Fig. 24.1
(a) Clinical photograph and (b) AP and lateral wrist radiographs of patient with Madelung deformity. Reproduced with permission from Shriners Hospitals for Children—Northern California
On physical examination, the deformity is most noticeable observing the subluxation from the ulnar side. The forearm is of normal shape. The distal end of the ulna is distinct under the skin and the styloid process and articular surface can be recognized. The hand is normal, but has dropped palmarly. The diameter of the wrist is almost twice normal. The hand, viewed from the radial side, is less obviously displaced. The extensor tendons, which pass over the radius towards the dorsum of the hand, bridge and obscure the step that is so noticeable on the ulnar side. The anteroposterior diameter of the wrist appears almost double that of the contralateral side. When the distal end of the radius is palpated with the hand dorsiflexed, and the extensor tendons relaxed, a large portion of the articular surface of the radius may be palpated. At the same time it is noticeable that the posterior lip of the distal radius, which is normally rather sharp, is more obscure. If it is compared with the radius of the healthy side, it is noticed that the whole distal epiphysis of the radius is angulated palmarly [3].
Associated Conditions/Differential Diagnosis
Leri-Weill dyschondrosteosis is a dominantly inherited skeletal dysplasia that is frequently associated with Madelung deformity. Those affected present with normal intelligence, short stature, mesomelic limb shortening, and Madelung deformity. Mesomelia is defined as when the middle portion of a limb is shortened in relation to the proximal portion and is the most frequent clinical finding in LWD [16]. In 2001, Ross et al. [17] performed a study of 43 patients with LWD and found that 32 (74 %) had Madelung deformity. Both Madelung deformity and LWD are more common in females, possibly due to the role estrogen plays in the development of dyschondrosteosis and the effect of estrogen on the physis [17, 18].
The short stature homeobox (SHOX) gene is expressed by both sex chromosomes in males and females and is thought to play a role in bone growth and development. Haploinsufficiency of the SHOX gene, which is located in the pseudo-autosomal region of the chromosomes, results in the genetic defect that causes LWD [17]. Due to recombination between sex chromosomes during meiosis, the SHOX defect is passed to offspring in a pseudo-autosomal dominant inheritance pattern instead of in a sex-linked pattern. Therefore, the offspring of a person with a SHOX haploinsufficiency disorder have a 50 % chance of acquiring the genetic mutation. Langer mesomelic dysplasia (LMD) results from a homozygous deletion or compound heterozygous mutation of SHOX. LMD may occur in offspring where both parents have LWD. It is characterized by severe skeletal dysplasia and short stature, with shortening of the long tubular bones more marked in the proximal portion of the extremity. Madelung deformity is much rarer in those with LMD than those with LWD [16].
Turner syndrome (TS) is a genetic disorder (45, XO) that is also due to haploinsufficiency of the SHOX gene and includes short stature, primary amenorrhea, neck webbing, lymphedema, high-arched palate, short metacarpals, scoliosis, hearing difficulties, cardiac and renal anomalies, hypothyroidism, and glucose intolerance [16]. Madelung deformity may be seen in up to 7 % of affected individuals. The reason for the relatively low incidence in TS versus the high incidence in LWD is not clear, but may be due to the influence of estrogen exposure on the development of Madelung deformity. Those with TS may be protected from developing Madelung deformity by their sex steroid deficiency, whereas LWD females generally have normal ovarian function [17].
Cases of Madelung deformity have also been reported in those with psuedohypoparathyroidism types 1a and 1b, due to a mutation in the GNAS gene [19, 20]. It has also been reported in the setting of nail-patella syndrome, which is inherited in an autosomal dominant fashion with variable penetrance [21]. Both of these syndromes share no known relationship with SHOX gene mutations and illustrate the complexity of the genetic origins of the deformity. Idiopathic cases may represent de novo or as uncharacterized mutations [18]. Further research is needed to identify the genetic mutations associated with this deformity.
The theory that Madelung deformity is caused by wrist trauma has been debated for decades, with argument against this cause dating as far back as Anton et al. in 1938 [22]. It is disputed that since most cases present in young females with no history or exposure to trauma, it is unlikely that this could be the reason for the deformity. However, in a more recent study, a Madelung-like deformity has been described in female gymnasts that are believed to be the result of physeal trauma due to repetitive loading of the wrist joint.
So-called reverse Madelung deformity was recognized by Kirmisson as a similar yet separate deformity in 1902. Since that time, there have been only a handful of cases reported in the literature. In the reverse Madelung deformity, the radius is bowed dorsally, displacing the distal ulna palmarly. The articular surface of the radius is angulated dorsally, shifting the carpus dorsally as well. It is unknown whether this deformity is mediated by the same genetics as true Madelung deformity, or whether it represents a separate form of skeletal dysplasia.
Diagnosis
Most patients with Madelung deformity initially present to the physician somewhere between 8 and 14 years of age [12]. The primary complaint is often that of wrist pain and stiffness, but may include difficulty with school, sports, or other activities of daily living, as well as concern over the appearance of the wrist itself [18]. Physical examination will reveal the prominent distal ulna with volar subluxation of the carpus relative to the forearm. Supination and wrist extension may be limited and there may be instability of the DRUJ depending upon the severity of the deformity. Distal hand function and elbow motion are unaffected [12]. Spontaneous rupture of extensor tendons has been reported in the literature, associated with the dorsal prominence of the distal ulna, and may lead to a diagnosis in those with longstanding disease. A comprehensive history and physical examination of the patient is essential to evaluate for associated diagnoses, such as LWD, or other unrelated causes for the patient’s complaints. In cases where LWD is suspected, younger siblings should be examined and radiographed as well, as it may be possible to intervene with less-invasive procedures prior to symptoms appearing.
Radiographs will confirm the diagnosis of Madelung deformity. Early reports on the radiographic appearance of the wrist in this disorder described features such as “pyramidalization” of the carpus as a result of the proximal subsidence of the lunate, the absence or narrowing of the ulnar aspect of the distal radial physis, anterior bowing of the radial shaft, and dorsal subluxation of the ulnar head [22]. Several radiographic parameters have been proposed to identify, quantify, and categorize Madelung deformity. Measurements were initially based on the radius [13], but this is unreliable due to the anatomic variability of the radius in this condition. More recent criteria have been based on the ulna, as it is thought to be normal. McCarroll et al. [23] identified five radiographic parameters for Madelung deformity, including ulnar tilt, lunate subsidence, lunate fossa angle, palmar tilt, and palmar carpal displacement. They found that ulnar tilt, lunate subsidence, and palmar carpal displacement are reliable and reproducible measurements for quantifying the severity of Madelung deformity on X-rays (Fig. 24.2). Measurement of palmar tilt is unreliable because of the superimposition of multiple structures on the lateral X-ray. In a later study performed by the same group, diagnostic threshold values for ulnar tilt, lunate subsidence, lunate fossa angle, and palmar carpal displacement were determined. The thresholds are defined as: an ulnar tilt of 33° or greater, lunate subsidence of 4 mm or more, lunate fossa angle of 40° or greater, and palmar carpal displacement of 20 mm or more. The lunate fossa angle was found to be especially useful in the early diagnosis of Madelung deformity [24].
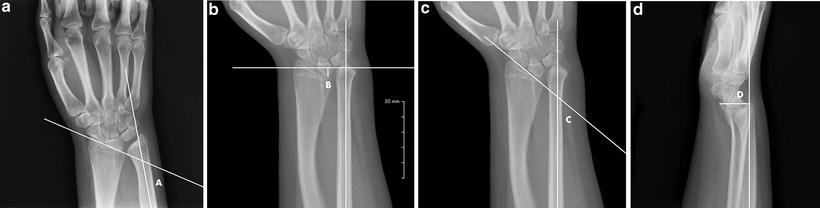
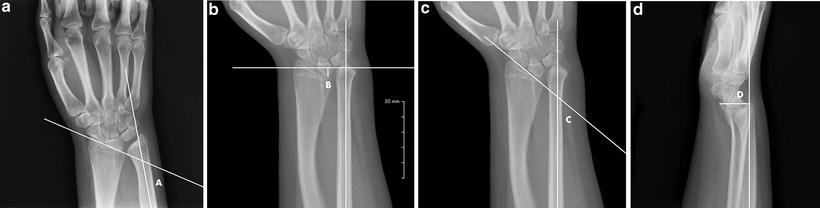
Fig. 24.2
Radiographic parameters of Madelung deformity. (a) (Ulnar tilt): Ulnar tilt is defined on the PA X-ray as the complement (90°-angle A) of the acute angle (angle A) between the longitudinal axis of the ulna and a line tangential to the proximal surfaces of the scaphoid and lunate. (b) (Lunate subsidence): Lunate subsidence on a PA X-ray is defined as the distance in millimeters (distance B) between the most proximal point of the lunate and a line perpendicular to the longitudinal axis of the ulna and through its distal articular surface. The measurement is positive if the ulna extends distal to the proximal surface of the lunate. (c) (Lunate fossa angle): Lunate fossa angle on a PA X-ray is defined as the complement (90°-angle C) of the acute angle (angle C) between the longitudinal axis of the ulna and a line across the lunate fossa of the radius. (d) (Palmar carpal displacement): Palmar carpal displacement on a lateral X-ray is defined as the distance in millimeters (distance D) between the longitudinal axis of the ulna and the most palmar point on the surface of the lunate or capitate. Reproduced with permission from Shriners Hospitals for Children—Northern California
There is little information written regarding the use of MRI in the diagnosis and evaluation of Madelung deformity. Vickers and Nielsen [13] advocate for the use of MRI in their 1992 study, suggesting that the early identification of the thickened volar radiolunate (Vickers) ligament may allow for prophylactic excision. Other studies [25, 26] have confirmed the presence of the Vickers ligament as well as an anomalous thickened volar radiotriquetral ligament. However, the clinical usefulness of MRI in Madelung deformity has not yet been evaluated critically and is not currently part of our institution’s routine workup.
Treatment Methods
Appropriate treatment of Madelung deformity remains controversial. This is in part due to the fact that many patients are very concerned with the appearance of the wrist, making it difficult to tease out other functional concerns. Patients who present simply because they notice the bony deformity do not necessarily require treatment. In our experience, however, this scenario is quite rare, and most patients present with limitations in range of motion along with pain. Nonsurgical treatment is limited to symptom relief—splinting and activity modification may help those with mild, intermittent symptoms. However, since Madelung deformity is an anatomic problem, definitive treatment is generally surgical. Surgical treatment of the Madelung deformity can be divided into three categories: early prevention, late correction, and salvage procedures. First, early deformity in young patients with open physes can be treated in a preventative manner with physiolysis and release of Vickers ligament. Second, various osteotomies of the radius and ulna have been described to correct the bony deformity in patients with limited growth remaining. Lastly, some patients may not present for treatment until adulthood, generally with complaints related to ulnocarpal impaction. In these patients, an ulnar shortening osteotomy, with or without a concomitant osteotomy of the distal radius, may be appropriate. Partial or complete wrist arthrodesis may also be considered in the setting of an arthritic joint.
Physiolysis and Vickers Ligament Release
In their 1992 study, Vickers and Nielsen [13] identified two distinct lesions that are central to the pathogenesis of Madelung deformity. The principal lesion is growth arrest in the ulnar zone of the distal radial physis, which slows the growth in this area asymmetrically resulting in volar and ulnar bowing of the distal radius. They also identified the Vickers ligament, which, as discussed previously, is an abnormally thickened short radiolunate ligament that tethers the lunate to the distal radius, leading to the classic pyramidalization of the carpus. This ligament may also contribute to the partial growth arrest of the distal radial physis secondary to compression. Vickers and Nielsen [13] recommended addressing both of these lesions through a transverse volar approach, but modifications in this approach have been made more recently to utilize a standard longitudinal volar incision [27].
This procedure is reserved for young patients with open physes and is intended to prevent further deformation of the wrist. A traditional Henry approach to the volar distal radius is utilized. The thickened Vickers ligament is identified deep to the pronator quadratus and transected, releasing the soft-tissue tether. The bony bridge on the volar-ulnar aspect of the distal radial physis is identified via a combination of preoperative imaging, intraoperative fluoroscopy, and direct visualization. This area is then curetted, with care being taken to avoid injuring the adjacent healthy physeal cartilage. Pronator muscle or fat is then interposed to replace the resected segment and to prevent physeal bar formation (this is also known as the Langenskiöld procedure). Once the soft tissues are repaired, the wrist is placed into a short-arm cast for 2 weeks (Fig. 24.3). The patient’s growth is followed closely with radiographs every 6 months. If the ulna appears to be overgrowing, epiphysiodesis should be considered [12]. The efficacy of this release is unknown. Vickers and Nielsen [13] treated 15 wrists in 11 skeletally immature patients and reported no progression of deformity.


Fig. 24.3
AP wrist radiograph before and 2 months after Vicker ligament release and physiolysis. Reproduced with permission from Shriners Hospitals for Children—Northern California
There is a paucity of additional publications on physiolysis for Madelung deformity. There are “word of mouth” reports of serious complications following the procedure, possibly secondary to loss of the support of the Vickers ligament, which is the only support for the volar aspect of the lunate. Until the usefulness of the procedure is further defined, the authors advise caution and care in its use. Also, the procedure described by Vickers and Nielson does not correct preexisting deformity, nor does it provide a solution for the more typical Madelung deformity patient who presents with marked deformity and little growth potential remaining [10, 28]. This led to the development of techniques to correct the bony deformity through a radial osteotomy, which may be performed in isolation or in combination with release of Vickers ligament. All of the recent publications describing osteotomy of the radius in patients with Madelung deformity have a common goal in preserving the DRUJ.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







