patellofemoral joint can be assessed using a tangential axial view (the Merchant view).
The tunnel view demonstrates osteophytes formed on the posterior aspect of the intercondylar notch.
The flexed, weight-bearing PA view of the knee reveals the joint space width of the more posterior aspect of the femorotibial joint. Early degenerative changes of the articular cartilage can be detected with this view.
A mechanical axis view provides exact alignment of the whole lower extremity. This view is commonly used in preoperative planning of HTO (FIG 1B).
The varus and valgus stress views are helpful to visualize the stability of medial and lateral laxity in medial knee OA and to confirm that the lateral compartment is almost intact (FIG 1C).
 Magnetic resonance imaging (MRI) provides multiplanar assessment of the pathology of the whole structure of a knee joint, including cartilage, synovium, ligaments, menisci, and bone marrow.
Magnetic resonance imaging (MRI) provides multiplanar assessment of the pathology of the whole structure of a knee joint, including cartilage, synovium, ligaments, menisci, and bone marrow.
 In medial compartmental knee OA, MRIs can satisfactorily depict the morphologic changes of articular cartilage from an irregular surface as the disease progresses, synovial hyperplasia, thick subchondral bone, the degenerative process of the medial meniscus, the condition of the ACL and medial collateral ligament, and bone marrow edema indicating overload applied to the articular surface.
In medial compartmental knee OA, MRIs can satisfactorily depict the morphologic changes of articular cartilage from an irregular surface as the disease progresses, synovial hyperplasia, thick subchondral bone, the degenerative process of the medial meniscus, the condition of the ACL and medial collateral ligament, and bone marrow edema indicating overload applied to the articular surface.
 Other diagnostic imaging tools include bone scintigraphy and positron emission tomography scan using fluorodeoxyglucose or 18F-sodium fluoride (18F-NaF).
Other diagnostic imaging tools include bone scintigraphy and positron emission tomography scan using fluorodeoxyglucose or 18F-sodium fluoride (18F-NaF).
DIFFERENTIAL DIAGNOSIS
 Osteonecrosis of the femoral condyle
Osteonecrosis of the femoral condyle
 Osteonecrosis of the tibial plateau
Osteonecrosis of the tibial plateau
 Charcot joint
Charcot joint
 Idiopathic joint apoplexy
Idiopathic joint apoplexy
 Elderly onset rheumatoid arthritis
Elderly onset rheumatoid arthritis
 Crystal-induced arthritis
Crystal-induced arthritis
 Pyogenic arthritis
Pyogenic arthritis
NONOPERATIVE MANAGEMENT
 Employment of a combination of pharmacologic and nonpharmacologic treatment is recommended for clinical practice (Osteoarthritis Research Society International recommendations for the management of hip and knee OA).25
Employment of a combination of pharmacologic and nonpharmacologic treatment is recommended for clinical practice (Osteoarthritis Research Society International recommendations for the management of hip and knee OA).25
 Patients should be instructed about the purpose of treatment and the importance of changes in lifestyle, pacing of activities, weight reduction, and the need for walking aids to reduce overload to the joint.
Patients should be instructed about the purpose of treatment and the importance of changes in lifestyle, pacing of activities, weight reduction, and the need for walking aids to reduce overload to the joint.
 A knee brace can reduce pain in knee OA with mild or moderate instability. Lateral-wedged insoles provide symptomatic relief for some patients with medial compartmental knee OA.
A knee brace can reduce pain in knee OA with mild or moderate instability. Lateral-wedged insoles provide symptomatic relief for some patients with medial compartmental knee OA.
 As pharmacologic treatments, acetaminophen is commonly used as an analgesic. Nonsteroidal anti-inflammatory drugs (NSAIDs) are recommended to be used at the lowest effective dose to prevent the increase of gastrointestinal risks. COX-2 selective agents should be used with caution in patients with cardiovascular risk factors. Glucosamine or chondroitin and weak opioids and narcotic analgesics may provide symptomatic benefits for patients with knee OA.
As pharmacologic treatments, acetaminophen is commonly used as an analgesic. Nonsteroidal anti-inflammatory drugs (NSAIDs) are recommended to be used at the lowest effective dose to prevent the increase of gastrointestinal risks. COX-2 selective agents should be used with caution in patients with cardiovascular risk factors. Glucosamine or chondroitin and weak opioids and narcotic analgesics may provide symptomatic benefits for patients with knee OA.
 Intra-articular injections with corticosteroids or hyaluronate can be used in the treatment of knee OA.
Intra-articular injections with corticosteroids or hyaluronate can be used in the treatment of knee OA.
SURGICAL MANAGEMENT
Indications
 The main indication for HTO is medial compartment knee OA, which does not provide adequate pain relief and functional improvement from a combination of nonpharmacologic and pharmacologic treatment.17,18
The main indication for HTO is medial compartment knee OA, which does not provide adequate pain relief and functional improvement from a combination of nonpharmacologic and pharmacologic treatment.17,18
 Patients with knee OA with lateral thrust are likely candidates for HTO.
Patients with knee OA with lateral thrust are likely candidates for HTO.
 Patients with osteonecrosis of the knee are also good candidates for HTO.
Patients with osteonecrosis of the knee are also good candidates for HTO.
 The ideal patients are physiologically young (younger than 55 years). However, a higher failure rate in obese or elderly patients of older than 65 years is not always identified. Old age and overweight patients are not contraindications for HTO.
The ideal patients are physiologically young (younger than 55 years). However, a higher failure rate in obese or elderly patients of older than 65 years is not always identified. Old age and overweight patients are not contraindications for HTO.
 Medial compartmental knee OA with less than 15 degrees of anatomic varus angulation and fixed flexion deformity of less than 15 degrees is indicated for OW-HTO. For other cases, CW-HTO should be considered as a surgical option.
Medial compartmental knee OA with less than 15 degrees of anatomic varus angulation and fixed flexion deformity of less than 15 degrees is indicated for OW-HTO. For other cases, CW-HTO should be considered as a surgical option.
 To perform HTO, the ACL must be functionally intact rather than insufficient. CW-HTO can decrease the tibial posterior slope and should be selected for ACL-deficient knee OA.
To perform HTO, the ACL must be functionally intact rather than insufficient. CW-HTO can decrease the tibial posterior slope and should be selected for ACL-deficient knee OA.
 Inflammatory knee arthritis or knee OA with involvement of both the medial and lateral compartment is not indicated for HTO.
Inflammatory knee arthritis or knee OA with involvement of both the medial and lateral compartment is not indicated for HTO.
Preoperative Planning
 At the beginning of preoperative planning, it is extremely important to check that the lateral joint space width is maintained in valgus-stressed AP knee radiographs because the postoperative main weight-bearing portion becomes the lateral compartment.
At the beginning of preoperative planning, it is extremely important to check that the lateral joint space width is maintained in valgus-stressed AP knee radiographs because the postoperative main weight-bearing portion becomes the lateral compartment.
 In planning for osteotomy, it is a basic principle to determine the location and direction of the osteotomy line and the desired angle of correction.
In planning for osteotomy, it is a basic principle to determine the location and direction of the osteotomy line and the desired angle of correction.
 Using a standing AP knee radiograph, a single osteotomy line is drawn from 35 mm of the point of the medial tibial cortex distal to the medial joint line to the proximal tibiofibular joint.
Using a standing AP knee radiograph, a single osteotomy line is drawn from 35 mm of the point of the medial tibial cortex distal to the medial joint line to the proximal tibiofibular joint.
 The desired postoperative knee alignment is 170 degrees of standing femorotibial angle (SFTA), which was proposed by Bauer and associates4 (10 degrees of anatomic valgus angulation). The desired angle of correction (θ°) is the angle calculated by subtraction of 170 degrees from the SFTA of the affected knee.
The desired postoperative knee alignment is 170 degrees of standing femorotibial angle (SFTA), which was proposed by Bauer and associates4 (10 degrees of anatomic valgus angulation). The desired angle of correction (θ°) is the angle calculated by subtraction of 170 degrees from the SFTA of the affected knee.
 From a point of intersection of the osteotomy line to the lateral tibial cortex, the base of a triangle (θ) is drawn, and the distance from the initial point of the osteotomy line to the point of intersection to the medial cortex is measured, which indicates the tibial width for opening the gap during operation.
From a point of intersection of the osteotomy line to the lateral tibial cortex, the base of a triangle (θ) is drawn, and the distance from the initial point of the osteotomy line to the point of intersection to the medial cortex is measured, which indicates the tibial width for opening the gap during operation.
Positioning
 The patient is positioned supine on the operating table with a sandbag inserted into the ipsilateral buttock region to place the lower extremity in neutral position (FIG 2).
The patient is positioned supine on the operating table with a sandbag inserted into the ipsilateral buttock region to place the lower extremity in neutral position (FIG 2).

 A pneumo-tourniquet is applied to the upper thigh area.
A pneumo-tourniquet is applied to the upper thigh area.
 Under preoperative fluoroscopy, it is necessary to check that the center of the femoral head, the ankle, and the position of the knee joint can be visualized.
Under preoperative fluoroscopy, it is necessary to check that the center of the femoral head, the ankle, and the position of the knee joint can be visualized.
Approach
 The approach for OW-HTO is a medial parapatellar incision from the lower part of the patella to 3 cm distal to the tibial tuberosity (FIG 3).
The approach for OW-HTO is a medial parapatellar incision from the lower part of the patella to 3 cm distal to the tibial tuberosity (FIG 3).
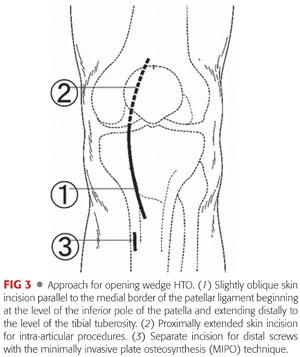
 When arthrotomy is needed for intra-articular procedures, including resection of osteophytes and resourcing articular cartilage, a longer skin incision is made from the upper part of the patella to distal to the tibial tuberosity, and the subvastus approach is commonly used.
When arthrotomy is needed for intra-articular procedures, including resection of osteophytes and resourcing articular cartilage, a longer skin incision is made from the upper part of the patella to distal to the tibial tuberosity, and the subvastus approach is commonly used.
TECHNIQUES
 Arthroscopy
Arthroscopy
A routine arthroscopic examination is performed through the anteromedial or anterolateral portal to determine the intra-articular pathology.
It is important to check the status of the articular surface of the lateral compartment because derangement of the articular cartilage influences the long-term clinical outcomes of HTO (TECH FIG 1A,B).
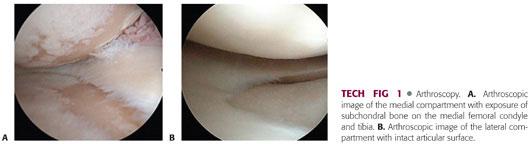
The condition of the ACL and the patellofemoral compartment are also investigated because OW-HTO is feasible to exacerbate the patellofemoral arthritis.
During arthroscopy, free body can be removed and meniscus tears are débrided if necessary. Bone marrow stimulation can be performed using a Kirschner wire or an ice pick.
 Opening Wedge High Tibial Osteotomy
Opening Wedge High Tibial Osteotomy
Initial Dissection
Bony anatomic landmarks, including relief of the patella tendon, the tibial tuberosity, a joint line, and Gerdy tubercle, are marked with a skin marker.
The medial parapatellar oblique skin incision is made from the lower part of the patella to 3 cm distal to the tibial tuberosity.
The incision is made through the skin and subcutaneous dissection is carried out until the anterior aspect of the proximal tibia covered by the sartorius fascia is exposed.
The fascia is longitudinally incised along both the medial and lateral margin of the patella tendon and the posterior insertion of the tendon is cleared for making a flange at the tibial tuberosity. The anterior aspect of the lateral side of the proximal tibia is also subperiosteally released for osteotomy (TECH FIG 2).
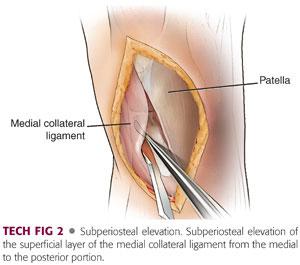
Insertion of hamstrings and superficial medial collateral ligament are released subperiosteally and the periosteum at the proximal tibia is elevated using a Cobb elevator from the medial to the posterior portion until the knee becomes slightly genu recurvatum.
The periosteum of the posterior portion of the tibia is thick and firm. The periosteum, associated with the muscle and soft tissue, is satisfactorily elevated to avoid unexpected neurovascular injury.
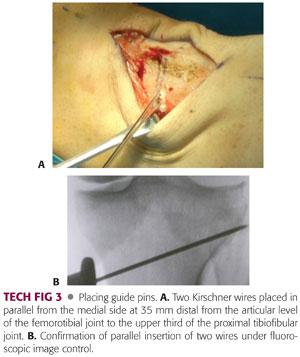
Placing Guide Pins
Under fluoroscopic image control, two Kirschner wires (2 mm in diameter) are inserted at the medial cortex, which is 3.5 cm below the medial joint surface (TECH FIG 3A) and directed in almost parallel line to the proximal tibiofibular joint, making an osteotomy plane (TECH FIG 3B).
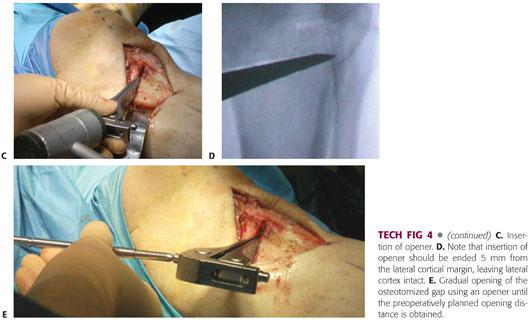
Osteotomy
When performing osteotomy, the medial and anterior cortical cut is made along the two Kirschner wires using a small oscillating bone saw (TECH FIG 4A), and the posterior, posterolateral and anterolateral cortical cut is made with thin osteotomes (TECH FIG 4B). The osteotomy is deepened. At this time, the lateral tibial cortex should remain intact.
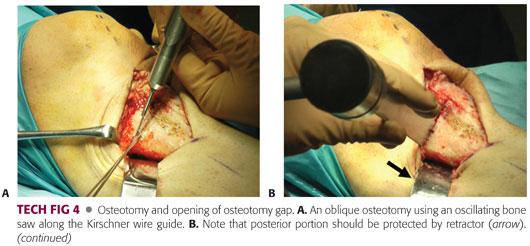
At the tibial tuberosity, an L-shaped osteotomy is performed to make a flange of about 2 cm in height. The height is determined based on the opening. Then incomplete osteotomy is achieved.
An opener is inserted from the osteotomized site (TECH FIG 4C) and to less than 10 mm of the lateral cortex (TECH FIG 4D). The separation of the proximal and the distal bone fragment is gradually accomplished with the use of an opener until the width of the gap is same as the distance measured in the preoperative radiograph (TECH FIG 4E). The limb alignment is supposed to be corrected to 170 degrees of SFTA (10 degrees of anatomic valgus angulation). The corrected alignment can also be used to check that the mechanical axis passes through the 62% coordinate along the tibial plateau using electrocautery.
Bone Grafting
The space is maintained with two spreaders inserted in the anterior and posterior side (TECH FIG 5A,B). Two wedge-shaped bone substitutes made of β-TCP (tricalcium phosphate) with 60% of porosity or bone grafts taken from the iliac crest are inserted into the opening space in order to reinforce mechanical strength against weight bearing and keep the corrected alignment (TECH FIG 5C,D).
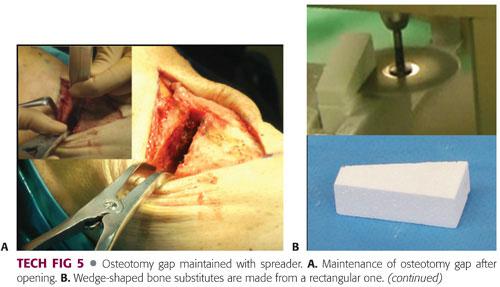
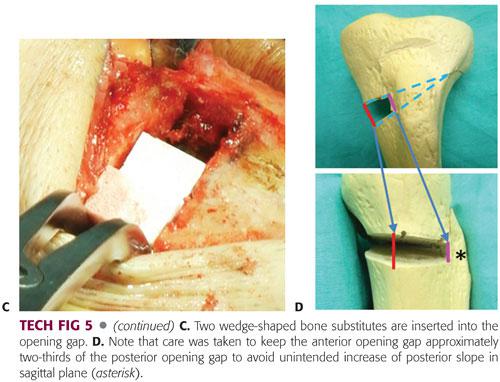
To maintain the natural tibial posterior slope, the first wedge-shaped bone substitute or allograft should be placed at the most posterior corner, and with knee extension, the base of wedge should be higher posteriorly than anteriorly (TECH FIG 5E). The size-adjusted second bone substitute or bone graft is inserted.
Plate Fixation and Closure
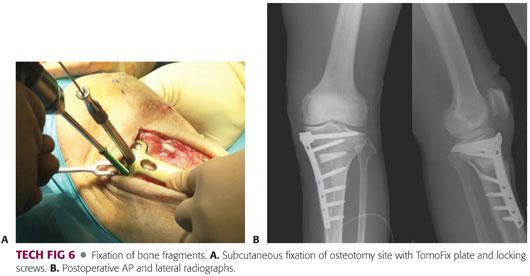
The periosteum is sutured as it was before separation and TomoFix plate (Synthes, Paoli, PA) with a locking mechanism is placed over the periosteum. Both the distal and the proximal fragment are fixed with screws (TECH FIG 6A,B). About 2 cm of additional incision above the distal end of the plate is often necessary for the distal screw fixation.
A medium Hemovac drain is placed in the osteotomized site and the subcutaneous tissue and the operative wound are closed in the standard fashion. A sterile dressing is applied. Knee immobilizers are not necessary.
 Application of Opening Wedge High Tibial Osteotomy to Another Pathologic Conditions of the Knee
Application of Opening Wedge High Tibial Osteotomy to Another Pathologic Conditions of the Knee
Dual Osteotomy for the Medial Compartmental Knee Osteoarthritis Associated with Patellofemoral Osteoarthritis
Combined medial OW-HTO and tibial tuberosity anteromedialization osteotomies
Approach
A midline longitudinal skin incision is made starting at the superior pole of the patella and ending nearly 5 cm distal to the tibial tuberosity.
Subcutaneous tissue is retracted medially and the medial retinaculum is released at the medial border of the patellar ligament. Distally, the incision is extended along with medial border of the tibial tuberosity and the medial collateral ligament and pes anserinus are subcutaneously elevated.
The lateral retinaculum is sharply dissected to release completely from the patella to the level of the vastus lateralis.
Osteotomy
The first osteotomy is a medial opening wedge oblique osteotomy, leaving the tibial tuberosity intact. Starting posterior to the patellar tendon insertion, an osteotomy of the proximal tuberosity is performed parallel to the anterior tibial cortex.
The second osteotomy is made as a tibial tuberosity anteromedialization after completing the opening wedge technique. An osteotomy is performed extending to 4 to 5 cm distal from the patellar ligament insertion with 8- to 10-mm thickness at proximal site. The distal end is incompletely cut with intact periosteum.
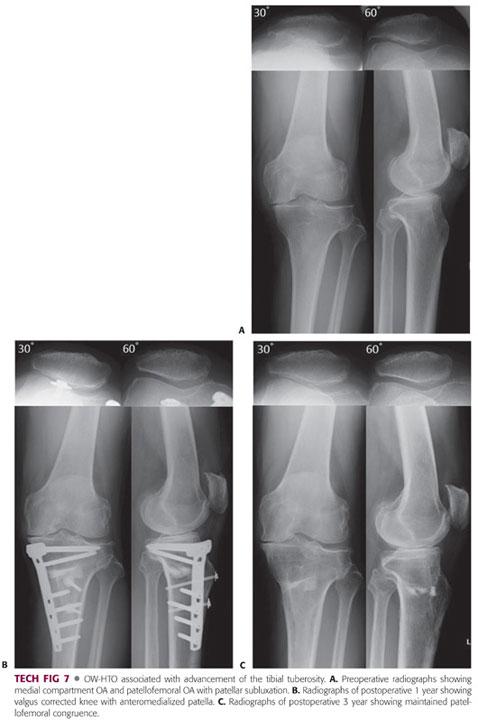
Bone Grafting and Osteosynthesis
The proximal part of the tibial tuberosity is transferred medially on its periosteal distal hinge. The distance of medialization depends on the extent of patellar subluxation. The proximal part is then elevated 10 mm anteriorly and the wedged-shaped artificial bone substitute with two holes for screws is placed under the partly detached bony fragment of the tibial tuberosity. Finally, the bony fragment is fixed with two 4.5-mm cannulated cortical screws (TECH FIG 7).
Opening Wedge High Tibial Osteotomy Associated with Mosaicplasty for Osteonecrosis of the Knee with a Large Cartilage Defect
Approach
In addition to skin incision for simple OW-HTO, a medial parapatellar skin incision is extended to the proximal pole of the patella.
Articular surface is exposed through subvastus arthrotomy.
Donor Harvest
The commonly used donor sites are the areas with less weight bearing, including the medial and lateral margins of the femoral trochlea.
Several small cylindrical osteochondral plugs of 20 mm depth are manually harvested using tubular chisels.
Graft Insertion
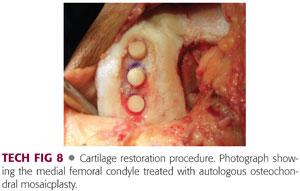
Remnants of residual cartilage and subchondral lesion are removed from the defect.
With the knee flexed, the recipient holes perpendicular to the articular surface are created using a drill.
A press-fit transplantation of the donor osteochondral plugs is performed. All plugs should be placed at the same level of the healthy cartilage (TECH FIG 8).
PEARLS AND PITFALLS | |
Exposure and dissection |
|
| |
| |
Osteotomy |
|
| |
| |
Opening gap |
|
| |
| |
| |
Plate fixation |
|
| |
| |
| |
POSTOPERATIVE CARE
 In immediate postoperative care, patients receive a femoral nerve block set at anesthesia with a patient-controlled ropivacaine injection for the first night.
In immediate postoperative care, patients receive a femoral nerve block set at anesthesia with a patient-controlled ropivacaine injection for the first night.
 After removal of the catheter, NSAIDs are used for pain control.
After removal of the catheter, NSAIDs are used for pain control.
 Sequential compression devices including foot pump (A-V Impulse System, Covidien, Mansfield, MA) are used during hospitalization to reduce the risk of deep venous thrombosis.
Sequential compression devices including foot pump (A-V Impulse System, Covidien, Mansfield, MA) are used during hospitalization to reduce the risk of deep venous thrombosis.
 The drain is removed within 48 hours postoperatively and active ROM exercise is started the day after the operation.
The drain is removed within 48 hours postoperatively and active ROM exercise is started the day after the operation.
 Straight-leg raising and setting exercises are allowed, and full knee extension is observed.
Straight-leg raising and setting exercises are allowed, and full knee extension is observed.
 Patients can walk non–weight bearing using crutches and partial weight bearing is allowed 1 week after the operation.
Patients can walk non–weight bearing using crutches and partial weight bearing is allowed 1 week after the operation.
 Walking exercise with full weight bearing using a T-cane starts 1 week after surgery.
Walking exercise with full weight bearing using a T-cane starts 1 week after surgery.
 Patients are allowed to be discharged from the hospital when they achieve the rehabilitation level of walking up and down stairs.
Patients are allowed to be discharged from the hospital when they achieve the rehabilitation level of walking up and down stairs.
OUTCOMES
 Many studies reported that HTO provided a good functional outcome for knee OA and postoperative clinical results were satisfactorily maintained for a long-term follow-up period, especially in cases with adequate postoperative limb alignment.20
Many studies reported that HTO provided a good functional outcome for knee OA and postoperative clinical results were satisfactorily maintained for a long-term follow-up period, especially in cases with adequate postoperative limb alignment.20
 Correction of the varus deformity reduces synovial inflammation and induces regeneration in the involved articular cartilage following HTO.
Correction of the varus deformity reduces synovial inflammation and induces regeneration in the involved articular cartilage following HTO.
 However, HTO has several potential disadvantages, such as limited patient selection, technical difficulty, short longevity (5 to 7 years),1,24 and possibility of neurovascular injury.
However, HTO has several potential disadvantages, such as limited patient selection, technical difficulty, short longevity (5 to 7 years),1,24 and possibility of neurovascular injury.
 Recently, OW-HTO has become more popular because of its surgical simplicity, intraoperative fine-tuning of correction, quick and safe exposure of the bone without any muscle attachment, and no risk for peroneal nerve palsy.
Recently, OW-HTO has become more popular because of its surgical simplicity, intraoperative fine-tuning of correction, quick and safe exposure of the bone without any muscle attachment, and no risk for peroneal nerve palsy.
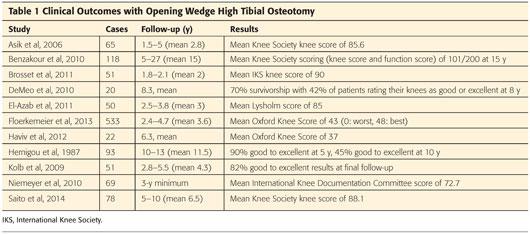
 Previous studies on OW-HTO have demonstrated promising clinical and functional short-term and midterm results (Table 1).3–6,8,9,11,13–15,19,21
Previous studies on OW-HTO have demonstrated promising clinical and functional short-term and midterm results (Table 1).3–6,8,9,11,13–15,19,21
COMPLICATIONS
 HTO is considered to be a technically demanding surgery; its complication rates are relatively high and vary depending on the experience of the surgeon, surgical procedures, and postoperative management.
HTO is considered to be a technically demanding surgery; its complication rates are relatively high and vary depending on the experience of the surgeon, surgical procedures, and postoperative management.
Intraoperative Complications
 Malalignment
Malalignment
Undercorrection or overcorrection causes unsatisfactory postoperative clinical and functional outcomes.
 Fracture of the medial or lateral cortex
Fracture of the medial or lateral cortex
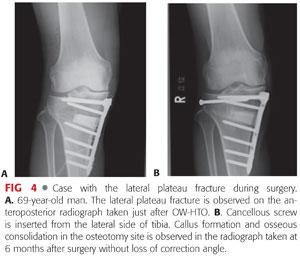
A high incidence of lateral hinge fracture was reported in OW-HTO (FIG 4).23
 Unexpected increase of the tibial posterior slope in OW-HTO
Unexpected increase of the tibial posterior slope in OW-HTO
 Unexpected intra-articular protrusion of the screw
Unexpected intra-articular protrusion of the screw
 Peroneal nerve palsy or blood vessel injury in CW-HTO
Peroneal nerve palsy or blood vessel injury in CW-HTO
Rates were reported to be between 2% and 16% for paresis of the peroneal nerve and 0.4% in vessel injury.10,12
Immediate Postoperative Complications
 Hematoma
Hematoma
 Early infection
Early infection
In a systematic literature review, superficial infections occurred in 1% to 9% and deep infections in 0.5% to 4.7%.2,16
 Compartment syndrome
Compartment syndrome
 Venous thromboembolism
Venous thromboembolism
Reports of venous thromboembolism after HTO are quite limited. The rate of deep vein thrombosis was 12.5% and that of asymptomatic pulmonary embolism was 9.4% with the use of a tourniquet in our recent study.
Late Postoperative Complications
 Patella baja
Patella baja
 Pseudarthrosis
Pseudarthrosis
The rate of pseudarthrosis is reported to be between 0.7% and 4.4%.22
 Implant failure
Implant failure
 Correction loss and recurrence of varus deformity
Correction loss and recurrence of varus deformity
REFERENCES
1. Aglietti P, Buzzi R, Vena LM, et al. High tibial valgus osteotomy for medial gonarthrosis: a 10- to 21-year study. J Knee Surg 2003;16:21–26.
2. Anagnostakos K, Mosser P, Kohn D. Infections after high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc 2013;21:161–169.
3. Asik M, Sen C, Kilic B, et al. High tibial osteotomy with Puddu plate for the treatment of varus gonarthrosis. Knee Surg Sports Traumatol Arthrosc 2006;14:948–954.
4. Bauer GC, Insall J, and Koshino T. Tibial osteotomy in gonarthrosis (osteo-arthritis of the knee). J Bone Joint Surg Am 1969;51:1545–1563.
5. Benzakour T, Hefti A, Lemseffer M, et al. High tibial osteotomy for medial osteoarthritis of the knee: 15 years follow-up. Int Orthop 2010;34:209–215.
6. Brosset T, Pasquier G, Migaud H, et al. Opening wedge high tibial osteotomy performed without filling the defect but with locking plate fixation (TomoFix) and early weight-bearing: prospective evaluation of bone union, precision and maintenance of correction in 51 cases. Orthop Traumatol Surg Res 2011;97:705–711.
7. Cass JR, Bryan RS. High tibial osteotomy. Clin Orthop Relat Res 1988;230:196–199.
8. DeMeo PJ, Johnson EM, Chiang PP, et al. Midterm follow-up of opening-wedge high tibial osteotomy. Am J Sports Med 2010;38:2077–2084.
9. El-Azab HM, Morgenstern M, Ahrens P, et al. Limb alignment after open-wedge high tibial osteotomy and its effect on the clinical outcome. Orthopedics 2011;34:e622–e628.
10. Flierl S, Sabo D, Hornig K, et al. Open wedge high tibial osteotomy using fractioned drill osteotomy: a surgical modification that lowers the complication rate. Knee Surg Sports Traumatol Arthrosc 1996;4:149–153.
11. Floerkemeier S, Staubli AE, Schroeter S, et al. Outcome after high tibial open-wedge osteotomy: a retrospective evaluation of 533 patients. Knee Surg Sports Traumatol Arthrosc 2013;21:170–180.
12. Georgoulis AD, Makris CA, Papgeorgiou CD, et al. Nerve and vessel injuries during high tibial osteotomy combined with distal fibular osteotomy: a clinically relevant anatomic study. Knee Surg Sports Traumatol Arthrosc 1999;7:15–19.
13. Haviv B, Bronak S, Thein R, et al. Mid-term outcome of opening-wedge high tibial osteotomy for varus arthritic knees. Orthopedics 2012;35:e192–e196.
14. Hernigou P, Medevielle D, Debeyre J, et al. Proximal tibial osteotomy for osteoarthritis with varus deformity. A ten to thirteen-year follow-up study. J Bone Joint Surg Am 1987;69:332–354.
15. Kolb W, Guhlmann H, Windish C, et al. Opening-wedge high tibial osteotomy with a locked low-profile plate. J Bone Joint Surg Am 2009;91:2581–2588.
16. Koshino T. The treatment of spontaneous osteonecrosis of the knee by high tibial osteotomy with and without bone grafting or drilling of the lesion. J Bone Joint Surg Am 1982;64(1):47–58.
17. Marti RK, Verhagen RA, Kerkhoffs GM, et al. Proximal tibial varus osteotomy. Indications, technique, and five to twenty-one-year results. J Bone Joint Surg Am 2001;83-A:164–170.
18. Matthews LS, Goldstein SA, Malvitz TA, et al. Proximal tibial osteotomy. Factors that influence the duration of satisfactory function. Clin Orthop Relat Res 1988;229:193–200.
19. Niemeyer P, Schmal H, Hauschild O, et al. Open-wedge osteotomy using an internal plate fixator in patients with medial-compartment gonarthritis and varus malalignment: 3-year results with regard to preoperative arthroscopic and radiographic findings. Arthroscopy 2010;26:1607–1616.
20. Odenbring S, Egund N, Hagstedt B, et al. Ten-year results of tibial osteotomy for medial gonoarthrosis: the influence of overcorrection. Arch Orthop Trauma Surg 1991;110:103–108.
21. Saito T, Kumagai K, Akamatsu Y, et al. Five- to ten-year outcome following medial opening-wedge high tibial osteotomy with rigid plate fixation in combination with an artificial bone substitute. Bone Joint J 2014;96-B:339–344.
22. Spahn G. Complications in high tibial (medial opening wedge) osteotomy. Arch Orthop Trauma Surg 2003;124:649–653.
23. Takeuchi R, Ishikawa H, Kumagai K, et al. Fractures around the lateral cortical hinge after a medial opening-wedge high tibial osteotomy: a new classification of lateral hinge fracture. Arthroscopy 2012;28:85–94.
24. Yasuda K, Majima T, Tsuchida T, et al. A ten- to 15-year follow-up observation of high tibial osteotomy in medial compartment osteoarthritis. Clin Orthop Relat Res 1992;282:186–195.
25. Zhang W, Moskowitz RW, Nuki G, et al. OARSI recommendations for the management of hip and knee osteoarthritis, Part II:OARSI evidence-based, expert consensus guidelines. Osteoarthritis Cartilage 2008;16:137–162.
< div class='tao-gold-member'>

















