13 Flaps
The proper development and implementation of the skin flap is a key skill in reconstruction of skin defects, especially facial defects, following trauma or the removal of benign skin lesions or skin cancers. Although the surgeon should always consider primary, linear closure of a skin defect, there are many circumstances in which a skin flap may be the ideal choice for reconstruction.1,2
Skin flaps may be chosen instead of a primary linear closure to:
Terminology
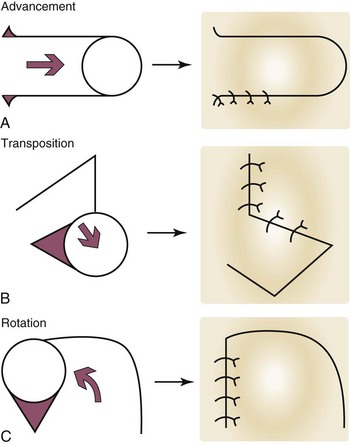
The random pattern flap is further classified by its movement. The three basic types of movement are (Figure 13-1):
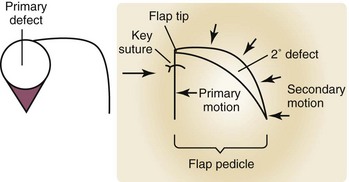
The initial wound that is to be reconstructed is the primary defect, and here it refers to the result of the removal of a skin tumor (Figure 13-2). Once a flap has been advanced, transposed, or rotated into position to close the primary defect, the wound that remains behind at the donor site of the flap is the secondary defect. The primary motion of a flap is the movement that the flap makes when it advances, transposes, or rotates into and closes the primary defect (Figure 13-2). The secondary motion is the movement that the tissue adjacent to and surrounding the flap makes when the final defect is closed. Both the primary and secondary motion of a flap are important in proper flap design. The very end of the flap that fills the primary defect, furthest from the donor site is the flap tip. The flap pedicle is that portion of the flap that connects it to the surrounding skin, and is the conduit for the vascular supply of the flap. The key suture of a local flap is the location in which the first suture is typically placed to provide the initial correct alignment of a flap to fill the primary defect and to direct additional placement of sutures to close the secondary defect. Standing cutaneous cones (dog ears) are areas of local tissue redundancy that occur in wound closure, but that can be minimized, eliminated, or moved to more cosmetically advantageous locations by the correct choice of and meticulous planning for a flap.
Advancement Flap
Conceptual
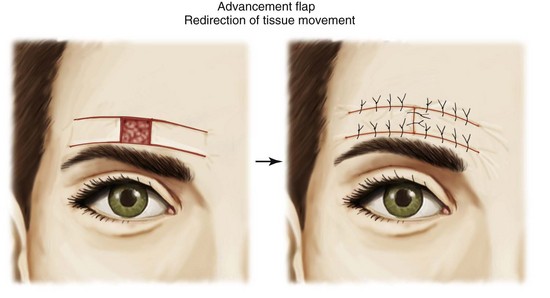
The primary motion of the advancement flap is the sliding of the flap, usually in a single linear vector as it advances into the primary defect. This sliding motion may be unidirectional (single advancement flap) or bidirectional (double advancement flap).3 Although there are several variations on this type of flap, the two main benefits of the advancement flap are as follows:
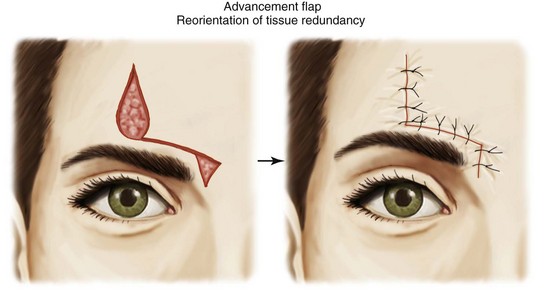
FIGURE 13-4 Reorientation of tissue redundancy to a more acceptable location away from the primary defect.
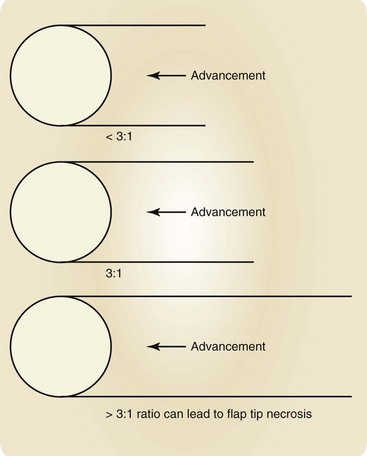
Advancement flaps are also limited by their blood supply. The pedicle of skin and soft tissue must not be compromised. A length:width ratio should ideally not exceed 3 : 1. A long, thin advancement flap in violation of this ratio runs a high risk of distal flap tip necrosis (Figure 13-5).