Fig. 7.1
Bizarre forearm synostosis in a patient with Holt-Oram syndrome
Fanconi anemia is the most common inherited cause of bone marrow failure [20]. The bone marrow failure most commonly occurs between the ages of 5 and 15. Phenotypic variations are common in presentation and include short stature, thumb and radius deformities, hyperpigmentation of skin, renal, cardiac, and genitourinary abnormalities [21]. The diagnosis can be made using a chromosome breakage analysis (diepoxybutane analysis). The test is expensive and its use as a routine screening tool in patients with apparent isolated RLD continues to be debated. However, the advent of successful pediatric bone marrow transplantation has led some authors to feel that diepoxybutane testing is important in every child with an RLD diagnosis.
Unique to many other conditions treated by the discipline of hand surgery, RLD often offers the hand surgeon the opportunity to be the first to make a diagnosis of other associated anomalies. This is related to the fact that the visible difference in upper extremity development often implores the parents and pediatrician to pursue evaluation for treatment of the affected limb. Hence, it is imperative that the hand surgeon be aware of these common associations and performs a complete evaluation of the child in all cases. This evaluation should include, at a minimum, a complete musculoskeletal and systemic evaluation, a complete blood count, echocardiogram, abdominal ultrasound, and subsequent evaluation for scoliosis.
Classification
The original classification of RLD was described by Bayne and Klug in 1987 [22]. They based the classification system on the radiographic appearance of the radius and divided the phenotype into four categories. Type I was defined as a short radius with delayed appearance of the distal radial epiphysis. Type II was defined as a “radius in miniature” with growth of both proximal and distal radial epiphyses affected. Type III denoted partial absence of the radius with no distal radial physis; Type IV was defined as complete absence of the radius.
The original classification of scheme of Bayne and Klug was modified by James et al. [23] in 1999 to include Types N and 0 with further delineation of what constituted Type I RLD. The classification was further modified by Goldfarb et al. [24] in 2005 to include more severe proximal manifestations of RLD as Type V. The current state of RLD classification is as follows (Fig. 7.2):
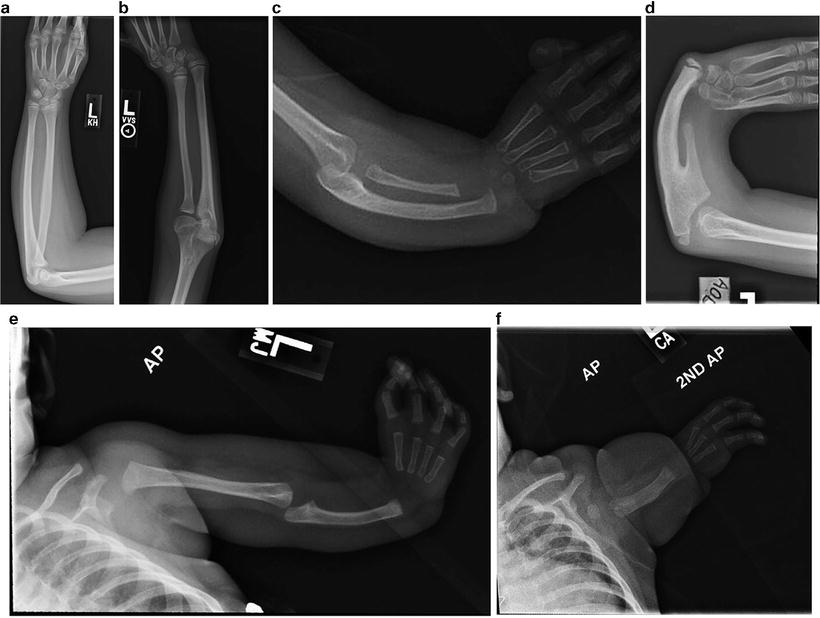
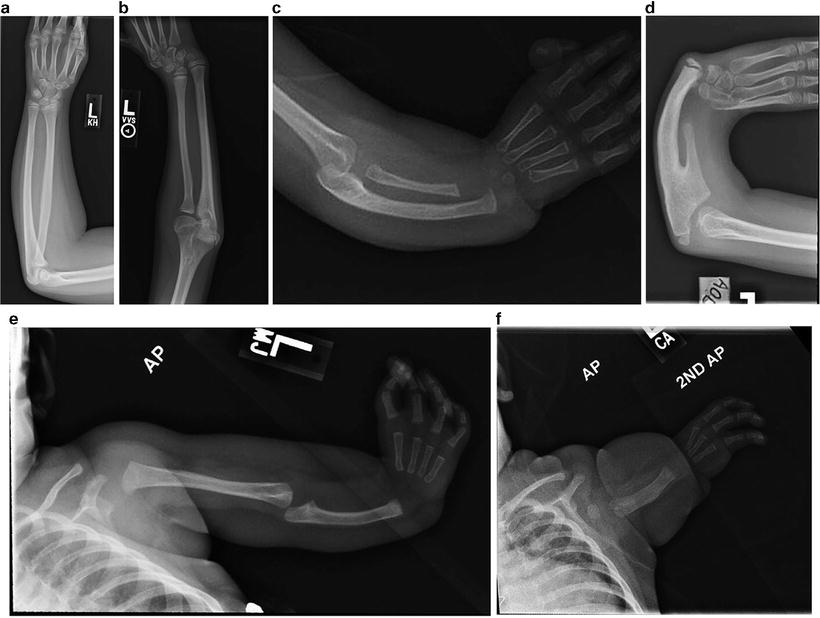
Fig. 7.2
(a) Type 0/N. (b) Type I. (c) Type II. (d) Type III. (e) Type IV. (f) Type V
Type N—The thumb is hypoplastic or absent in the presence of a normal carpus or radius. Radial angulation at the wrist is usually absent or minimal.
Type 0—The radius is of normal length with proximal and distal physes. The radial carpal bones are hypoplastic or absent. The degree of radial angulation of the wrist is variable. The angulatory deformity is owing to the abnormal carpal bones and the presence of tight soft tissue structures on the radial side of the wrist, including the wrist capsule and musculotendinous structures.
Type I—The radius is foreshortened by at least 2 mm compared to the distal ulna. The distal radial physis is present but its growth is slowed. The proximal radial physis is present and of normal morphology. Radio-ulnar synostosis or congenital radial head dislocation is variably present.
Type II—The radius is hypoplastic in its entirety with proximal and distal physes present—the so-called radius in miniature. This can be associated with notable ulnar bowing.
Type III—The distal portion of the radius is absent. There is no distal radial physis.
Type IV—The radius is absent in its entirety. This is the most common phenotypic presentation of RLD [22].
Type V—This represents a severe proximal form of RLD formerly considered phocomelia. Taking into account principles of developmental biology, the concept of a true intercalary defect has been challenged by recent authors [24, 25]. Extremities in this category have an abnormal glenoid, absence of the proximal portion of the humerus, articulation of the distal humerus with the ulna, and radial sided hand abnormalities.
Clinical Presentation
While the etiology of the condition hinges on the longitudinal dysplasia of the radius, the clinical presentation of patients with radial longitudinal dysplasia is diverse. Patients can often present with skeletal abnormalities that extend beyond the radial deficiency. These include shortening of the forearm and/or bowing of the ulna, absent or limited elbow flexion, and absence or hypoplasia of the scaphoid and other carpal bones. Thumb hypoplasia can be present and consist of hypoplasia of the thenar intrinsic and/or extrinsic musculature, hypoplasia of the skeletal elements with or without associated articular instability, rudimentary presence of the thumb (“pouce floutant”), or complete absence of the thumb. The fingers can exhibit limited flexion, with the radial digits more affected than the ulnar digits. In addition to the manifestations of RLD in the hand, the soft tissues on the radial side of the wrist and forearm are tight contributing to the radial angulation of the hand plate on the distal ulna. The extrinsic wrist extensors are often poorly developed, and the malformed radial soft tissues often form a fibrous tether to the radial side of the wrist. This combination results in the classic presentation of a radial deviated wrist held in a flexed posture.
The abnormalities have both aesthetic and functional consequences. In severe cases the appearance of the extremity can be unsightly secondary to the shortened forearm and the angled, flexed posture of the wrist and hand. On average, the forearm length is 54 % of normal, ranging from 37 to 67 % [26]. This limits the extremity’s reach and can make two-handed activities with the normal, opposite extremity difficult. In patients with bilateral upper extremity involvement, the functional limitations can be more severe. James et al. [23] found the incidence of bilateral involvement to be 65 % in a study of 104 patients. If poorly functioning digits are present, this can further impede function. Unfortunately, when present, finger dysfunction is rarely amenable to surgical correction. This is in contradistinction to thumb limitations, where several options are available to improve function.
Non-operative Management
The non-operative care of a child with RLD often begins very early in life. Occupational therapy intervention is commonly instituted during the first few weeks of life, especially if the infant requires hospitalization for associated abnormalities. Those children whose health allows them to be discharged from hospital care in the first few days of life are often referred for outpatient therapy services very early on by their pediatricians.
Therapeutic intervention at this point includes stretching exercises aimed at lengthening the contracted tissues on the radial side of the wrist and improving the hand-forearm angle. Splinting is often used as an adjunct to stretching in an effort to maintain the wrist in the corrected position and provide static resistance to a resting position of radial deviation. Specific therapeutic protocols for treatment of RLD by non-operative means vary widely from surgeon to surgeon and therapist to therapist. There have been no published reports of therapeutic regimens proven to change the natural history of RLD, although its effectiveness in teaching children to use the affected limb in an efficient and useful manner has been seen clinically by many who care for these patients. Timing of intervention is also a topic of debate among those who treat these children. The authors feel that an early stretching regimen with nap and night splinting can be instituted early in life, but the parents should be encouraged to remove the splints for extended periods while the child is awake to allow him/her to interact appropriately with his/her surroundings and obtain the sensory interaction with the environment that is essential for proper development. Two-handed activities generally begin around the age of 3 months. At this time, splint wear during awake hours may become beneficial to place the hand in a less radially deviated position, functionally increasing the length of the affected extremity, and allowing for easier two-handed manipulation of objects.
Operative Management
There have been many procedures described for the management of the wrist and forearm deformity in RLD. Since the original description of centralization by Sayre in 1894, several authors have published similar techniques with slight variations to the original procedure [27–30]. In addition, newer techniques such as radialization, pre-centralization distraction, and microsurgical transfer of vascularized epiphyses have been introduced to treat the deformity [31–34]. No single procedure has proven superior to another. Hence there remains vast disparity in treatment recommendations between surgeons treating the condition. Recurrence of the radial angulation remains the Achilles heel for procedures aimed at correcting the deformity [35].
Reports centered on treatment of Types 0, N, I, and II RLD are sparse.
Type 0
Despite the relative frequency of Type 0 RLD reported by James et al. [23], a small number of these patients require surgical intervention. In 2004, Mo and Manske [36] reported on six wrists in five children treated with surgical correction. They recommended surgical intervention for radial deviation deformity greater than 20°. In their subset of patients, the preoperative hand-forearm angle ranged from 35° to 70° with all wrists lacking active extension to neutral. The authors describe a dorsal approach to the wrist with exposure of the extensor carpi radialis tendon or tendons. The tendon is released from its distal insertion. Following release, the dorsal–radial wrist capsule, as well as the volar wrist capsule, is released allowing passive correction of the wrist to neutral position. The extensor carpi ulnaris tendon is released, leaving a distal stump for tenoraphy with the radial wrist extensors, effectively removing the radial deviation force and realigning it to gain neutral wrist extension. The proximal stump of the extensor carpi ulnaris tendon is sewn into the dorsal wrist capsule overlying the third metacarpal to further augment active wrist extension. Optionally, a pin can be placed across the carpus into the distal ulna to maintain the wrist in its corrected position. The patient is then casted in neutral to slight wrist extension for 6–8 weeks. The cast and pin, if present, are removed and the patient is allowed to begin active range-of-motion exercises. At rest the patient is splinted in the corrected position for an extended duration.
Mo and Manske [36] reported favorable outcomes using the above surgical technique. They reported an average improvement of radial deviation at rest from 58° to 12°, with active wrist extension improving an average of 53° and passive wrist extension improving and average of 28°. The average length of follow-up was 19 months (range, 2–38 months).
Types I and II
There have been few published reports on the treatment of Types I and II radial longitudinal deficiencies. Often, children with these types of RLD do not require surgical intervention. When necessary, the most common form of treatment is radial lengthening with release of the tight radial soft tissues and tendon transfer to support the realigned position. Lengthening of the radius is most commonly done by way of osteotomy and lengthening through an external fixator [37–40]. Others have reported on lengthening of the radius acutely, with gains of up to 1.6 cm [41]. Many authors have described techniques of lengthening through an external fixator with slight variations. Depending on surgeon preference, the lengthening can be performed with a single plane fixator [38] or by using a ring-type fixator [40]. When performing acute radius lengthening, Waters et al. [41] described a technique of using a temporary external fixator intraoperatively for distraction of the radius after performing a Z-cut osteotomy, followed by plate fixation of the bone in its new lengthened position.
Matsuno et al. [38] reported on two patients with Type II RLD who underwent radial lengthening with an external fixator. The outcomes demonstrated recurrence of the deformity following fixator removal with and increase the hand-forearm angle at final follow-up.
Types III and IV
The treatment of Types III and IV RLD is classically described as centralization of the carpus on the distal end of the ulna. Since Sayre first described the original procedure of centralization in 1894, multiple authors have published their experience using this technique, as well as several modifications to the procedure aimed at decreasing the recurrence of the radial angulation deformity. In addition, many others have suggested alternative procedures to accomplish the task of neutralizing the carpus on the end of the forearm. These procedures include radialization of the carpus, transfer of vascularized epiphyses to support the radial side of the carpus, and ulnocarpal fusion [31, 34, 42, 43].
Centralization
The centralization procedure is based on four surgical steps: (1) initial stretching of soft tissues ± pre-centralization distraction, (2) surgical alignment of the carpus on the ulna, (3) balancing of the deforming forces, and (4) maintenance of the corrected position.
Historically, stretching of the radial tissues was accomplished by serial cast application prior to surgical centralization, often carried out within the first several months of life. This technique fails to adequately distract the tight radial soft tissues or translate the carpus distally over the end of the ulna; instead it simply aligns the carpus alongside the distal ulna. In addition, the early application of casts precludes the use of the extremity by the child during the formative time of “learning” single and two-handed object manipulation. As a result, the use of external fixation to accomplish soft tissue distraction has been advocated in recent years by some surgeons. The application of uniplanar [44], biplanar [32, 45], and ring [33, 46, 47] external fixators have been described. The use of external fixation allows for the correction of the radial deviation deformity through distraction of the radial soft tissues and correction of the volar subluxation of the carpus in relation to the distal ulna. Distraction of the deformity is begun 3–5 days following the application of the fixator. The distraction is carried out at a rate of 0.5–1 mm per day until the desired position of the carpus is accomplished. The extremity is then maintained in the fixator for a period of 3 to 4 weeks prior to surgical stabilization of the carpus in its centralized position to allow the soft tissues to equilibrate.
Originally, the centralization procedure was performed through a longitudinal dorsal incision. Since that time, there have been multiple incisional techniques described to accomplish surgical centralization of the carpus [27, 28, 48]. The pre-centralization distraction of the soft tissues allows for ease in accomplishing surgical centralization while often obviating the need for transposition flaps for soft tissue coverage. Regardless of the incision used, the hypoplastic extensor tendons are carefully identified and retracted. The tight dorsal, radial, and volar wrist capsule and soft tissues are released to allow for a tension-free placement of the carpus onto the distal ulna aligned on the axis of the third metacarpal. Buck-Gramcko described “radialization” of the carpus in which he aligned the carpus on the axis of the second metacarpal in an effort to decrease the tendency towards recurrence of the deformity [31]. With the use of preoperative distraction, the need for “notching” [49] of the carpus to decrease soft tissue tension is usually unnecessary. The importance of obtaining a tension-free centralization has been reinforced by Sestero and Van Heest [50], who demonstrated that ulna in non-centralized radial longitudinal deficient extremities attained 64 % of normal length while the ulnar length in centralized extremities was 58 % of normal compared to 48 % of normal when notching of the carpus was performed. They postulated that the decrease in longitudinal growth capacity of the ulna was secondary to increased pressure applied to the distal ulnar physis by the centralized carpus. Once an appropriate centralized position is obtained, carpus is pinned to the ulna with longitudinal Kirschner wires (K-wires) taking care to avoid the distal ulnar physis. The pins are cut beneath the skin and often remain in place for up to 6 months postoperatively to maintain the corrected position. Soft tissue rebalancing procedures are then performed to redirect the forces across the centralized carpus. The extensor carpi ulnaris tendon is advanced to improve the ulnar and dorsal vector of pull to the wrist and hand [22, 30, 31]. If present, the radial wrist extensors are transferred ulnarly to alleviate the deforming force caused by their function. The digital extensors are translated in an ulnar direction using a sling of extensor retinaculum to align them along the longitudinal axis of the ulna, hence eliminating another deforming force.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








