27 Photorejuvenation with Lasers
Cumulative damage to the skin over time from ultraviolet light results in photoaging. Photoaging changes are clinically evident as benign pigmented lesions, such as solar lentigines, freckles (ephelides), hyperpigmentation, melasma, and as benign vascular lesions, such as telangiectasias, poikiloderma of Civatte, rosacea, and cherry angiomas.1 Photorejuvenation refers to the cosmetic treatment of photoaged skin with nonablative lasers and light-based technologies (collectively referred to as lasers*).2 Treatments are most commonly performed on the face, neck, chest, and hands, but may be performed on almost any photodamaged area of the body.3 Photorejuvenation treatments reliably achieve improvements, have short postprocedure recovery times and minimal risks of complications, and are associated with high patient satisfaction.4,5
Laser Principles
Laser treatments are based on the principle of selective photothermolysis. Light-absorbing pigments in the skin, called chromophores, selectively absorb light energy and convert it to heat in the targeted lesions. The lesions are heated, damaged, and eliminated, while the surrounding skin is left unaffected. Photorejuvenation treatment of benign pigmented and vascular lesions is achieved through selectively targeting two main chromophores in the skin, oxyhemoglobin, which is found in red blood, and melanin, which is found in pigmented lesions.6
When treating red vascular lesions, laser energy is absorbed by the oxyhemoglobin chromophore. The vessel is heated, causing injury to the vessel wall and perivascular collagen damage, which results in vessel closure and obliteration. Oxyhemoglobin absorbs light between 510 and 600 nm (Figure 27-1). Lasers used for the treatment of red vascular lesions produce light in this range and include argon (510 nm), potassium titanyl phosphate or KTP (532 nm), and pulsed dye (585 nm) lasers.
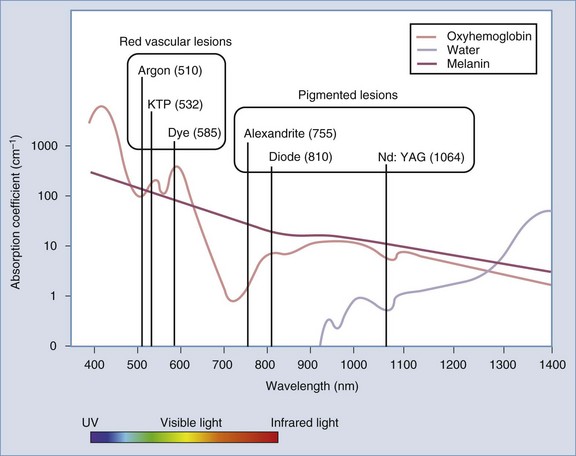
FIGURE 27-1 Absorption spectra of tissue chromophores and lasers commonly used for photorejuvenation.
When treating benign pigmented lesions, such as lentigines, light energy is absorbed by the target chromophore melanin that is contained within the melanosomes of epidermal melanocytes and keratinocytes. The melanosome is heated, ruptured, and the melanin eliminated. Melanin preferentially absorbs light between 650 and 1100 nm (see Figure 27-1). Lasers used for treatment of epidermal pigmented lesions produce light in this range and include ruby (694 nm), alexandrite (755 nm), diode (810 nm), and neodymium-doped yttrium aluminum garnet or Nd:YAG (1064 nm) lasers. The light from KTP (532 nm) and argon (510 nm) lasers has high absorption by both melanin and oxyhemoglobin and can be used to treat both pigmented and vascular lesions.
Several device parameters affect the safety and efficacy of photorejuvenation treatments. These parameters include wavelength, fluence, pulse duration, and spot size (see Laser Parameters in Chapter 19, Aesthetic Principles and Consultation).
Patient Selection
Patients with fair skin (Fitzpatrick skin types I through III) are the best candidates for photorejuvenation treatments because this population presents with the greatest contrast between background skin and target lesions. Both benign vascularities and hyperpigmentation are common complaints in patients with light skin types. Photodamaged skin characteristically shows midface erythema and peripheral lentigines (see Figure 19-1 in Chapter 19).
Indications
Patient Expectations
Photorejuvenation of benign pigmented and vascular lesions may be performed on virtually any body region where photodamage is present. The face, neck, chest, and hands are some of the most commonly treated areas. Noticeable results are evident with a single treatment in properly selected candidates, but typically a series of three to five IPL treatments is required for dramatic improvements.4 Treatment with lasers may require a fewer number of treatments than with IPL devices. Larger red facial vessels, which have more chromophore target, usually respond more dramatically than smaller lacy red vessels or diffuse erythema. Discreet lesions such as cherry angiomas typically resolve with no recurrence after one or two treatments.
Alternative Therapies
Nonlaser treatment options for benign pigmented lesions include liquid nitrogen, exfoliation treatments such as microdermabrasion and chemical peels, and topical skin-lightening products such as hydroquinone. Liquid nitrogen can achieve reduction in pigmentation, however, it is frequently associated with hyperpigmentation and hypopigmentation and it is advisable to restrict use to lighter skin types for this reason. Exfoliation and topical therapies are slower to achieve improvements and results are rarely comparable to those seen with lasers. More aggressive laser treatments with longer recovery times and greater risks of complications, such as ablative carbon dioxide and erbium lasers (fractionated and nonfractionated), are also indicated for pigmented lesions. Electrosurgery may be used for some vascular lesions, although this may scar (see Chapter 14, Electrosurgery). Photodynamic therapy (PDT), utilizing topical photosensitizing medication activated by light, has also been used for photorejuvenation (see the Current Developments section below).
Products Currently Available7–11
Lasers commonly used for treatment of red vascular lesions include the following:
Lasers commonly used for treatment of pigmented lesions include these:
See the Resources section at the end of this chapter for laser manufacturers.
Contraindications
See Chapter 26, Hair Reduction with Lasers, for general laser contraindications. Other contraindications include:
Anatomy
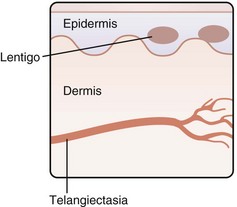
Benign pigmented lesions, such as lentigines, and benign vascular lesions, such as telangiectasias, are some of the most common lesions evident in photodamaged skin. Figure 27-2 shows the relative location of these lesions in the skin, with lentigines in the epidermis and telangiectasias in the dermis.
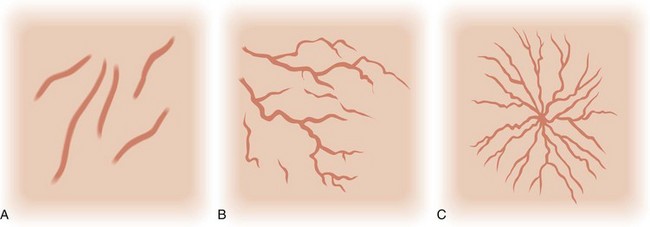
Telangiectasias are these cutaneous vessels that range in size from 0.1 to 1.0 mm. The three main types linear, arborizing and spider, are shown in Figure 27-3. Telangiectasias that arise from dilated arterioles are bright red with small diameters; those from venules are bluish in color with larger diameters; and those from capillaries are fine lacy red vessels or appear as background erythema to the naked eye.12 Red facial telangiectasias seen with photoaging are commonly located in the midface on the nasal ala and dorsum of the nose and cheeks. Telangiectasias may also be associated with clinical conditions such as rosacea, genetic syndromes, and collagen vascular diseases (Box 27-1).
BOX 27-1
Causes of Telangiectasias
Source: Adapted from Habif TP. Clinical Dermatology, 5th ed. St. Louis: Mosby; 2009.
Solar lentigines are small brown macules that increase in size and number with chronic sun exposure and are typically located around the periphery of the face (see Figure 27-8A later in the chapter). Postinflammatory hyperpigmentation can be seen in susceptible individuals, typically darker skin types (Fitzpatrick IV through VI), as brown macules arising at sites of previously inflamed acne lesions or sites of wound healing (see Figure 24-6A in Chapter 24, Skin Care Products). Melasma presents as hyperpigmented reticulated patches and brown macules, typically on the cheekbones, upper lip, forehead, and chin (see Figure 27-13A later in this chapter). It is frequently observed following a change in female hormonal status such as during pregnancy (chloasma) or after initiating use of oral contraceptives.
Cutaneous pigmented lesions may be located in the epidermis, dermis, or in both. Solar lentigines and ephelides (freckles) are located in the epidermis. Postinflammatory hyperpigmentation and melasma may be located in any of these levels. A Wood’s lamp can be used to determine the depth of melanin pigmentation in the skin.13 Epidermal pigmentation appears darker with more contrast against the background skin under Wood’s lamp illumination, whereas dermal pigmentation has less contrast.
Procedure Preparation
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree