22 Procurement of Thin Flaps as Indicated in the Lower Extremity
Summary
Elevation on the superficial fascia (super-thin) is a new approach for elevating flaps. It has advantages such as providing a thin flap allowing increased versatility to achieve better contour of flap, minimizing the need for secondary debulking, and being hemodynamically reliable.
Keywords: super-thin flap, superficial fascia elevation, flap elevation
22.1 Introduction
The goals of microsurgery reconstruction are functional outcome and aesthetic result. To achieve these goals, we often need a thin flap that is pliable and viable. Perforator flaps have been extensively used for these purposes from head and neck reconstruction, trunk reconstruction, and extremity reconstruction. But often when reconstructing for coverage, the bulk of the perforator flaps makes it difficult to achieve good contour at a single stage especially in obese patients.1
The current method of elevation of the perforator flap is either subfascial where the flap is elevated with the deep muscle fascia or suprafascial where the elevation is made just above the deep fascial plane.2 In either case, the flap frequently remains too bulky to resurface the defect. Immediate debulking procedures can follow but may result in partial loss of the flap.3 Microdissection can be applied with better success to achieve a thin flap but may be to tedious and time consuming.4 Thus, secondary debulking procedures are chosen to minimize flap loss, and procedures such as liposuction or surgical resection are followed to achieve better contour of the reconstruction site. But if possible, one should aim to have the ideal reconstruction at a given single stage like the concept of the reconstructive elevator.5
In this chapter, we will focus on how to thin the flap based on a new plane, the superficial fascial plane, which may provide a constant safe and reliable plane.6 Since the anterolateral thigh (ALT) flap and the thoracodorsal artery perforator (TDAP) flap have been discussed in detail in the previous chapters, only the superficial circumflex iliac artery perforator (SCIP) flap and the gluteal artery perforator (GAP) flap will be exemplified in this chapter.7,8,9,10
22.1.1 Attributes
• There are three distinctive layers for elevation: subfascial, suprafascial, and superficial fascia.
• The superficial fascia is a distinct white film-like layer between the deep and superficial fat that is easily identifiable.
• The linking vessels may be connected in the superficial fat that stabilizes vascular reliability of the flap when elevating on this plane.
• The indirect linking vessels allow the flap to capture multiple perforasomes.
• The superficial fascia is a relatively avascular plane that allows easy dissection.
• The elevation on this plane allows for a thin skin flap harvest.
22.1.2 Detriments
• Elevation on the superficial fascia will be thick in very obese patients and may need further debulking secondarily, but far thinner than taking the whole thickness.
• When near the pedicle, one should be careful and take note of the small perforators and the branches.
• It cannot be used as a sensate flap as the nerve is usually located just above the deep fascia.
• A steep learning curve may be needed.
22.2 Anatomical Considerations
Using the superficial fascial plane in flap elevation is a different approach from the classical subfascial or suprafascial approach. The subfascial approach is made by incising the deep fascia, and then elevating beneath this fascia, which makes it easier to identify the perforators before it penetrates the fascia. It is the easiest and, maybe, fastest way to elevate the flap.2,11,12 The disadvantage, however, is that this approach leaves the thickest flap with possibility of muscle hernia. The suprafascial approach elevates the flap above the fascia until the perforator is reached and then opening the hiatus of the deep fascia and dissecting the perforator proximally toward the source vessel. Although it reduces the risk of muscle hernia by keeping the deep fascia intact, the risk of skin graft loss and depression of scar remains a problem if the donor site is not closed primarily. Finally, despite being thinner than the subfascial approach, it may still be too thick and not adequate for resurfacing defects with thin surrounding skin.6
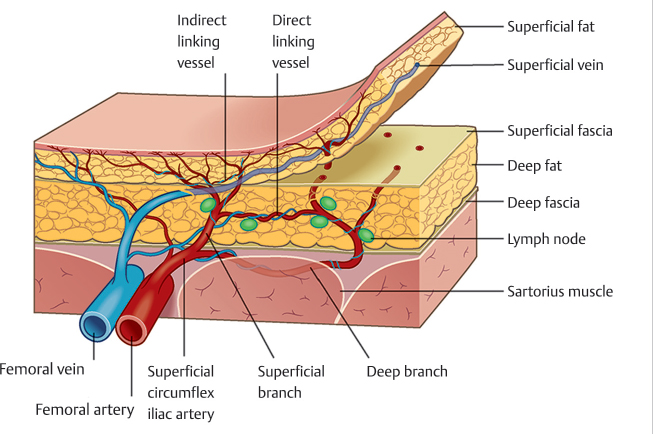
The critical anatomy when elevating the thin flap is the identification of layers: deep fascia, deep fat, superficial fat, and the superficial fascia that lies between the two fat layers (▶ Fig. 22.1).3,13,14 According to the perforasome concept by Saint-Cyr et al, viability of the flap with the superficial fascia plane will be derived from perfusion of the perforator and the ability of indirect linking vessels connecting to each other.15,16 Based on this knowledge, a large thin flap will survive even without direct linking vessels.17,18 Therefore, despite the debulking of the deep fat where the direct linking vessels might be found, the thin flap harvested on the superficial plane will still have adequate blood supply.6
The superficial fascia acts to maintain the skin integrity. Once removed, the skin can expand mimicking the full-thickness skin graft. Thus, the ability to stretch allows the flap to have thinner appearance while maintaining adequate circulation to the flap.
Another critical component of elevation on a superficial fascia plane is to identify perforators. When elevating on the superficial fascia plane, one can come across multiple perforators heading upward toward the skin. If multiple ones are identified, the perforator with the largest diameter is usually preferred. Once the perforator of choice is determined, dissection has to head toward the source vessel until an adequate length of the perforator is achieved; this is known as the freestyle approach. The final critical component of elevating on the superficial fascia can be the superficial veins. The importance of the superficial veins is known especially when elevating flaps having a potentially dominant superficial venous system. Among the commonly used flaps in the extremity, DIEP (deep inferior epigastric perforator) and SCIP flaps can be such examples. In these flaps, it is wise to include the superficial vein even when accompanying veins of the perforator allow adequate drainage.
Fig. 22.1 The critical anatomy when elevating the thin flap is the identification of layers: deep fascia, deep fat, superficial fat, and the superficial fascia that lies between the two fat layers. This illustration depicts the elevation on the superficial fascial plane.
The skin of the flap itself can vary in thickness. The only part of the skin that has a large epidermal component other than the hand and foot is the buttock skin. While the back (TDAP flap, parascapular flap) and the buttock (GAP flap) have a similar or a lightly thicker skin thickness (epidermis and dermis) compared to the plantar surface, the back skin has only half the epidermal component compared to the buttock.19 On the contrary, the skin thickness of the anterior body may be thinner. Furthermore, the SCIP flap has one of the thinnest fat deposits as the skin is relatively tightly adhered to the deep fascia compared to other sites such as the abdomen and thigh. Thus, one can consider the skin thickness when reconstructing a defect.
22.3 Anatomical Variants and Potential Pitfalls
When elevating the flap on the superficial fascia, the identification of this layer can be tricky especially in thin patients. In a thin patient, there might be lack of deep fat as well as superficial fat, making the distinction difficult. Nevertheless, adequate tension can show the superficial fascia. Adequate tension and countertension during elevation of the perforator flap is critical to identify the superficial fascia. This maneuver allows identifying the avascular thin white film-like structure with better clarity.
The elevation in freestyle allows coping with any variant of perforator location. However, pre-elevation Doppler marking will guide you to expect where and when meticulous approach is needed. The concept of hot and cold zones of the flap may come in handy when elevating any perforator flap. Rapid elevation can occur during the elevation of the cold zone where there are no meaningful perforators and meticulous dissection is required as you come close to the vicinity of the marked perforators (hot zones).
There can be multiple perforator variants derived from the ALT, TDAP, GAP, and SCIP flaps. The perforators may not originate from the commonly known named sources. However, the freestyle approach lets you overcome these variations by quickly identifying another perforator in the adjacent region and change the flap design accordingly.
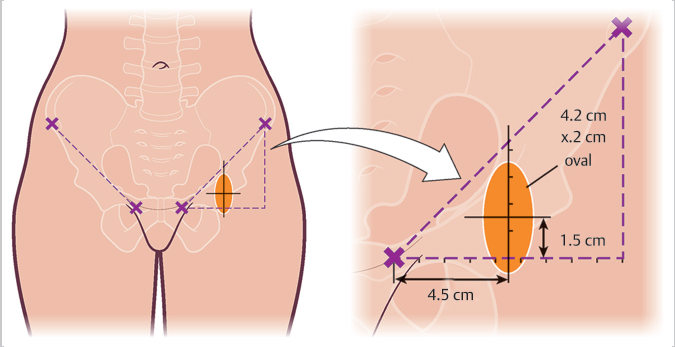
The SCIP flap can be raised as a fasciocutaneous flap known as the groin flap.20 When raised on the suprafascial plane, it is Dr. Koshima’s original description of the SCIP flap.21 On this plane, one can take the SCIP flap as a chimeric flap to include lymph nodes to address patients with lymphedema or extend the dissection to the iliac bone to reconstruct small bone defects.22 The dissection to include the bone may become very tedious as the small branches from the perforator can be difficult to identify. The donor site may have prolonged leakage of the lymphatic fluid if the lymphatic vessels and nodes are not adequately coagulated.
The GAP flap can be based on either the superior or the inferior gluteal artery.23 When elevating with the full fat layers, it can be used to reconstruct the breast.24 When elevating above the superficial fascia, it can be used to resurface the lower extremity or a weight-bearing foot. There can be many designs available from each GAP.25,26 It can be designed in multiple axes directing to the trochanter or toward the flank. The design variation depends on the donor site appearance or the position of the defect if it is used as a local flap to cover the defect usually originating from a pressure sore.