, Shimin Chang2, Jian Lin3 and Dajiang Song1
(1)
Department of Orthopedic Surgery, Changzheng Hospital Second Military Medical University, Shanghai, China
(2)
Department of Orthopedic Surgery, Yangpu Hospital Tongji University School of Medicine, Shanghai, China
(3)
Department of Microsurgery, Xinhu Hospital Shanghai Jiao Tong University, Shanghai, China
In 1983, Donski and Fogdestam first described a distally perforator-based sural fasciocutaneous flap for heel coverage. The flap was based on perforating branches from the posterolateral septum issued from the peroneal artery at 5–7 cm above the lateral malleolus.
On the basis of the results of their preliminary cadaver dissection and their clinical experience, Aoki et al. [1] proved that the vascular anastomosis between the superficial sural artery and the septocutaneous perforator of the peroneal artery forms an arterial network around the entire length of the distal sural nerve.
The clinical and anatomical findings suggested that the sural nerve can be preserved to prevent surgically induced paresthesia [2].
25.1 Vascular Anatomy
Briefly, the superficial sural artery from the popliteal, the septocutaneous perforators from posterior tibial (medial side) and peroneal artery (lateral side), and the myocutaneous perforators from gastrocnemius and soleus form a three dimensional vascular architecture of the posterior lower leg integument. There are prominent longitudinal orientation or axiality of the circulation of fascial, paraneural (sural nerve), and perivenous (lesser saphenous vein) vascular plexuses. There are 4–5 axial communications between this longitudinal neuro-veno-adipofascial plexus and the posterolateral septocutaneous perforators issued from the peroneal artery. The lowest anastomosis from the peroneal artery, the posterolateral supramalleolar perforator, usually 1.2 mm in origin diameter, was located approximately 5 cm above the lateral malleolus. With a distal axial perforator perfusion, blood can run a long distance along the lower resistance longitudinal vascular plexuses and result in a large flap survival without arterial ischemia (Fig. 25.1).


Fig. 25.1
Vascular anatomy of the peroneal artery
There are two venous systems in the calf and sural region, i.e., superficial venous system in the subcutaneous adipose tissue and deep venous system accompanied to the main artery (venae comitantes). Both of these vessels are provided with valves to direct venous return proximally. The superficial and deep venous systems are connected with each other by perforating and communicating veins through the deep fascia.
As a distally based sural neuro-veno-fasciocutaneous flap was raised, all the proximal vessels are cut and ligated, so only the distal vessels have functions for flap circulation. Drainage of venous blood of the flap was thought in the same way as arterial perfusion. It was drained first by the avalvular small venous plexuses of fascial, paraneural, and perivenous to the distal perforating or communicating veins and then to the deep venous system and returned in orthograde direction. Large subcutaneous lesser saphenous vein has no functional role for venous return in distally based sural flaps.
25.2 Case 1: Flap Based on the Distal Most Septocutaneous Perforator
A 56-year-old man sustained a traffic accident injury on his left ankle over the lateral malleolus, resulting a wound measured 10 × 6 cm (Fig. 25.2).


Fig. 25.2
Preoperative view and the flap design
Flap Design
After debridement, a 12 × 7 cm peroneal artery perforator flap supplied by a pivot point 6 cm above the lateral malleolus was designed in an eccentric propeller shape (Fig. 25.3). The longitudinal axis of the flap was a line from the mid-popliteal point to the midpoint between the Achilles tendon and lateral malleolus (Fig. 25.4).


Fig. 25.3
Flap design
Fig. 25.4
Schematic drawing of the flap design
Flap Elevation
An incision was made along the anterior border of the flap. The terminal peroneal septocutaneous perforating vessel was located in the fascial plexus of the flap by careful dissection. During the dissection procedure, particular attention was paid to preserve the vascular pedicle (Fig. 25.5).
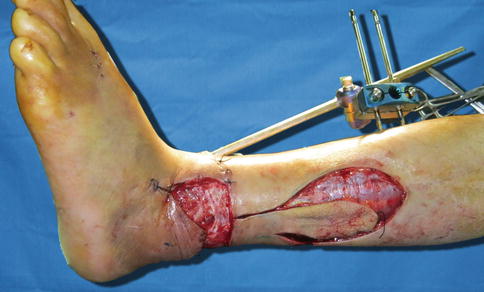
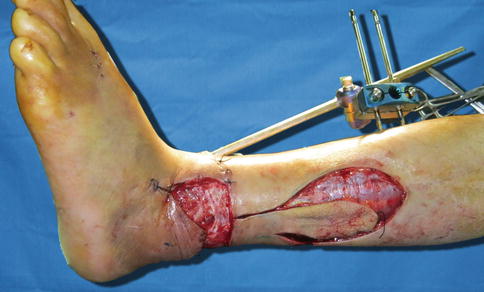
Fig. 25.5
Perforator vessel visualization
The lesser saphenous vein and sural nerve traveled through the proposed flap; they were dissected out and left intact (Fig. 25.6




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree