Pressure Sores
Karen L. Powers
Linda G. Phillips
INTRODUCTION
A pressure sore is localized soft-tissue injury resulting from unrelieved pressure, usually over a bony prominence. Because areas of tissue pressure depend on patient position, the term “pressure sore” is preferred, rather than bedsore or decubitus ulcer. Relieving the pressure caused by patient positioning is the key to prevention and healing. Factors contributing to the development of pressure sores include decreased mobility, decreased sensation, spasticity, shearing forces, friction, and moisture. With so many factors playing a part in pressure sore development, prevention and treatment frequently require a multidisciplinary approach, often with the plastic surgeon consulted for reconstruction of the soft-tissue defect.
The most widely accepted pressure sore staging system was revised by the National Pressure Ulcer Advisory Panel in 2007 to include the original four stages and an additional two stages regarding deep tissue injury and unstageable pressure sores (Table 98.1). Stage I includes intact skin with nonblanching erythema, stage II includes partial-thickness loss of dermis, stage III includes full-thickness tissue loss, and stage IV includes exposed bone, tendon, or muscle.1 Additional classification includes suspected deep tissue injury, usually characterized by maroon localized intact skin or blood-filled blister, and unstageable, which is a full-thickness ulcer with eschar at the base. Limitations exist in this system; signs like skin erythema can be present in more than one stage and dark skin pigmentation can actually obscure the presence of erythema, necessitating other diagnostic signs like increased skin temperature, edema, and induration, to accurately stage the wound. Long-standing wounds of the pelvic girdle warrant careful examination and possible imaging to evaluate for extension into deeper structures, such as the acetabulofemoral joint.
EPIDEMIOLOGY
The incidence of pressure sore formation is variable but the patient populations commonly studied include those in acute care settings, nursing home patients, and paraplegic populations. In general, pressure sores develop in approximately 9% of all hospitalized patients, affecting 2.5 million people annually.2 For acute and long-term care facilities, the overall reported prevalence ranges between 3.5% and 29.5%.3 In addition to causing pain, suffering, and disability, pressure sores contribute to over 60,000 deaths per year according to the National Pressure Ulcer Advisory Panel.1 Data from the National Pressure Ulcer Long Term Care Study suggest that up to 19% of new patients develop a pressure ulcer while in long-term care and 22% arrive with an existing pressure ulcer.4 Beginning in October 2008, The Centers for Medicare and Medicaid Services ended reimbursement of acute care facilities for the development of a hospital-acquired stage III or IV pressure sores, thereby compounding the challenge of pressure sore prevention with the essential task of documentation of pressure sores present on admission.
TABLE 98.1 NATIONAL PRESSURE ULCER ADVISORY PANEL STAGING SYSTEM, 2007 | ||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||
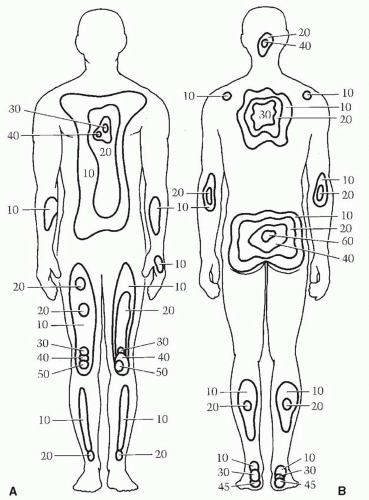
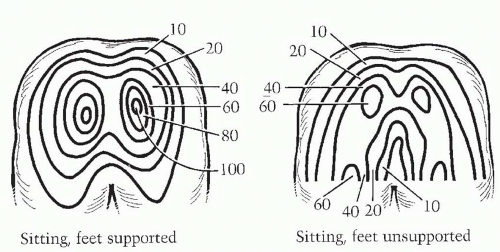
Multiple studies have demonstrated that age, moisture, immobility, and friction/shear are key risk factors.5 Impaired sensory perception is known to contribute to the development of pressure sores but the incidence in patients with spinal cord injuries varies greatly. The Braden Scale, incorporating factors such as mobility, can be used to predict an individual’s pressure sore risk. Stal et al.6 cited a 20% incidence in paraplegic patients and a 26% incidence in patients who were quadriplegic. For the majority of patients, wounds develop in either the supine or seated position. Up to 75% of all pressure sores are located around the pelvic girdle. This is not unexpected, as it mirrors the distribution of pressure in supine and sitting positions (Figures 98.1 and 98.2). A study of a large cohort from a statewide Arkansas registry cited significant risk factors in the spinal cord-injured patient, including being underweight, use of pain medications, smoking, suicidal behaviors, history of incarceration, and alcohol and drug use.7
PATHOPHYSIOLOGY
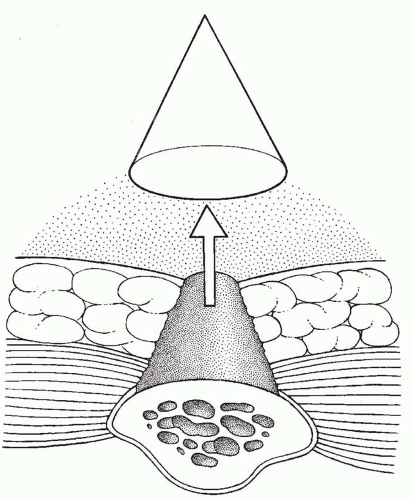
Compression of soft tissues results in ischemia and, if not relieved, it will progress to necrosis and ulceration, even in well-vascularized areas (Figure 98.3). What is seen on the surface is often merely the tip of the iceberg, as confirmed by pressure measurements taken over bony prominences8 (Figure 98.4). In susceptible patients, progression from excessive pressure to irreversible ischemia and tissue necrosis is accelerated by infection, inflammation, edema, and other factors that are not yet understood.
Pressure
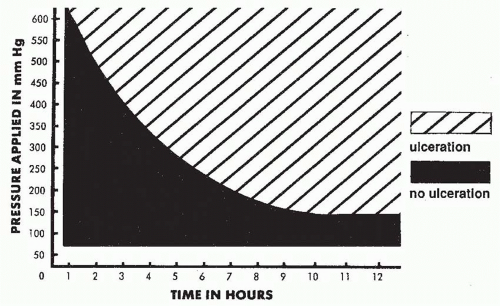
Ischemia occurs when external pressure exceeds the capillary pressure, which was shown by Landis9,10 in the 1930s to be 12 mm Hg on the venous end and 32 mm Hg on the arterial end. If the external compressive force exceeds capillary bed pressure (32 mm Hg), capillary perfusion is impaired and ischemia will ensue. Original dog studies demonstrated an inverse parabolic relationship between the amount of pressure and duration of exposure (Figure 98.5). Early studies demonstrated that pressure of 70 mm Hg applied over 2 hours was sufficient to cause pathologic changes in dogs. Dinsdale11 confirmed these results in a pig model; perhaps just as importantly, he was also able to demonstrate the absence of injury if pressure could be relieved for as little as 5 minutes, even with pressures as high as 450 mm Hg. Similarly, Daniel et al.12 demonstrated that pressure of 500 mm Hg applied for 2 hours, or pressure
of 100 mm Hg for 10 hours, was sufficient to cause muscle necrosis. Interestingly, it was not until pressure of 600 mm Hg was applied for 11 hours that ulceration of the skin could be seen. Not only did these results confirm the relationship between pressure and time, but they also demonstrated that the initial pathologic changes occurred in the muscle overlying the bone, followed by the more superficial soft tissue, involving the skin last.13 Several classic studies investigated pressure and its effects as it relates to location, time, and intensity in humans (Figures 98.1 and 98.2). In the supine position, the maximal recorded pressures were 40 to 60 mm Hg near the heels, buttock, and sacrum. In the sitting position, pressures were greatest near the ischial tuberosities.
of 100 mm Hg for 10 hours, was sufficient to cause muscle necrosis. Interestingly, it was not until pressure of 600 mm Hg was applied for 11 hours that ulceration of the skin could be seen. Not only did these results confirm the relationship between pressure and time, but they also demonstrated that the initial pathologic changes occurred in the muscle overlying the bone, followed by the more superficial soft tissue, involving the skin last.13 Several classic studies investigated pressure and its effects as it relates to location, time, and intensity in humans (Figures 98.1 and 98.2). In the supine position, the maximal recorded pressures were 40 to 60 mm Hg near the heels, buttock, and sacrum. In the sitting position, pressures were greatest near the ischial tuberosities.
Inflammation
Maintenance of soft-tissue integrity requires tightly regulated interactions between cells, growth factors, their receptors, extracellular matrix molecules, and a variety of proteases and their inhibitors. When tissue is injured by causes such as unrelieved pressure, there is a demargination and influx of cells responsible for inflammation. For injuries to heal, a series of events unfolds, including vasoconstriction/vasodilatation, coagulation, influx of proinflammatory cells like neutrophils and macrophages, and, finally, matrix formation/maturation. In chronic wounds, there is a breakdown in this sequence, leading to a non-healing wound. Altered immune function has been implicated in the development of pressure sores and molecular evidence points to an imbalance between matrix metalloproteases (MMPs) and tissue inhibitors of metalloproteases (TIMPs). MMPs, especially 1 and 9, are key to cell signaling and migration, whereas TIMPs, especially 1 and 2, bind to these proteases and presumably protect uninjured tissues. Numerous subsequent studies have documented the presence of elevated levels of various MMPs and decreased levels of TIMPs in chronic wounds, or an imbalance between the levels of MMPs and TIMPs.14 In patients with spinal cord injuries, the loss of sympathetic tone results in vasodilatation of denervated tissues, which further intensifies this problem.
Edema
Approximately 80% of soft tissue mass is fluid. External pressure on soft tissue increases plasma extravasation, which leads to edema formation, a significant factor in pressure sore formation. Denervation contributes to pressure sore development through loss of blood vessel sympathetic tone and its subsequent vasodilatation, vessel engorgement, and edema. Circulatory deficiencies, such as heart failure, renal failure, and venous insufficiency, are risk factors for pressure sore formation in part due to their propensity to increase edema in dependent soft tissue. On a molecular level, inflammatory mediators such as prostaglandin E2 released in response to the trauma of compression increase leakage through the cell membranes and increase interstitial fluid accumulation.
PREOPERATIVE CARE
As Tchanque-Fossuo et al.5 noted in a 2011 review of evidence-based approaches to pressure sores, the goals of management for a patient with a pressure sore are (1) prevention of complications, particularly invasive infection, related to the existing sore; (2) preventing the existing sore from getting larger; (3) preventing sores in other locations; and, if possible, (4) closure of the wound. Most authors report high recurrence rates after surgical closure of pressure sores. Successful pressure sore coverage is multifactorial but key components include resolution of infection, the preoperative/postoperative relief of pressure, and, for cases of chronically non-ambulatory patients, the control of spasm and contractures.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree