Temtamy classification [6]
Type A: well-formed and functioning digit on ulnar side of small finger
Type B: small nonfunctioning digit that may be pedunculated or a nubbin
Stelling classification [7]
Type 1: digit with soft tissue only
Type 2: digit with phalangeal elements
Type 3: digit with phalangeal and metacarpal elements
Buck-Gramko classification [9]
Type V rud: digit with soft tissue only
Type V distal phalanx: digit with bifid distal phalanx
“Universal” classification
Type V distal interphalangeal (DIP) joint: digit with two distal phalanges articulating at DIP joint
Type V middle phalanx: digit with bifid middle phalanx
Type V proximal interphalangeal (PIP) joint: digit with two middle phalanges articulating at PIP joint
Type V proximal phalanx: digit with bifid proximal phalanx
Type V metacarpal phalangeal (MCP) joint: digit with two proximal phalanges articulating at MCP joint
Type V metacarpal: digit with bifid metacarpal
Type V carpometacarpal (CMC) joint: digit with two metacarpals articulating with the CMC joint
Rayan classification [2]
Type I: small “wart-like” skin nubbin without a nail or bone
Type II: digit with small nail and bone with or without a joint that has no tendons and no function
Type III: digit that is more developed than type II with hypoplastic or absent PIP joint and articulation with MCP joint or bifid fifth metacarpal
Type IV: fully developed sixth digit with a sixth metacarpal
Type V: others; including ulnar polydactyly with syndactyly and other bony abnormalities
Al-Qattan classification [10]
Type I: small nubbin without bone or nail
“Modified Rayan”
Type IIA: Pedunculated non-functioning digit with narrow pedicle (<3 mm)
Type IIB: Pedunculated non-functioning digit with wider pedicle (>3 mm)
Type IIIA: Well-formed functioning digit articulating with bifid metacarpal or partially duplicated fifth metacarpal
Type IIIB: Well-formed functioning digit with proximal phalanx fused to fifth metacarpal
Type IV: digit with separate sixth metacarpal
Type V: others; including polysyndactyly and triplication of small finger
Pritsch classification [8] for Type A only
Type I: fully developed sixth metacarpal that articulates at CMC joint “metacarpal type”
Type II: digit on lateral side of fifth digit with intercalated distal metacarpal remnant “metacarpal phalangeal type”
Type III: digit from hypoplastic sixth metacarpal or fused to fifth metacarpal “phalangeal type”
Type IV: digit from metacarpal phalangeal joint “intercalated type”
Type V: digit from bifid proximal phalanx “fully developed type”
Epidemiology
Ulnar polydactyly, the most frequent congenital hand difference in African American children occurs in approximately 1 in 150 newborns [3]. Although this condition is far less common in Caucasian (1:1,400), Mexican (1:700), and Middle Eastern patients (1:1,000), it is, nonetheless, one of the most frequently encountered congenital abnormalities of the upper limb. There are several differences in associations of ulnar polydactyly in children of different racial backgrounds [10, 11].
In African American children, the condition is usually inherited in an autosomal dominant pattern and is rarely associated with other hand anomalies, congenital syndromes, or non-syndrome systemic abnormalities. The ulnar polydactyly occurring in most African American children is usually classified as Type B ulnar polydactyly. Cases are usually bilateral (70 %). The left hand is more commonly affected in unilateral cases [2, 11]. There is equal sex distribution [10, 11].
In patients of non-African decent, ulnar polydactyly is usually sporadic. Only 5 % of patients of non-African decent demonstrate a recognizable pattern of inheritance. Non-African descent patients demonstrate both Type A and Type B ulnar polydactyly. Twenty percent of cases are bilateral and males are more commonly affected than females [11]. Non-African patients also demonstrate a higher incidence of associated hand conditions including polysyndactyly, mixed polydactyly, and isolated syndactyly than do African American children. Foot involvement (i.e., lateral toe polydactyly) may also be present in some children. Cases may also be associated with other congenital syndromes [12–15]. Associated syndromes and their inheritance patterns are listed in Table 20.2. Other congenital abnormalities not associated with one of the listed syndromes are uncommon [16].
Name | Associated anomalies | Inheritance |
|---|---|---|
Ellis–van Crevald syndrome | Dwarfism, short limbs, small chest, dental abnormalities, cardiac defects | Autosomal recessive |
Smith–Lemli–Opitz syndrome | Abnormal facies, microcephaly, intellectual disability, cardiac, renal, gastrointestinal and genital malformations, hypotonia, | Autosomal recessive |
McKusick–Kaufman syndrome | Genital malformations (hydrometrocolpos), cardiac defects | Autosomal recessive |
Trisomy 13/Patau syndrome | Intellectual disability, cardiac defects, brain/spinal cord abnormalities, microophthalmia, cleft lip/palate, hypotonia | Sporadic |
Short rib-polydactyly I–III | Small chest, short limbs, cardiac defects, polycystic kidney disease, cardiac, gastrointestinal and genital abnormalities | Autosomal recessive |
Orofaciodigital syndrome | Abnormal facies, oral and dental abnormalities, cleft lip/palate, polycystic kidney disease (type I only) | Type I: X-linked dominant |
Others: autosomal recessive | ||
Bardet–Biedel syndrome | Visual loss, obesity, intellectual disability, hypogonadism, abnormal facies, cardiac, hepatic and gastrointestinal abnormalities | Autosomal recessive |
Meckel syndrome | Occipital encephalocele, other neural tube defects, polycystic kidney disease, cirrhosis | Autosomal recessive |
Greig cephalopolysyndactyly syndrome | Abnormal facies, macrocephaly, intellectual disability, large hallux/thumb | Autosomal dominant |
Pallister–Hall syndrome | Brain abnormalities (hypothalamus hamartoma), bifid epiglottis, imperforate anus, renal abnormalities | Autosomal dominant |
Weyers acrofacial dysostosis | Dental abnormalities, malformed nails, shortened limbs | Autosomal dominant |
Joubert syndrome | Brain abnormalities (molar tooth sign), hypotonia, ataxia, intellectual disability, abnormal facies, retinal dystrophy, renal, hepatic and endocrine abnormalities | Autosomal recessive, rare X-linked recessive |
Simpson-Galabi-Behmel syndrome | Abnormal facies, polythelia, diaphragmatic hernia, umbilical hernia, renal abnormalities, hepatosplenomegaly, intellectual disability, solid organ malignancy | X-linked dominant |
Hydrolethalus syndrome | Abnormal facies, cleft lip/palate, hydrocephalus, brain abnormalities, cardiac defects, airway stenosis, omphalocele | Autosomal recessive |
Acrocallosal syndrome | Macrocephaly, corpus callosum agenesis, abnormal facies, cleft lip/palate, cardiac abnormalities | Autosomal recessive |
Asphyxiating thoracic dystrophy/Jeune syndrome | Small chest, short ribs, short limbs, pelvic abnormalities, respiratory failure | Autosomal recessive |
Focal dermal hypoplasia/Goltz-Gorlin syndrome | Multiple skin abnormalities, cutaneous papillomas, ocular abnormalities, dental abnormalities, cleft lip/palate | X-linked dominant |
Isolated, non-syndrome ulnar polydactyly is also strongly associated with genetic inheritance patterns. Both autosomal dominant and autosomal recessive patterns have been described. Genetic analysis has linked ulnar polydactyly to chromosomes 7, 13, and 19 [13, 17–21]. However, the exact pattern of inheritance of ulnar polydactyly is uncertain and most likely more complex than simple Mendelian genetics [11, 22]. Environmental exposure has been suggested as posing a risk for the development of ulnar polydactyly [23].
Pathogenesis
Although ulnar polydactyly is linked to failure of differentiation of the anterior–posterior axis of the developing limb bud, the exact mechanism is unknown. Embryologic limb development occurs in a coordinated fashion along the three spatial axes in a complex series of steps that begin with limb bud formation [1]. The embryologic formation of the upper limb is detailed in elsewhere in this book (Chap. 1). As the limb bud develops and lengthens along the proximal–distal axis, the zone of polarizing activity (ZPA) is established in the posterior mesoderm. Sonic hedgehog (SHH), elaborated by the ZPA, influences digital development and identity along the anterior–posterior axis. SHH contributes to the unique formation of the ulnar-sided structures of the forearm, wrist and hand including the ulna, the two ulnar columns of the carpal bones, and the small finger, ring finger, and the ulnar half of the middle finger. Deficiency of SHH leads to ulnar ray deficiency and overexpression of SHH leads to radial polydactyly [14]. Ulnar polydactyly has been linked to the Gli-3 transcription factor, an important protein in the signaling pathway of SHH located on chromosome 7 [24]. The Gli-3 protein exists in an active form (Gli-3A) and a repressor form (Gli-3R). Gli-3A exists primarily in the posterior mesoderm and displays the same gradient as SHH with decreasing concentrations anteriorly. Gli-3R has the opposite gradient with higher concentrations in the anterior mesoderm and decreasing concentrations posteriorly. Syndromes associated with ulnar polydactyly have been associated with defects in the Gli-3 gene as well as with defective processing of the Gli-3 protein into its active form [14, 25]. The normal balance of Gli-3 is disturbed when there is a relative increase in Gli-3R compared to Gli-3A. It has been proposed that this imbalance contributes to the formation of ulnar polydactyly [14].
Anatomy
Type B ulnar polydactyly includes rudimentary supernumerary digits that arise from the ulnar border of the small finger (Fig. 20.1). Because these digits lack bony elements and tendons, they are nonfunctional. The digits may be as small as a wart-like bump on the ulnar side of the small finger proximal phalanx or may take the form of a somewhat more developed digit with a fibro-cartilaginous ossicle and a hypoplastic nail [3, 26]. The small, wart-like bumps, or rudimentary polydactyly, are considered to be remnant stumps from digits that were auto-amputated in utero [27, 28]. “Pacifier polydactyly” refers to a specific Type B polydactyly demonstrated by a very large and edematous soft tissue nubbin that is consistently sucked by the patient [29]. All Type B supernumerary digits, including rudimentary polydactyly, contain a neurovascular pedicle.
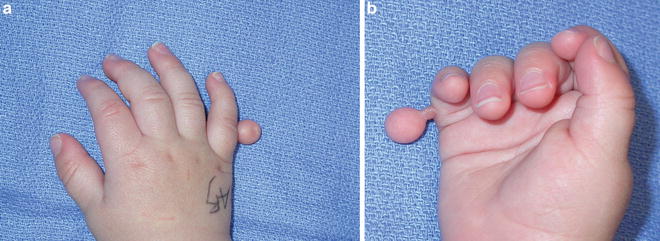
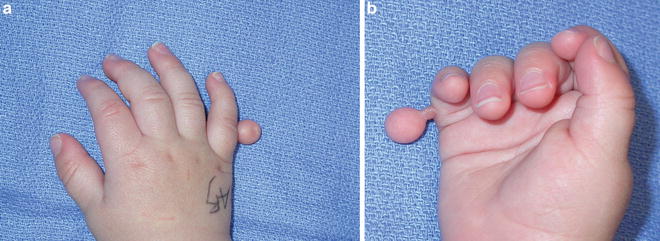
Fig. 20.1
(a) Dorsal and (b) volar views of a child with Type B ulnar polydactyly demonstrating a large pedunculated mass with a long stalk. There is a rudimentary nail present on dorsal aspect
Type A ulnar polydactyly includes more developed digits with variable anatomy (Fig. 20.2). Type A digits always contain bony elements and may contain anomalous flexor and extensor tendons including the insertion for the abductor digiti minimi (ADM) and flexor digiti minimi brevis (FDMB) muscles. The interphalangeal joints are often hypoplastic and stiff. Digits that extend to or beyond the metacarpophalangeal (MCP) joint, either with a bifid metacarpal or a duplicated proximal phalanx articulating with a common metacarpal phalangeal joint, will include the insertion for the ulnar collateral ligament of the metacarpal phalangeal joint. A sixth metacarpal may include the insertions of the opponens digiti minimi (ODM) and be surrounded by the muscle bellies of the ADM and FDMB muscles. Type A digits contain digital nerves and arteries.
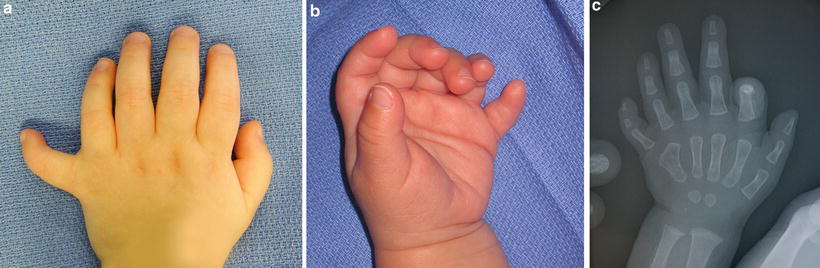
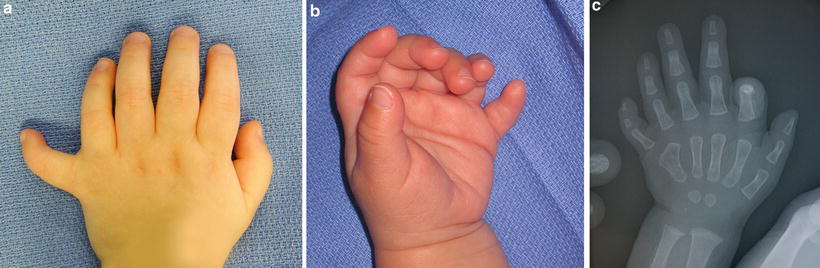
Fig. 20.2
(a) Dorsal and (b) volar views of a child with Type A ulnar polydactyly. The extra digit is fully formed with bony elements. There is some ulnar angulation of the digit compared to the adjacent small finger. (c) Hand radiographs demonstrate the proximal phalanx of the polydactylous digit is articulating with an abnormally broad metacarpophalangeal joint along the ulnar side of the joint. The joint surface is sloped ulnarly, which explains the angulation of the extra digit
Diagnosis
Ulnar polydactyly, particularly Type A, may be diagnosed prenatally during routine second trimester ultrasound [15]. Remaining cases of ulnar polydactyly usually should be diagnosed during routine postnatal physical exams. Most cases of rudimentary ulnar polydactyly may be diagnosed by careful examination of the skin on the ulnar border of the hand. The physical examination should focus on elements associated with syndromes that include ulnar polydactyly (see Table 20.2). In children with Type A ulnar polydactyly, anterior–posterior radiographs will help clarify the bony anatomy of the supernumerary digit. Family history should be obtained to determine a potential genetic causation. Referral to a geneticist should be considered in patients with evidence of congenital syndromes or isolated familial ulnar polydactyly. Referral to other pediatric specialists should precede surgical treatment of the ulnar polydactyly.
Treatment
The families of patients with Type A ulnar polydactyly are often surprised and distressed by their child’s hand difference. The treatment of ulnar polydactyly is not an emergency. Type A ulnar polydactyly with a fully formed sixth ray may be functional. The family may still opt for surgery to give the hand a more “normal” appearance. In some cultures ulnar polydactyly is seen as a supernatural trait and individuals with extra digits were often given deferential treatment [30].
Many newborns with Type B ulnar polydactyly are treated by ligation without hand surgery consultation. Small, pedunculated digits are commonly treated by suture ligation by the nursery staff, pediatricians, obstetricians, and neonatal intensivists. With time the digit becomes ischemic and falls off days to weeks after the suture is applied [3] (Fig. 20.3). Vascular clips have also been used to cause ischemia by clamping across the pedicle of the digit. It has been reported that in untreated patients, the digit may auto-amputate and fall off without intervention [2]. Newborns with more completely developed ulnar polydactyly are usually referred to a hand surgeon [31].
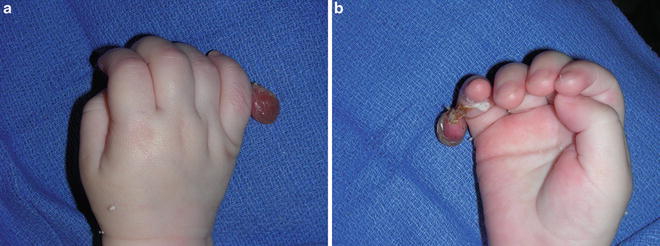
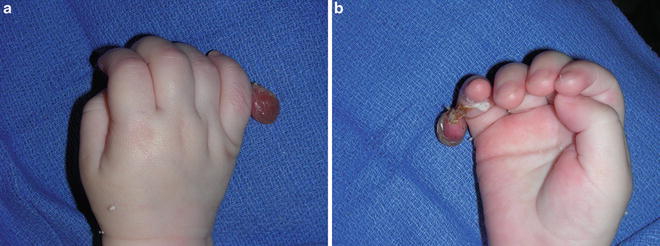
Fig. 20.3
(a) Dorsal and (b) volar views of a child treated with suture ligation of Type B ulnar polydactyly. One week after the suture was placed, the digit demonstrates significant edema and necrosis. The stalk can be seen to be separating from the ulnar aspect of the small finger. The digit subsequently fell off and the area went on to heal without complication
Open excision of Type B digits in the nursery or office is an alternative to ligation that avoids the creation of a necrotic digit. The patient is soothed with a pacifier and the hand anesthetized with local anesthesia. The area is prepped and the supernumerary digit is excised in a fusiform pattern. The base of the wound is coagulated using a battery cautery, electrocautery, or topical silver nitrate and closed using simple absorbable suture. Topical antibiotic ointment or steristrips may be applied to the area as a dressing. The area typically heals with a small scar that is rarely problematic.
Because Type A polydactyly generally requires treatment under general anesthesia, surgery is delayed until the child is 6 months old. The goal of surgery is to excise abnormal bony and soft tissue elements while preserving function of the small finger. The incision should be designed using a racquet shape around the supernumerary digit preserving as much skin as possible. The incision can be extended proximally in the mid-lateral line of the finger and hand along the junction of the glabrous and non-glabrous skin. The skin is incised and sharp and blunt dissection is used to expose the bony elements of the digit. The bony elements are isolated from the surrounding subcutaneous tissue. Anomalous flexor and extensor tendons are sharply dissected, incised, and allowed to retract into the hand. The neurovascular bundles to the extra digit are identified. Traction neurectomies are performed on the digital nerves and the arteries are cauterized using bipolar cautery. The skin flaps are trimmed to allow for a linear closure that should lie in the midlateral line. Standing cutaneous deformities “dog-ears” should be corrected extending the incision longitudinally or along flexor creases.
Ulnar polydactyly that extends to or is proximal to the fifth metacarpal phalangeal joint deserves special attention. The hypothenar muscles, including the insertion of the ODM and muscle bellies of the ADM and FDMB, should be preserved and dissected from the extra metacarpal in the subperiosteal plane. In cases where the polydactyly extends proximal to the metacarpal phalangeal joint, the ADM insertion on the extra proximal phalanx is preserved with a periosteal sleeve. The ADM insertion is transferred to the base of the radial proximal phalanx to assure small finger abduction. If the polydactyly includes two proximal phalanges articulating with the small metacarpal at the MCP joint, the insertion of the ulnar collateral ligament on the base of the extra proximal phalanx should also be preserved with a periosteal sleeve. After excision of the ulnar digit, the ulnar collateral ligament should be transferred to the base of the retained proximal phalanx. When the metacarpal is bifid, osteotomy of the metacarpal creates a more normal contour of the residual small finger metacarpal. Angulation of the metacarpal should be corrected with closing wedge osteotomies and Kirschner wire fixation. The ulnar collateral stability of the reconstructed metacarpal phalangeal joint of the small finger should be tested. If additional stability is necessary, suture capsulorrhaphy with pin fixation of the MCP joint should be considered. The extrinsic flexor and extensor tendons should be centralized if eccentric.
Complications
Treatment-related complications are surprisingly more frequent in suture ligation than in surgical excision [2]. First, unless the suture is tied exactly at the base of the pedunculated digit, where it originates from the skin of the small finger, the skin that remains that is proximal to the suture may persist as a visible and palpable bump (Fig. 20.4); this occurs in up to 40 % of patients who undergo suture ligation [2, 3]. A painful neuroma may form at the amputation site. Improvement after excision of the remainder of the bump and traction neurectomies of the nerves has been demonstrated by several studies [32–34]. This occurrence of this complication may be minimized by surgical excision of pedunculated Type B ulnar polydactyly with traction neurectomy [35]. Other complications associated with suture ligation include bleeding, infection, and necrosis without amputation [2, 33].









