Type
Depth of penetration
Solution
Superficial
Epidermis
Alpha hydroxy acids:
20–70 % Glycolic acid, lactic, citric, tartaric
Beta hydroxy acids
20–30 % Salicylic acid
Lipo-hydroxy acid
Jessner’s peel (salicylic, lactic, resorcinol)
10–25 % TCA
Medium
Papillary
25–35 % Trichloroacetic acid
Trichloroacetic acid and solid CO2
Trichloroacetic acid and Jessner’s
Trichloroacetic acid and 70 % Glycolic
50 % Trichloroacetic acid
Deep
Reticular
Phenol
Superficial Peels
Superficial depth chemical peels are the mildest of all chemical peels and are indicated for all skin types. They are generally well tolerated and safe with rare complications. These peels create an inflammatory response from the epidermis to the stratum granulosum, or upper papillary dermis. Patients with pigmentary dyschromias, minimal photodamage, and the mildest of rhytids will benefit from superficial peels.
Alpha hydroxy acids (AHA) are extracts from fruits and vegetables and are common agents in superficial peels. Examples include glycolic acid from sugar cane, citric acid from citrus, and lactic acid from milk. The beta hydroxy acids (BHA), salicylic acid and lipo-hydroxy acid, are also agonized as superficial peels, although less commonly used. The AHA and BHA are manufactured in varying strengths and are commonly found incorporated in the many of the cosmetics and in skin maintenance cosmeceutical regimens today. Glycolic acids are one of the most frequently used alpha hydroxy acids, and in the delicate periorbital area, concentrations up to 70 % may be used with careful observation [4]. Caution should be taken when working with glycolic acid, its application is time-dependent, and a neutralizing solution such as water is used to counteract the action. These peels are extensively used today in both physician offices and by trained aestheticians.
The concentration of trichloroacetic acid (TCA) may be adjusted to create a superficial, medium, or deep peel. Low concentrations of 10–25 % generate superficial peels. Trichloroacetic acid at these concentrations produces superficial coagulation of skin proteins and destruction of the epidermis and upper papillary dermis, followed by dermal rejuvenation with new collagen deposition and normalization of elastic tissue [5]. For lower eyelid dyschromias and mild rhytidosis, 20 % TCA is an effective superficial peeling agent. Clinical indication of the depth of penetration of a TCA peel is judged by the intensity of the skin frost, with superficial peels exhibiting erythema or erythema with a light frost.
Used alone, Jessner’s solution (Table 3.2) is a superficial peeling agent which acts as a keratolytic, by targeting the intracellular bridges between keratinocytes. It is depth-dependent, and the penetration used to achieve exfoliation is generally achieved using one to three chemical coats. The first clinical response after if application is mild erythema followed by a light powdery frost of the skin.
Table 3.2
Jessner’s formula
|
Resorcinol
|
14 g
|
|
Salicylic acid
|
14 g
|
|
Lactic acid
|
14 mL
|
|
Ethanol
|
100 mL
|
Re-epithelialization for superficial chemical peels is usually complete within a few days, with beneficial results lasting between 2 and 3 weeks. Patients will notice improvement in skin texture and mild dyschromias, accompanied with a generalized brightening around the periocular area. Since the effects of superficial peels are cumulative, a series of peels repeated at regular intervals (every 4–6 weeks) may be indicated to maintain the results.
Medium-Depth Peels
Medium-depth peels create a skin injury depth from the epidermis to the upper portions of the papillary dermis. These peels are a widespread peel of choice in the periocular region due to its uniform penetration, consistent results, and favorable risk/benefit ratio. Patients that present with crosshatched skin in the lower lid area, crow’s feet, superficial rhytids, and moderate amount of sun damage often benefit from medium-depth peels (Figs. 3.1, 3.2, and 3.3).

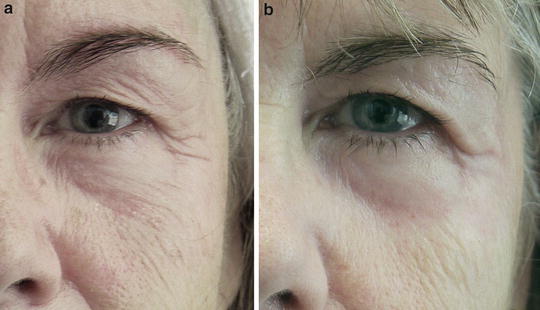
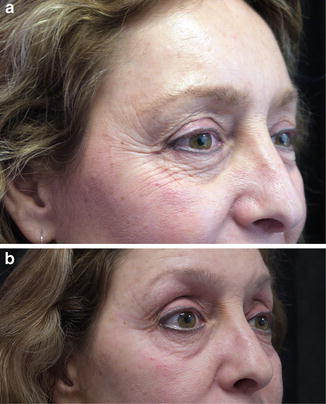

Fig. 3.1
A 45-year-old woman before (a) and after (b) a combination Jessner’s and 35 % TCA of the periorbital area. Note the reduction of dermatochalasis (excess skin) of the lower lid
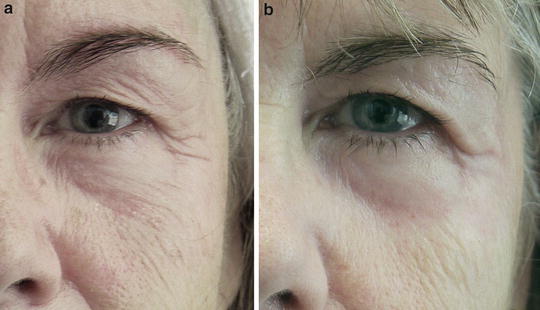
Fig. 3.2
A 50-year-old woman before (a) and after (b) a combination of Jessner’s and 35 % TCA of the periorbital area. An improvement of the dyschromias and wrinkling is evident
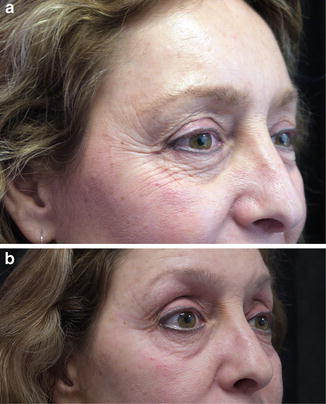
Fig. 3.3
A 49-year-old woman before (a) and after (b) a combination of Jessner’s and 35 % TCA of the periorbital area. The crosshatched skin and rhytids in the lower lid area show overall improvement
The spectrum of medium-depth TCA concentrations starts from 30 % and generally does not exceed 50 % [6]. Concentrations of 50 % or greater have lost favor, as the results are unreliable and have been shown to greatly increase the risk of postoperative scarring [7]. Variables such as the concentration, time of application, and application technique influence the outcome of a TCA peel and are therefore vastly operator-dependent.
Over time, practitioners began combining the lower concentrations of TCA with other agents. The combination produced a deeper penetration of the wounding agent without the associated complications of higher concentrations of TCA [8]. Combinations of TCA with other agents have been described by Monheit with Jessner’s solution [9], Brody and Haily [10] with solid carbon dioxide [10], and by Coleman with 70 % glycolic acid [11, 12]. The authors discovered that these combinations obtain deeper penetration of the wounding agent and have proven to be equal as the use of 50 % TCA but without its associated complications.
The combination peel described by Monheit begins with the application of Jessner’s solution and then sequentially follows with the 35 % TCA. The Jessner’s peel functions as an exfoliant and superficial peel, removing the stratum corneum and penetrating down to the basal layer of the epidermis, allowing for a deeper penetration of the 35 % TCA and a more even application of the peeling solution [13]. This combination Jessner’s/35 % TCA peel has been shown to produce predicable results with a measured decrease in complications. Patients generally develop a light crusting in 3–5 days and will exfoliate completely in 7–10 days. Patients may return back to work in 7 days, using light makeup to cover the pink and erythematous color of the freshly peeled skin. This combination medium-depth peel is the author’s peel of choice in the periorbital area and will be described in detail in this chapter.
TCA solutions are prepared commercially or in the office from crystals mixed with distilled water and compounded in a weight-to-volume preparation. Clear communication with those preparing the solution is paramount, bringing attention to the fact that the dilution is weight to volume, assuring a standardized concentration. The solution should be carefully mixed before usage due to potential settling of crystals. It is stable at room temperature and not light-sensitive, but care must be taken to make sure the bottles are closed securely, as evaporation will increase the concentration of the solution.
Deep Chemical Peels
Deep chemical peels use chemoexfoliants that penetrate from the epidermis to the mid reticular dermis. They effectively resurface deeper periocular rhytids, crepey appearance, crow’s feet, and severe actinic keratosis (Fig. 3.4). The Baker–Gordon formula (Table 3.3) is the often referenced classic deep peel and has given rise to various authors developing modifications of the phenol–croton oil-based formula. The reaction following application of the phenol is characterized by keratocoagulative necrosis of the epidermis extending into the papillary dermis and by a marked inflammatory reaction [14]. The healing process takes place over 8–14 days with post-peel redness continuing up to 2 months [15]. The lasting and restorative effects make phenol peeling ideal for patients seeking improvement of deeper rhytids and creases in the periorbital area.
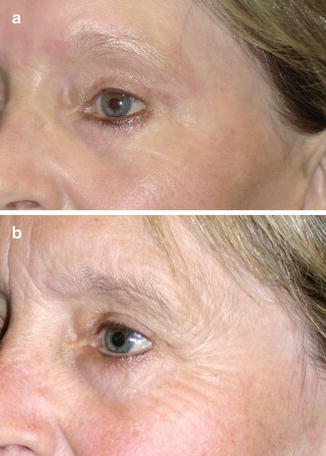
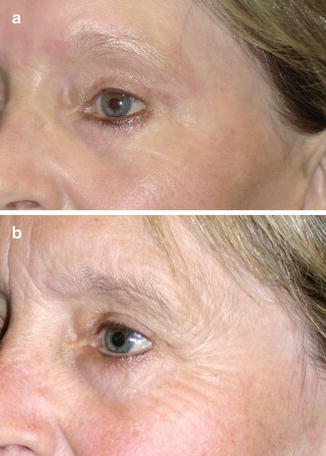
Fig. 3.4
A 70-year-old woman before (a) and after (b) a phenol peel of the periorbital area. She has had a previous blepharoplasty. Note the dramatic resolution of the periorbital rhytids and wrinkles
Table 3.3
The Baker–Gordon formula
|
3 mL 89 % Liquid phenol (USP)
|
|
2 mL Tap water
|
|
Eight drops of liquid soap (Septisol)
|
|
Three drops of croton oil
|
Because of the depth of the wounding of the skin, these peels have a prolonged healing time and higher risk of complications such as hypopigmentation and scarring. Discretion should be used in patients with a history of hepatic, cardiac, and renal disease, as it can affect hepatic and renal function and has reportedly caused suppression of pulmonary function and cardiac activity [16]. Phenol is directly toxic to the myocardium, necessitating the need for full cardiopulmonary monitoring. To minimize these complications, the solution is applied slowly and systematically to individual aesthetic units over a prescribed period of time, while monitoring carefully for cardiac arrhythmias before proceeding to the next subunit. These peels have a considerable learning curve and should be reserved for physicians with a comprehensive understanding of complexity of peels and considerable level of experience with the procedure.
Patient Selection
Indications
Proper patient selection is paramount for successful outcomes. The physician should customize the procedure with the patient’s goals, establish patient compliance, and manage expectations.
Patient assessment begins with the evaluation of skin type, severity of rhytids, amount of redundant skin, degree of laxity of the lower eyelid margin, thickness of the dermal skin around the eyes, actinic damage, and dyschromias. Clarifying the difference between rhytids due to sun damage from that of volume loss and need for a blepharoplasty is necessary for both the patient and physician to recognize.
The Fitzpatrick skin color classification (Table 3.4) is a convenient means in evaluating skin color type and its reaction to sun exposure. Once skin type is identified, the Glogau classification system (Table 3.5), which assesses skin texture, skin thickness, degree of photodamage, and severity of wrinkles, will guide in choosing the appropriate peel. In conjunction with a patient’s medical history and lifestyle, the physician will be able to further tailor the treatment for the patient condition.
Table 3.4
Fitzpatrick classification scale
|
Skin type
|
Skin color
|
Characteristics
|
|---|---|---|
|
I
|
White; very fair, red/blond hair; blue eyes, freckles
|
Always burns, never tans
|
|
II
|
White; very fair, red/blond hair; blue, hazel, or green eyes
|
Usually burns, tans with difficulty
|
|
III
|
Cream white; fair with any hair or eye color; very common
|
Sometimes mild burn, gradually tans
|
|
IV
|
Brown; typical Mediterranean Caucasian skin
|
Rarely burns, tans with ease
|
|
V
|
Dark brown; Middle Eastern skin types
|
Very rarely burns, tans very easily
|
|
VI
|
Black
|
Never burns, tans very easily
|
Table 3.5
The Glogau classification scale
|
Skin class
|
Description
|
|---|---|
|
I
|
Early wrinkles
Age: Twenties to thirties
Early photoaging
Mild pigment changes
Minimal wrinkles
No “age spots”
|
|
II
|
Wrinkles in motion
Age: Thirties to forties
Early to moderate photoaging
Appearance of smile lines
Early brown “age spots”
Early changes in skin texture
|
|
III
|
Wrinkles at rest
Age: Fifties and older
Advanced photoaging
Prominent brown pigmentation
Visible brown “age spots”
Small blood vessels
Wrinkles, even at rest
|
|
IV
|
Only wrinkles
Age: Sixties and older
Severe photoaging
Yellow-gray skin color
Prior skin cancers
Precancerous skin changes (actinic keratosis)
|
Superficial peels are effective for Fitzpatrick skin types I–V and Glogau I patients with mild sun damage and fine wrinkling around the eye area. Sometimes referred to as “refresher” peels, these peels may require repeat treatments to maintain desired results.
The medium-depth peel provides a safe resurfacing modality for moderate photoaging and rhytids (Glogau II) and Fitzpatrick skin types I–IV. Peeling higher Fitzpatrick skin types should be guarded and performed only by experienced practitioners, as Kadhim reports fine and medium periorbital wrinkles responded favorably with medium-depth chemical peels with low and mild adverse effects in dark-skinned individuals [17].
Deeper, coarse rhytids and marked photoaging respond effectively to deeper peels with resultant dramatic and long-lasting effects. The optimum candidate is a Glogau III and IV and a Fitzpatrick I and II and generally not considered for darker skin types due to a high incidence of hypopigmentation.
History
The Patients’ thorough medical and drug history must be throughly evaluated. Relative contraindications for any resurfacing procedure include cutaneous radiation history, active or frequent herpes simplex virus infections, diabetes, hypertrophic scar, or keloid history [18].
Previous history of isotretinoin (Accutane, Roche, Nutley, NJ) usage is a relative contraindication, as the scaring that may result after a peel can be devastating. Isotretinoin prevents post-peel reepithelialization, and a cessation period of 12–24 months is recommended prior to the peel [18].
Birth control pills, exogenous estrogens (soaps, creams, oils), or photosensitizing drugs are to be avoided due to the risk of hyperpigmentation. Because of the level of estrogen in pregnancy, the patient should avoid plans to become pregnant within the first 6 months of the peel [19].
Patients with a history of herpes simplex require antiviral prophylaxis prior to the peel and continued after until re-epithelialization is complete. Antiviral treatment regimens such as valacyclovir (Valtrex, Glaxo Wellcome, West Caldwell, NJ) 500 mg twice a day 2 days prior to the peel, followed by 5 days after the peel, are prescribed. This treatment averts most herpetic breakouts during the post-healing process. Alternative antiviral regimens exist and some physicians advocate prophylactic antivirals to all patients undergoing the peel.
If the patient has had a previous blepharoplasty, or a previous peel, check the ability for the upper lid to completely close. If the upper lid does not fully close, peeling of the upper eyelid is contraindicated due to the potential upper lid tightening, incomplete lid closure, and resultant globe desiccation.
Lifestyle
For a patient to qualify for the peeling procedure, it is essential to examine their lifestyle and habits. They must be reliable to comply with pre- and posttreatment instructions and motivated to care for the area to ensure success of the peel. A prescreening questionnaire reviewing the patient’s daily activities, occupation, and hobbies will identify areas of concern.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








