Table 23.1
Types of arthrogryposis as classified by Halla
1. Limb only |
(a) Classic arthrogryposis (Amyoplasia) |
(b) Distal arthrogryposis (10 types) |
2. Limb and viscera (syndromic) |
3. Limb and CNS (lethal) |
Classic arthrogryposis is also known as amyoplasia, or arthrogryposis multiplex congenital (AMC). This is a distinct form of arthrogryposis with characteristic clinical findings. Amyoplasia refers to a = no, myo = muscle, plasia = growth. In this condition, the shoulders are usually internally rotated and adducted, the elbows are extended, the wrists are flexed and ulnarly deviated, the fingers are stiff, and the thumbs are in the palm (Fig. 23.2). If there is lower extremity involvement, the hips may be dislocated, the knees are extended, and the feet often have severe equinovarus contractures. Many patients have a mid-facial hemangioma. Associated conditions can exist. In one series, 10 % of children had gastroschisis or bowel atresia [2]. In most clinical series, symmetrical involvement of the upper and lower extremities occurs. Other variations include upper extremity only, lower extremity only, or asymmetric involvement. In Hall’s original description of 135 patients with amyoplasia, all cases were sporadic; however, there was an increased prevalence in twins and it occurred more commonly in conditions that would lead to decreased intrauterine limb movement, such as a bicornuate uterus, oligohydramnios, or intrauterine crowding [3].
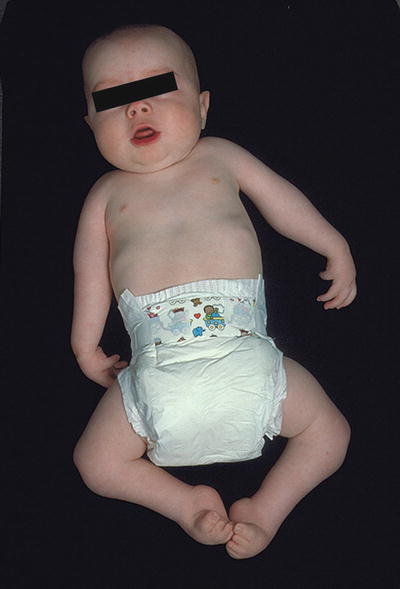
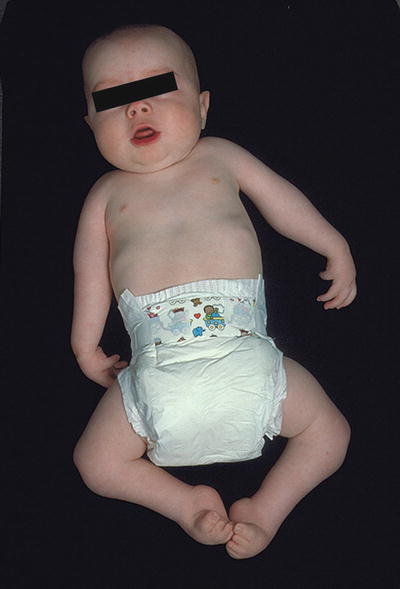
Fig. 23.2
A baby with classic arthrogryposis shows the typical features of internally rotated shoulders, extended elbows, flexed and ulnarly deviated wrists, stiff fingers, and the thumbs are in the palm. Additionally, her hips are dislocated, her knees are extended, and her feet have severe equinovarus contractures
Distal arthrogryposis includes ten distinct types as seen in Table 23.2. As described in the Online Mendelian Inheritance in Man® (OMIM®) [4], distal arthrogryposis includes what was previously called Freeman–Sheldon syndrome, Sheldon–Hall syndrome, Gordon syndrome, and multiple pterygium syndrome. Specific diagnostic criteria are necessary to make a diagnosis of a distal arthrogryposis. In the upper limb, major diagnostic criteria include camptodactyly, hypoplastic or absent flexion creases, overriding fingers, and ulnar deviation of the wrist (Fig. 23.3). This is commonly referred to as “the windblown hand.” For the lower limb, major diagnostic criteria include talipes equinovarus, calcaneovalgus deformities, congenital vertical talus, and/or metatarsus adductus. To be affected, an individual must exhibit two or more major criteria; however, when a first degree family member meets diagnostic criteria, other family members only need one major criterion to be affected.

Table 23.2
Distal arthrogryposis syndromes
Syndrome | New label | OMIMa number |
|---|---|---|
Distal arthrogryposis type 1 | DA1 | 108120 |
Distal arthrogryposis type 2A (Freeman–Sheldon syndrome) | DA2A | 193700 |
Distal arthrogryposis type 2B (Sheldon–Hall syndrome) | DA2B | 601680 |
Distal arthrogryposis type 3 (Gordon syndrome) | DA3 | 114300 |
Distal arthrogryposis type 4 (scoliosis) | DA4 | 609128 |
Distal arthrogryposis type 5 (opthalmoplegia, ptosis) | DA5 | 108145 |
Distal arthrogryposis type 6 (sensorineural hearing loss) | DA6 | 108200 |
Distal arthrogryposis type 7 (trismus pseudo-camptodactyly) | DA7 | 158300 |
Distal arthrogryposis type 8 (autosomal dominant multiple pterygium syndrome) | DA8 | 178110 |
Distal arthrogryposis type 9 (congenital contractural arachnodactyly) | DA9 | 121050 |
Distal arthrogryposis type 10 (congenital plantar contractures) | DA10 | 187370 |

Fig. 23.3
Clinical features of distal arthrogryposis are seen in this father and son. The autosomal dominant disorder shows camptodactyly in the digits, with mild ulnar deviation of the wrists. Dislocated radial heads are noted by the prominence in the lateral elbow for the son
Syndromic arthrogryposis includes multiple CNS disorders or neuromuscular diseases, which include multiple congenital contractures. Developmental abnormalities that affect the forebrain, such as microcephaly, are sometimes associated with arthrogryposis. Genetic peripheral neuropathies with an onset during fetal life are rare causes of arthrogryposis. Neuromuscular junction blockade in fetuses carried by mothers with myasthenia gravis or autoantibodies against fetal acetylcholine receptors can result in arthrogryposis [5].
Etiology
Multiple congenital contractures appear to have a final common pathway. In the normal fetus, joint formation occurs by cavitation between 26 and 52 days post-fertilization. In order for normal joint development to occur, there must be adequate space, nerve supply, and muscle activity to promote normal joint formation. A disruption in any of these elements will lead to loss of normal joint movement, causing congenital contracture [1, 5]. Restricted movement can occur through fetal crowding with multiparous births, or uterine abnormalities such as a bicornuate uterus. Maternal illness can cause restricted movement, such as myasthenia gravis. Abnormal muscle or nerve development additionally leads to congenital contractures. Oligohydramnios has a known association with multiple congenital contractures. Classic arthrogryposis (amyplasia) is not known to have a specific genetic cause.
Distal arthrogryposes are a group of autosomal dominant disorders that mainly involve the distal aspects of the limbs, characterized by primary hand and foot involvement, limited involvement of proximal joints, and variable expressivity [6]. Mutations in at least five genes (TNN12, TNNT3, TPM2, MYH3, and MYH8) that encode components of the fast twitch contractile myofibers have been associated with distal arthrogryposis [7–9]. For example, in approximately 90 % of cases of distal arthrogryposis type 2, mutations are found in MYH3, a gene that encodes embryonic myosin. Mechanisms by which altered contractility leads to congenital contracture are not known.
Syndromic arthrogryposis is commonly most severe and includes many CNS and muscular diseases [1]. CNS malformations that are associated with diminished corticospinal activation of spinal cord motor neurons, such as hydranencephaly or microcephaly, most likely contribute to fetal hypomobility and development of congenital contractures [10]. Congenital neuropathies, myopathies, and muscular dystrophies may similarly lead to multiple congenital contractures due to lack of normal fetal movement.
Historical Perspective
Adolph Wilhelm Otto first described an infant with multiple congenital contractures noted at autopsy in 1841. He described this as “a monster with inwardly curved extremities.” This has been credited as the first written description of arthrogryposis.
Clinical Manifestations of Arthrogryposis
The most common presentation to the hand surgeon includes classic arthrogryposis and distal arthrogryposis. Many children with syndromic arthrogryposis that includes limb and viscera are not surgical candidates. Patients with limb and CNS involvement have a lethal presentation as stillborn.
Classic Arthrogryposis (Amyoplasia)
Patients with classic arthrogryposis (amyoplasia) most commonly have lack of formation of normal musculature. The lack of normal muscles leads to multiple congenital joint contractures in the upper extremity. The most common pattern of deformity in the upper extremity is internal rotation of the shoulder with weak or absent shoulder girdle muscles; extension contracture of the elbow with weak or absent biceps and brachialis muscles; pronated, flexed, and ulnarly deviated wrists, with weak or absent wrist extension; and rigid digits with thumb and palm deformity. The degree of stiffness and weakness ranges from mild to severe and is not progressive.
The goal of treatment for children with arthrogryposis is to improve their quality of life by facilitating functional independence. At birth, nonoperative measures are initiated, with range of motion exercises, muscle and joint stretching, and splinting of specific joints to improve passive range of motion. Treatment to improve the function of the upper limb requires comprehensive planning with simultaneous assessment of shoulder, elbow, wrist, forearm, and hand function.
Nonoperative management is initiated at birth, and most commonly carried out for at least 12 months. Improvement of joint mobility is common, particularly at the elbow and wrist. The elbow is most critical in terms of achieving passive mobility to gain hand-to-mouth function. If after nonoperative treatment functional independence is still not possible, consideration for surgical treatment is explored [11]. Possible surgical treatment options are shown in Table 23.3.
Table 23.3
Surgical treatment options in amyoplasia
Shoulder | Derotational humeral osteotomy |
Elbow | Elbow capsular release |
Elbow tendon transfers | |
Radial head excision | |
Wrist | Dorsal carpal wedge osteotomy |
Tendon transfer | |
Digits | Syndactyly release |
Thumb | Tendon transfer |
First web release | |
Thumb adductor release |
Clinical Features of Amyoplasia
The joints of the upper and lower extremities are stiff in varying degrees. The skin is smooth over the joints, with reduced or absent skin creases. Oftentimes at large joints, particularly the shoulders, skin dimples are seen. Reduced mass of the muscles is visualized, and palpation shows an increase of firm tissue with an increase in fibrous tissue. A similarity in facial appearance is notable; intellectual development is usually normal.
Treatment of the Shoulder
In most patients, shoulder internal rotation is an integral part of their ability to perform bi-manual skills as the shoulder internal rotation helps bring their hands to midline and cross over to assist with grasp, as shown in Fig. 23.4. However, in some children, if the internal rotation contracture is severe and actually interferes with function, an external rotational osteotomy of the proximal humerus can be performed to improve function.


Fig. 23.4
De-rotation osteotomy of the shoulder can be indicated for severe internal rotation positioning of the limb causing significant dysfunction. Care must be taken with judicious use of this operation as most children with amyoplasia use the shoulder internal rotation to assist with bimanual hand use as shown in this figure
Treatment of the Elbow
Nonoperative management is initiated at birth, and most commonly carried out for at least 12 months. Improvement of joint mobility is common, particularly at the elbow and wrist. The elbow is most critical in terms of achieving passive mobility to gain hand-to-mouth function. If after nonoperative treatment elbow flexion is insufficient to allow passive mobility of hand to mouth, surgical treatment would be indicated. Specifically, if less than 90° of flexion is achieved and the hand cannot be brought to the mouth passively, a posterior elbow capsulotomy with triceps lengthening would be indicated [11]. Indications for surgery are less than 90° of passive elbow flexion and an inability to reach the hand to the mouth.
Surgical Technique
Posterior elbow capsulotomy with triceps lengthening is performed with the patient in a lateral decubitus position. A sterile tourniquet is used, at least through initial dissect to allow identification and protection of the ulnar nerve. The posterior aspect of the elbow is identified by palpation. Caution should be taken that oftentimes the limb is so internally rotated that the medial epicondyle can be mistaken for the olecranon. A curvilinear incision is made down the posterior aspect of the elbow. In arthrogryposis, significance of cutaneous tissue with minimal tissue planes is a common pathological finding. The ulnar nerve is identified as it passes through the inner muscular septum and through the cubital tunnel. Osborne’s fascia is released, and the ulnar nerve is protected with a vessel loop. The sterile tourniquet then can be removed to allow greater proximal dissection and triceps mobilization once the ulnar nerve has been identified and protected, particularly in the small child. The tricep is isolated on its insertion at the olecranon. Dissection is carried out medially and laterally, isolating the triceps tendon back to the level of the musculotendinous junction as shown in Fig. 23.5. A Z-lengthening or V-Y advancement is performed; at least doubling the length of the tendon will be necessary to provide appropriate elbow flexion.









