Chapter 49 Principles of new invasive modalities
![]() For additional online content visit http://www.expertconsult.com
For additional online content visit http://www.expertconsult.com
A Laser-Assisted Liposuction
Introduction
Liposuction is considered the gold standard procedure for body sculpting and contouring.1 The introduction of the tumescent technique has reduced the risk of bleeding, reducing the need for general anesthesia and hospitalization, and diminished postoperative ecchymoses associated with liposuction.1–5 Other advances include the refinement of body site-specific cannulas and the use of manual syringe suction for autologous fat transfer and fine contouring.6 More recently, ultrasound-assisted liposuction (UAL), power-assisted liposuction (PAL), vibroliposuction, and laser-assisted liposuction have shown promise in facilitating fat removal and in reducing procedure duration, surgeon strain, patient recovery time, and postoperative pain.1,4,5,6
A detailed study7 described the physics, quantification and safety of subdermal laser heat treatment. Later, the same authors presented a preliminary report on skin shrinkage and increased elasticity as a result of multi-wavelength laser application.8 Although the aforementioned study showed promising results, it did not directly compare the effects of laser-assisted liposuction to those of an internally controlled traditional liposuction alone. A subsequent study obtained quantitative, objective data for comparing tissue shrinkage and skin tightening achieved by laser-assisted liposuction vs. liposuction alone. Skin shrinkage was quantified by changes in surface area and skin tightening was quantified by changes in the skin stiffness index.9 This led to the proof of the unique significance of laser energy application; the first concurrent method to definitively address skin laxity in the body contouring patient without the need for invasive excision intervention.
Preoperative Preparation
Patients are consulted in terms of fat reduction and skin laxity improvement. Since specific areas are treated, patients are marked for the usual fat attention in addition to 5×5 cm squares representing the areas of skin laxity energy application (Fig. 49.1). Tumescent fluid, approximately 50–100 ml per 5×5 cm2 sector, is administered. In addition, patients are given two oral Valium (10 mg each) and two Percocet® (acetominophen 325 mg/hydrocodone 5 mg) approximately 20–30 minutes prior to tumescent fluid application (Fig. 49.1). The procedure is rarely done with more than oral and local anesthesia.
The surgical plan is for a biplanar technique to disrupt adipose cells, resulting in a more liquefied material that can be removed through a smaller cannula. This refines the removal, especially closer to the surface, reducing contour irregularity from larger instrumentation. Surface temperature goals of 40–42°C, if measured superficially, or 47–52°C, if measured deep, are used for increased skin elasticity and tightening. This is the most important aspect of this procedure for managing patient expectations and diligence in achieving these temperature goals, uniformly, is of utmost importance. It is also necessary to stress to the patient that the skin tightening goal is a function of their age, genetics and skin condition from environmental factors such as smoking and sun. If expectations for outcomes are in terms of a surgical procedure, then that should be performed. For optimizing outcomes, please see Box 49.1.
Box 49.1 Optimizing Outcomes
Laser-Assisted Liposuction
• Limit the size of the procedure to 24 sectors: Proper energy delivery takes time (5 min per sector) for the whole procedure.
• Do not give insufficient energy to potentially reduce skin tightening.
• Heat causes swelling for the first 4 weeks. Any areas of dense swelling or firmness need to be treated with massage or mechanical interventional devices if available.
• Indicate to patient that the skin component takes at least 90 days to take effect.
• Avoid the nerves of the face; neck below mandible is fine.
• Treat mild to moderate fat volumes.
• Avoid hanging skin in lieu of surgery.
• Best areas are neck, brachial, lower abdomen, medial thigh, and back rolls.
Surgical Technique
The laser system used (Triplex®, Cynosure, Westford, MA, USA) permits individual as well as sequential emission of 1064 nm, 1320 nm, and 1440 nm wavelengths. Energy is delivered to the subdermal tissue through a 600 or 1000 µm fiber threaded through a 1 mm microcannula and extending 2 to 3 mm beyond the distal end of the microcannula. When the microcannula is inserted in tissue, the laser is activated and the microcannula is moved slowly and evenly through the deep fat layer with a 1064–1440 nm combination (Fig. 49.2), or the superficial subdermal layer with a 1064–1320 nm combination. Wavelength combinations are used for preferential target affinity of fat (deep) and water (dermis), respectively, for ideal absorption and performance.
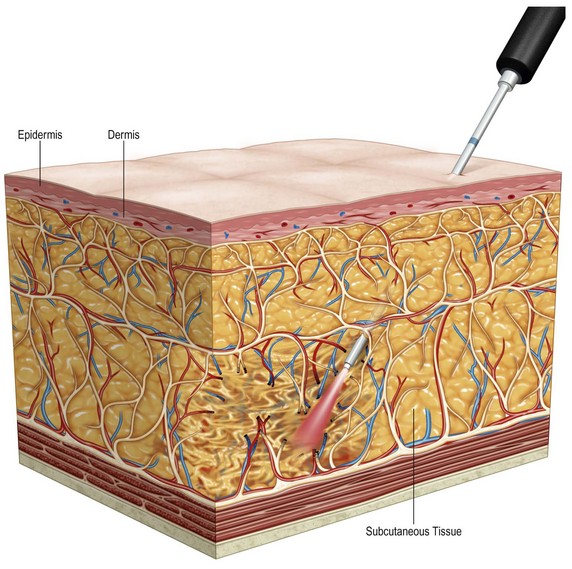
FIG. 49.2 Diagrammatic representation of placement of deep laser energy for adipocyte and fibrous disruption.
Patient safety is addressed with respect to energy delivery via an accelerometer delivery system (Smart Sense®, Cynosure) attached to the laser handpiece, used to minimize the occurrence of localized thermal damage during treatment, If, during treatment, the surgeon slows the motion of the handpiece, the laser power delivered drops accordingly. If the handpiece stops, energy delivery ceases within 0.2 s. Temperature safety is measured with a thermistor probe at the tip of the cannula, which is then set for a safe range measured below the skin, usually 47–52°C (Fig. 49.3).
FIG 49.3 Appears ![]() ONLINE ONLY
ONLINE ONLY
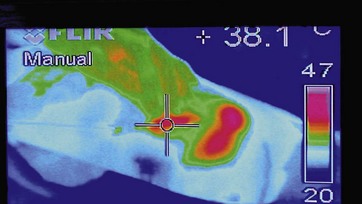
The laser will stop firing when this threshold is reached, again adding to the safety of the system. Although at this point the thermistor is fully capable of measuring temperature throughout all levels of the procedure, previous surface measurements were taken with a laser-guided thermometer, needing an additional assistant to operate it (Fig. 49.3). The accuracy of these devices was confirmed in studies using a thermal camera (Fig. 49.4).
FIG 49.4 Appears ![]() ONLINE ONLY
ONLINE ONLY
The tissue is treated using a two-layer/two-step technique. The first step is to treat the deep fat layers (1–3 cm below the epidermis) within the premarked squares (Fig. 49.2). Two to four incisions, 1 mm each, are made with a number 11 blade in each treated area, for insertion of the microcannula. Subsequently, in the second step, the superficial subdermal layer (0.5 cm below the epidermis) is treated (Fig. 49.5). The entire surgically marked site(s) are then aspirated with a standard 3 mm suction cannula to remove any remaining fat, disrupted cells, and free fat oils.

FIG. 49.5 Superficial laser application just under the dermis, with visualization of helium neon guiding beam.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree