Nipple Reconstruction
Michael S. Beckenstein
Nipple reconstruction is an essential component in the creation of an attractive breast. When viewing breasts, the eyes are drawn to the nipple-areola complexes. A surgeon can create aesthetically pleasing breast mounds, but the improper placement of the nipple-areola complexes will compromise the final result. In addition, errors in nipple-areolar placement are challenging to correct. Nipple reconstruction techniques may seem minor in the overall scheme of breast reconstruction; they are a major factor in the final result and demand meticulous attention to achieve good aesthetic results.
The goal of nipple-areolar reconstruction is to create nipples that are appropriately located on the breast mound and are of appropriate size, shape, color, and texture. Projection is another key aspect of nipple reconstruction which can be varied to attain a patient’s goal. There are many techniques of nipple-areolar reconstruction that can be employed to suit the goals of both the patient and the surgeon. Some techniques are better suited for autologous breast reconstruction where there is more subcutaneous adipose tissue and others might be best applied to prosthetic breast mounds with thinner subcutaneous tissue.
MARKING
When performing unilateral breast reconstruction, simply triangulating the distances from the contralateral nipple onto the reconstructed breast mound may not result in an appropriate placement. Because there are usually breast mound asymmetries, the surgeon uses aesthetic judgment to position the nipple. One way to approximate the nipple-areola position is to cover the contralateral breast and carefully study the reconstructed breast mound and place a mark where the nipple location appears appropriate. The contralateral breast is then uncovered and a careful comparison is made. Adjustments are made as deemed necessary. The patient is allowed to have input into the nipple-areola location as well. A round adhesive bandage is placed on this location. The patient can relocate the bandage to what she feels is an appropriate location.
In bilateral reconstructions, there is more latitude in nipple location yet the marking methods are similar. Initially, each breast is assessed separately. Careful inspection of both breasts is then performed and adjustments/compromises made as necessary.
METHODS
Ideally, the surgeon is familiar with a variety of techniques and will choose one based on the goals of the patients and the amount of tissue available on the breast mound. The more common reconstruction methods consist of local flaps, grafts, or a combination of both. Acellular dermal matrices (ACMs) used alone or in conjunction with local flaps are being utilized as well as injectable materials. Tattooing can also serve as the sole form of nipple-areola construction in select patients.
Local Flaps
Local flaps are the most frequently performed methods of nipple reconstruction today. A central dermal fat pedicle is wrapped by full- or partial-thickness skin flaps, creating a nipple. These procedures employ skin grafts or primary closure to close the donor defects. Examples of the commonly used pedicle flaps are the skate flap, modified skate flap, star flap, cervical visor (CV) flap, wrap flap, and fishtail flap. To be successful in creating nipples of sufficient projection and dimension, the breast mound must provide well-vascularized soft tissue of sufficient thickness. One must keep in mind that these are second-generation flaps; that is, they are created from flaps of tissue that were themselves either mastectomy flaps or autologous transferred flaps! These methods may not be suitable for reconstructions in patients with thin skin or irradiated tissue. Local flaps are best suited for breast mounds composed of autologous tissue where these soft-tissue requirements are met. These local flaps often lose volume and contract substantially over time. Consequently, an initial overcorrection is warranted. In unilateral reconstruction, the local flap is made 50% to 75% larger than the contralateral nipple size in anticipation of atrophy. If the final result is substantially larger than desired, a reduction is readily performed as an office procedure. It is easier to reduce the size than to perform a secondary procedure to increase the size of a volumedepleted, contracted nipple.
Technique.
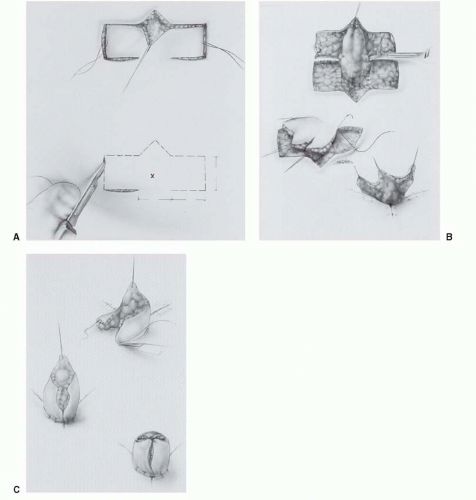
All local flap procedures begin by designing the flaps so that the base of the flap is located at the marked position of the nipple. The flap dimensions are drawn within the confines of a 38-, 42-, or 45-mm “cookie cutter.” The skin incisions are then made; the lateral flaps are raised as full- or partial-thickness skin grafts. The dermal fat pedicle is incised into the subcutaneous adipose layer, raising the dermal-fat pedicle 90° to the plane of the breast mound. Care is taken to preserve the delicate blood vessels in the adipose tissue to minimize tissue atrophy postoperatively. The dermal fat pedicle must be of sufficient thickness to provide the necessary bulk for the nipple. The donor site is closed in layers, approximating the deep dermis with an absorbable 4-0 suture. The skin is closed with 5-0 absorbable simple mattress sutures. The lateral skin flaps are then rotated around the dermal fat pedicle and sutured with simple mattress sutures. All remaining skin edges are closed in a similar manner. Figure 63.1A-C demonstrates these tenets, using Hartrampf’s Penny flap as the example. A dressing is applied, consisting of the base of a 20-mL syringe, cushioned by an eye pad with the center cut out. A 1-in. Xeroform strip is placed into the barrel of the syringe after it is placed over the newly reconstructed nipple and a Tegaderm dressing is applied. An alternative dressing consists of an arterial line protector, which is then injected with antibiotic ointment, after it is placed over the nipple. The dressings are removed 1 week postoperatively. The patient wears the plastic nipple shields for an additional week, placing them through the center of an adhesive bandage. These dressings are changed twice daily, applying antibiotic ointment to the nipple.
Grafts
The use of grafts is another effective method of nipple-areola reconstruction. Grafts are particularly useful in prosthetic reconstructions as there is often a paucity of soft tissue to create nipples with sufficient projection using the local flap techniques. The disadvantage of autografts is that they require a
donor site. Grafts of tongue, earlobe, toe, and labia have been used, but these donor sites are undesirable and are of mostly historical significance.
donor site. Grafts of tongue, earlobe, toe, and labia have been used, but these donor sites are undesirable and are of mostly historical significance.
One of the best methods in unilateral breast reconstruction is a composite nipple graft from the contralateral nipple. If the patient has sufficient projection in the contralateral nipple and is willing to use it as a donor site, excellent nipple symmetry can be attained. This is an easy technique to perform and can readily be accomplished in the office. The patient must be informed that the donor nipple may suffer loss of sensibility and erectile and ductile function. The graft can be harvested in several ways, depending on the nipple size and projection. If there is sufficient donor nipple projection, a simple transection of the distal 30% to 50% of the nipple can be performed. The donor nipple can be closed primarily with 4-0 chromic, interrupted, vertical mattress sutures. Alternatively, a central vertical wedge can be excised closing the defect in a similar fashion. If the donor nipple does not have a significant projection to accommodate simple transection, a wedge can be excised along the horizontal axis (analogous to a piece of pie), closing the defect primarily. This will diminish the diameter of the donor nipple but will not alter the projection. The appropriate diameter of skin is excised to prepare the recipient site. The graft is then placed duct side down and sutured to the skin with 4-0 chromic mattress sutures. Another method, which increases both the nipple size and projection, raises a small, local skin flap 90° from the plane of the recipient breast mound. The nipple graft is sutured to the base of the recipient site and to the local flap edges creating a hybrid, local flap-composite graft nipple reconstruction. Dressings, similar to those used for local flaps, are employed. The donor site is dressed with antibiotic ointment and a bandage. The graft dressings are changed 1 week postoperatively, and are dressed every other day with Xeroform for an additional week. Although the graft may appear dark and dusky after 1 week, it is usually pink and viable within 2 to 3 weeks. Over the next 2 to 3 months, the graft may grow approximately 20% to 30% larger, attaining the appearance of the contralateral nipple.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree