22 Chemical Peels
Chemical peeling is a skin resurfacing procedure that utilizes topical agents to remove the outermost layers of the skin.1 This controlled method of wounding stimulates a reparative healing response with regeneration of a healthier epidermis and dermis. Chemical peeling, also called chemexfoliation, is commonly used for skin rejuvenation to improve photodamage, reduce hyperpigmentation and acne, and smooth rough skin texture and superficial scarring.2
As with all skin resurfacing procedures, deeper penetration into the skin is associated with greater potential benefits. However, risks and complications also increase with greater depths of penetration into the skin. The depth of penetration achieved with chemical peels ranges from the superficial epidermis to deep dermis. Standard terminology for skin resurfacing depths is illustrated in Figure 19-12 in Chapter 19, Aesthetic Principles and Consultation. The focus of this chapter is light chemical peels, which include very superficial chemical peels that remove the stratum corneum, and superficial chemical peels that remove the entire epidermis and may extend to the upper papillary dermis.3
Chemical peels are one of the most common cosmetic procedures performed in the United States, ranking closely behind botulinum toxin, laser hair removal, and dermal fillers, according to data from the American Society for Aesthetic Plastic Surgery.4 They are technically straightforward to perform and, with minimal start-up costs, they are often one of the first aesthetic procedures incorporated into office practice.1,5 Chemical peels can be readily combined with other minimally invasive aesthetic modalities such as microdermabrasion, topical products, and nonablative lasers to enhance skin rejuvenation results.
Patient Selection
While almost any patient will derive benefit from light chemical peels, patients with mild to moderate photoaging changes such as solar lentigines, skin dullness, rough texture6–8 (e.g., Glogau types I and II), and acneic conditions9,10 typically derive the most noticeable benefits (see Chapter 19 for a description of Glogau types). Results with light chemical peels are slow and progressive, requiring a series of treatments for improvements to become evident. Light peels may also improve fine lines, coarse pores, and superficial atrophic scarring,7 but results are not comparable to more aggressive forms of skin resurfacing, such as medium-depth peels or laser resurfacing. Assessment of patients’ expectations at the time of consultation and commitment to a series of treatments is essential to ensure success with these treatments.
Very superficial chemical peels (e.g., glycolic acid 20%, salicylic acid 20% and retinol) can be used in all skin types (Fitzpatrick types I through VI). Patients with darker skin types (IV through VI) have increased risks with aesthetic procedures, particularly postinflammatory hyperpigmentation, and these gentle peels are one of the treatment options available to manage aesthetic skin conditions in darker skin types such as acne, enlarged pores, and hyperpigmentation (see Chapter 19 for a description of Fitzpatrick skin types).11–14 A conservative approach for providers getting started with superficial chemical peels (e.g., glycolic acid 70%, trichloroacetic acid 20% to 30%, and Jessner’s 4 to 7 layers) is to restrict use of these peels to lighter skin types (Fitzpatrick types I through III) to minimize the risk of complications.
Patients with erythematous conditions such as rosacea, telangiectasias, and poikiloderma of Civatte are also treated conservatively with light chemical peels, as aggressive chemical peels may exacerbate erythema associated with these conditions.15
Indications
Products Currently Available
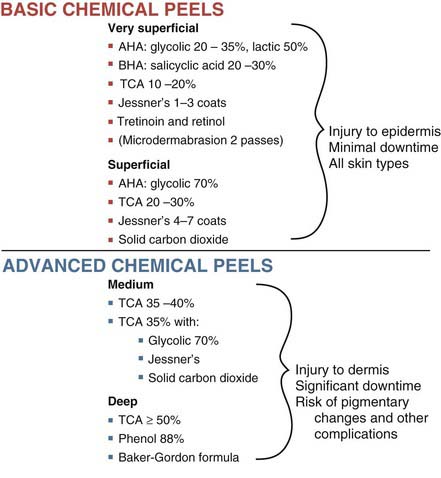
Numerous chemical peels are available and common agents, along with their typical depth of skin penetration, are summarized in Figure 22-1.15–18 Many factors influence the depth of penetration with chemical peels, and although a given chemical peel may be classified as a superficial peeling agent, in practice, peels may vary in the depth of penetration. Figure 22-1 is, therefore, intended only as a general guide for chemical peel depths.
Chemical Peel Depth of Penetration
The depth achieved with light chemical peels ranges from very superficial resurfacing with removal of the stratum corneum, to superficial resurfacing with penetration to the upper papillary dermis. Although the type and concentration of chemical agent used are the main determinants of the depth of penetration in the skin, other factors also influence the depth of penetration including19:
Alpha Hydroxy Acids
Alpha hydroxy acids (AHAs) are derived from organic fruit acids and include: glycolic (sugar cane), lactic (milk), malic (apples), tartaric (grapes), citric (citrus), mandelic (almonds), and phytic (rice) acids. These products are keratolytic and penetrate through the stratum corneum, causing exfoliation by disrupting corneocyte adhesion. AHAs in more acidic formulations (i.e., lower pHs) and in higher concentrations have stronger biologic effects. Glycolic acid peels typically have a pH of 2.5 to 3. Very low pHs (pH < 2) of glycolic acid, however, are associated with greater risk of necrosis and crusting, and do not offer improved results over less acidic preparations.20 AHAs found in topical products as part of daily skin care regimes typically contain low AHA concentrations (10% or less) in less acidic formulations (pH 3.5 or greater).
Glycolic acid (GA) is the most commonly used AHA and is an agent frequently selected by providers getting started with chemical peels.12 Glycolic acid is a small, water-soluble molecule that readily penetrates the skin. GA peels are clear colorless solutions that do not change in appearance upon application to the skin, unlike salicylic acid for example. Figure 22-2 shows GA applied to the dorsum of one hand, and salicylic acid on the other hand with its characteristic white precipitate. Because GA chemical peels do not exhibit a reliable clinical endpoint that is visible, application must be carefully monitored and timed, and the acid neutralized at the appropriate point to control the procedure. Clinical response to glycolic acid can be variable. Some patients have a brisk inflammatory response to low-strength (20% to 35%) short-duration applications (1 to 3 minutes), whereas others may tolerate higher strengths (70%) for longer duration (up to 7 minutes). The effects of GA can be terminated after application through neutralization, which raises the pH and renders the acid ineffective. Neutralization of alpha hydroxy acids may be performed with water or sodium bicarbonate solution (5% to 15%). If neutralization is not performed, AHAs will continue to be active and may penetrate deeper than intended.
Beta Hydroxy Acids
The benefits of SA as compared to the AHAs include less stinging, because SA has a mild anesthetic effect; a visible clinical endpoint with a fine white precipitate (“pseudofrost”), which helps ensure even application (see Figure 22-2), and no requirement for neutralization. Once a white precipitate is formed, there is little additional penetration of the acid and water may be used to wash off the precipitate. A disadvantage of SA is more obvious post-treatment desquamation than with GA. SA peels are available as pure or combination products, and instructions for application and endpoints vary based on the product used. For example, La Roche-Posay’s Biomedic SA peel 30% ends with frosting, whereas SkinCeutical’s SA/Mandelic Peel (SA 20% combined with mandelic acid 10%) does not frost.
Trichloroacetic Acid
Trichloroacetic acid (TCA) is an agent familiar to many clinicians who have used it as therapy for condylomata acuminata (in highly concentrated preparations of 80% to 90%). For superficial chemical peels, it can be used as pure TCA 10% to 30%, or in combination with other peeling agents, such as TCA 15% combined with lactic acid 10%, or TCA 15% combined with SA 15% and lactic acid 15%. After application, TCA causes skin erythema and a whitish discoloration called frosting, which occurs 30 seconds to 2 minutes after application. Histologically, frosting corresponds to coagulation of epidermal proteins and keratinocytes. The intensity of frosting correlates directly with the depth of penetration (see Table 22-1).21 The desired clinical endpoint for superficial depth peels with TCA is level I frosting, visible as patchy erythema with faint white coloration.
TABLE 22-1 Frosting with Trichloroacetic Acid Chemical Peels and Depth of Penetration
Frosting | Depth of Penetration | Clinical Findings |
|---|---|---|
| Level I | Superficial | Patchy erythema with faint patchy white color |
| Level II | Medium | Even white color with some erythema visible through the white |
| Level III | Deep | Opaque confluent white |
Jessner’s Solution
Jessner’s solution is a combination of resorcinol 14%, salicylic acid 14%, and lactic acid 14% in ethanol, which was originally developed to lower the concentration of any one agent and, hence, reduce the risk of toxicity.22 Modified Jessner’s formulations are also available that have no resorcinol, such as salicylic acid 14%, lactic acid 14%, and citric acid 8% in ethanol (e.g., PCA Peel®). Once applied, erythema is followed by a powdery whitening of the skin due to precipitation of salicylic acid. Neutralization is not required, but water may be used to remove the white precipitate. Jessner’s peels are frequently applied in multiple layers, with a period of 4 to 7 minutes of observation for clinical endpoints between layers. Figure 22-3 shows a patient with mild erythema and a faint whitish coloration after application of six layers of a Jessner’s peel.
Retinoids
Topical retinoids, such as tretinoin (Retin-A) and tazarotene (Tazorac), have been principal therapies for acne and skin rejuvenation for many years as part of home skin care regimes. More recently, retinoids have been used as superficial peeling agents ranging from tretinoin peels 0.05% to 1%23 to lower strength preparations containing retinol (e.g., retinol 15% combined with lactic acid 15%). Retinoid peels cause a yellowish discoloration after application. They are not neutralized and are typically washed off by the patient 8 hours after application. Retinol peels may be layered over other superficial peeling agents (such as glycolic and salicylic acids) to enhance desquamation. Figure 22-4 shows a patient immediately after application of six layers of Jessner’s peel followed by one layer of retinol 15% peel combined with lactic acid 15% peel with characteristic yellow skin coloration.
Contraindications