Abstract
The skin has one pigment-forming cell: the melanocyte. Melanocytes are dendritic cells found in the basal layer of the epidermis. Nevus cells, a type of melanocyte, found in the basal layer of the epidermis as well as in the dermis, are arranged in nests, and do not have dendritic processes. Melanocytes contain tyrosinase, the enzyme necessary for pigment (melanin) synthesis, and are thought to be derived from a progenitor cell in the neural crest.
Pigmented growths ( Table 6.1 ) are the result of an increased number of melanocytes, nevus cells, or pigment deposition. The diagnosis of malignant melanoma is important because it can be recognized early, when it is curable.
Chapter Contents
Definition
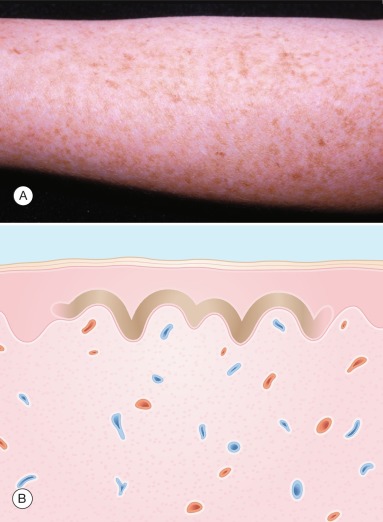
A freckle (ephelis) is a brown macule found in sun-exposed areas of the skin ( Fig. 6.1 ). The amount of melanin in the basal area of the epidermis is increased, with no increase in the number of melanocytes.
Incidence
Freckles are a common incidental finding during a skin examination and are rarely a reason, in and of themselves, for seeking medical attention.
History
Freckles usually appear before 3 years of age and darken after ultraviolet (UV) light exposure. The patient has a history of sunburning easily.
Sunlight darkens freckles.
Physical Examination
The freckled individual typically has a fair complexion and reddish or sandy hair. Hundreds of freckles occur on sun-exposed skin. They are 1 to 6 mm, irregularly shaped, discrete brown macules.
Freckles occur only in sun-exposed areas.
Differential Diagnosis
Lentigo and junctional nevus can look like a freckle. Actinic lentigo does not darken with sun exposure and is acquired later in life. In contrast, freckles darken after sun exposure and are present from early childhood. Lentigo simplex is acquired in childhood, but the lentigines are not confined to sun-exposed skin. Junctional nevi and freckles are acquired in childhood. Darker pigmentation and lack of change after sunlight exposure favor a diagnosis of junctional nevus.
- ●
Junctional nevus
- ●
Actinic lentigo
- ●
Lentigo simplex
Laboratory and Biopsy
Ordinarily, freckles do not require biopsy ( Fig. 6.1B ).
| Frequency (%) a | History | Physical Examination | Differential Diagnosis | Laboratory Test (Biopsy) | |
|---|---|---|---|---|---|
| Freckle | Appear before age 3 years | Tan macule, sun-exposed skin | Junctional nevus Lentigo Seborrheic keratosis | No | |
| Lentigo | 0.2 | Acquired at any age | Brown macule | Junctional nevus Freckle Seborrheic keratosis | If uneven color |
| Melanoma | 0.3 | Recent acquisition Itches Bleeds Growing | Excision or deep shave biopsy | ||
| Superficial spreading | Irregular surface, border, color | Nevus Seborrheic keratosis Angioma Pigmented basal cell carcinoma | |||
| Lentigo maligna | Irregular surface, border, color | Actinic lentigo Seborrheic keratosis | |||
| Acral lentiginous melanoma | Irregular surface, border, color | Nevus Tinea nigra palmaris | |||
| Nodular | Blue-black nodule | Blue nevus Pyogenic granuloma Angioma Dermatofibroma | |||
| Melasma | 0.2 | Adults | Brown macules on face | Postinflammatory hyperpigmentation Freckle | No |
| Nevus | 2.8 | Not acquired past 3rd decade | Flesh- or brown-colored macule or papule; smooth or verrucous surface | Melanoma Seborrheic keratosis Skin tag Neurofibroma Dermatofibroma Basal cell carcinoma Lentigo Freckle | If change |
a Percentage of new dermatology patients with this diagnosis seen in the Hershey Medical Center Dermatology Clinic, Hershey, PA.
Therapy
Freckles should be accepted as normal. Prevention by sunlight avoidance is effective but not practical.
- ●
None
Pathogenesis
Ultraviolet radiation induces an increase in melanin pigment in the basal layer of the epidermis without an increase in melanocytes.
Lentigo
- 1.
Lentigo simplex occurs in childhood and is idiopathic
- 2.
Actinic lentigo occurs in adults and is sun-induced
Definition
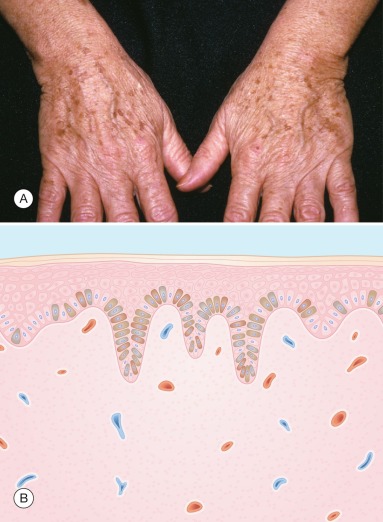
A lentigo (plural, lentigines) is a brown macule caused by an increased number of melanocytes. Two types are recognized: lentigo simplex lesions arise in childhood and are few in number, whereas actinic (solar) lentigines ( Fig. 6.2 ) arise in middle age and are numerous in sun-exposed skin.
Types of lentigo:
- 1.
Simplex – few, congenital or in childhood
- 2.
Actinic – many, sun-exposed skin, in middle age
Incidence
Lentigo simplex is uncommon. Actinic lentigines are found on more than 90% of Caucasians after the age of 70 years, but seldom cause a patient to seek medical advice.
History
Lentigo simplex may be congenital or may arise in childhood. It has no relation to sun exposure. Conversely, actinic lentigo is acquired in middle age, does not fade, and occurs in sun-exposed skin. Patients often call actinic lentigo “liver spots.”
Physical Examination
Lentigo is a uniform, tan, brown, or dark brown macule. Lentigo simplex is sharply marginated and occurs anywhere on the body and mucosae. These lesions are usually few in number.
Lentigo is a brown macule with uniform color.
Actinic or solar lentigo is a tan or brown macule, ranging in size from several millimeters to several centimeters, with distinct borders. The lesion occurs in sun-exposed areas of the body: particularly on the dorsum of the hands, neck, head, shoulders, upper trunk, and lower legs.
Differential Diagnosis
In childhood, the differential diagnosis of lentigo includes junctional nevus and freckle . In adults, seborrheic keratosis and malignant melanoma in situ (lentigo maligna) are included in the differential diagnosis. The most important of these is lentigo maligna, which appears as an irregularly colored (varying shades of brown and black), irregularly bordered macule on sun-exposed regions of the body.
- ●
Junctional nevus
- ●
Freckle
- ●
Seborrheic keratosis
- ●
Malignant melanoma in situ
Laboratory and Biopsy
Biopsy is seldom indicated unless there is concern for a malignant melanoma. If biopsy is performed, the histologic picture is characterized by an increased number of melanocytes within the epidermis as well as increased pigmentation within the keratinocytes. The rete ridges may be normal or elongated ( Fig. 6.2B ).
Therapy
No therapeutic intervention is required, except for cosmetic purposes. For multiple actinic lentigo, tretinoin cream 0.1% (Retin-A) applied daily is effective in lightening these photo-aging spots. Irritation, however, is common, thus requiring less-frequent application (every other day or every third day) or use of a less concentrated cream (0.025% or 0.05%). Preparations containing hydroquinone are generally ineffective. A combination product, 2% mequinol plus 0.01% tretinoin solution (Solage) applied twice daily, lightens these spots. Mild freezing with liquid nitrogen or laser destruction of these pigmented lesions is effective. Sunscreens with a sun protective factor (SPF) of 30 should be used to prevent the development of more actinic lentigo.
Course and Complications
Lentigo has no malignant potential. The multiple lentigines syndrome , a rare but distinctive syndrome, is characterized by hundreds of lentigines on the trunk, head, and extremities, including the palms and soles. It is dominantly inherited and also called the LEOPARD syndrome ( L entigines, E lectrocardiographic abnormalities, O cular hypertelorism, P ulmonary stenosis, A bnormal genitalia, R etarded growth and development, and D eafness).
Syndromes with numerous lentigines:
- 1.
LEOPARD
- 2.
Peutz–Jeghers
Peutz–Jeghers syndrome is a dominantly inherited trait that is distinctive because of numerous lentigines occurring around the mouth and eyes as well as on the lips, oral mucosa, hands, and feet, in association with gastrointestinal polyps. Intussusception, hemorrhage, and malignancy are complications of these polyps.
Malignant Melanoma
- 1.
Thin melanoma is curable
- 2.
Prognosis is best predicted by depth of invasion (Breslow thickness) in primary cutaneous melanoma
- 3.
Sentinal lymph node biopsy is prognostic, not therapeutic
Definition
Malignant melanoma is a cancerous neoplasm of pigment-forming cells, melanocytes, and nevus cells. Clinically, its hallmarks are an irregularly shaped and colored macule, papule, or plaque. Four types of melanoma are recognized ( Table 6.2 ): (1) superficial spreading; (2) lentigo maligna; (3) nodular; and (4) acral lentiginous.
| Type | Location | Median Age (years) | Premetastatic | Frequency (%) a | Ethnicity |
|---|---|---|---|---|---|
| Lentigo maligna | Sun-exposed surfaces (head, neck) | 70 | 5–15 years | 10 | Caucasian |
| Superficial spreading | All surfaces (back, legs) | 47 | 1–7 years | 27 | Caucasian |
| Nodular | All surfaces | 50 | Months to 2 years | 9 | Caucasian |
| Acral lentiginous | Palms, soles, nail beds | 61 | Months to 8 years | 1 | Black, Asian |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








