Fig. 59.1
Folliculotropic mycosis fungoides. Intensely pruriginous, dusky erythematous, tumid, alopecic plaques, over the forehead, eyebrows, and eyelids in a 78-year-old man

Fig. 59.2
Folliculotropic mycosis fungoides. Infiltrated alopecic plaques on the scalp represent a usual finding in follicular mycosis fungoides

Fig. 59.3
Folliculotropic mycosis fungoides. Subtle widespread acne-like lesions, milium-like cysts, and follicular pustules on the trunk and extremities

Fig. 59.4
Folliculotropic mycosis fungoides. Follicular papules, pustules, and alopecic plaques are evident on the upper arms
Pathology
As early lesions may not display diagnostic features, biopsies may be misinterpreted as inflammatory processes like folliculitis, eosinophilic folliculitis, rosacea, lichen planopilaris, and lupus erythematosus. Multiple biopsy specimens and a high index of clinical suspicion are required to make a definitive diagnosis. Well-established lesions show a dense perifollicular lymphocytic infiltrate with prominent folliculotropism (Figs. 59.5 and 59.6). The epidermis and interfollicular dermis are usually spared. However, minimal epidermotropism can be revealed in serial sections. Rare cases may also show various degree of syringotropism (Fig. 59.5). The infiltrate is composed mainly of atypical lymphocytes with cerebriform nuclei accompanied by plasma cells, eosinophils, and histiocytes. Follicular epithelium may contain variable amounts of mucin. There may be alteration of the follicle (Fig. 59.7), resulting in comedonal changes or keratin plugging. A granulomatous inflammation may sometimes be evident due to follicular rupture and destruction. Large cell transformation may be seen in some cases.
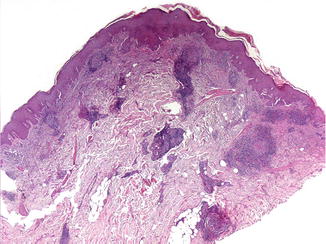
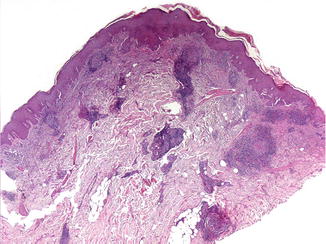
Fig. 59.5




Folliculotropic mycosis fungoides. This biopsy taken from a facial alopecic tumid plaque shows a striking adnexocentric infiltrate involving both follicular and eccrine epithelium without evident epidermotropism
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








