Fig. 1.1
Dimensions of the ideal face divided into horizontal facial thirds and vertical fifths
Fig. 1.2
The golden ratio and beauty defined following the golden rule: The distance between the oral commissures when smiling should ideally be equal to the interpupillary distance and form a square
Facial Skin
The skin and the subcutaneous tissue over the face has been broadly classified into periorifacial and cervicofacial skin. The periorifacial skin around the eyes, nose, and mouth is thinnest on the face and has little or negligible subcutaneous fat. The muscle fibers in these areas are firmly adherent to the dermis of the skin and therefore clinically manifest as expression lines.
In contrast, the forehead, cheek, and neck are covered with thick skin with abundant subcutaneous fibrofatty tissue. The superficial musculoaponeurotic system (SMAS) is an example of this thicker cervicofacial tissue. Due to the presence of this thicker skin and subcutaneous tissue layer, these cervicofacial regions are less vulnerable to fine lines and wrinkle formation. The subcutaneous tissue and fat in these areas also define the facial framework and topography by softening bony prominences and filling in natural facial contours [8].
The skin in general is composed of the epidermis, dermis, and loose connective tissue with fat. The outermost layer, the epidermis, is composed of four distinct layers—(1) keratinized and impermeable stratum corneum, (2) stratum granulosum, (3) vascular stratum spinosum, and (4) the cellular stratum basal (keratinocytes, melanocytes, fibroblasts) [7]. Although there is great variability in the thickness of the epidermis based on the particular anatomical site, it is on average 100 μm deep. The epidermis receives its nutrition from the highly vascular papillary dermis. Keratinocytes, which are the major cells of the epidermis, contribute to the genetic skin color of the epidermis. Keratin is the major protein that reacts with chemical peel agents, such as trichloroacetic acid (TCA) and phenol, to precipitate and form frost. CO2 laser resurfacing evaporates the epidermis and a portion of dermis using water as a chromophore. If the epidermis and dermis are well hydrated, the results of laser resurfacing are therefore more uniform. Keratinocytes are sensitive to ultraviolet light exposure, which can cause structural damage to their DNA, leading to mutated precancerous cells [9].
The underlying dermis consists mainly of collagen and some elastic fibers (5 %). Approximately 500–1,000 μm thick, the dermis provides structural support to the epidermis and determines the thickness and elasticity of the skin. Dermal regeneration of the epidermis with any form of treatment like dermabrasion, laser resurfacing, or chemical peels depends on the integrity and function of the adnexal structures of the dermis. The dermis is subdivided into the superficial loose vascular layer of connective tissue called the papillary dermis and the deeper reticular layer rich in collagen and elastic fibers. To optimally correct wrinkles and scars with skin rejuvenation procedures, the dermal layer needs to be targeted to the appropriate depth based on the structure to be treated. Vascular lesions like port wine stains and telangiectasis are mainly dermal and can be minimized with dermal treatments. The dermis layer is compact, highly vascular, and also rich in nerve endings. Therefore, penetration of a needle into the dermal layer may meet resistance, be painful, and may cause superficial bruising.
The subcutaneous layer located beneath the dermal layer comprises primarily lobules of fatty tissue. Its thickness and presence of fascial connections are vital to the youthful face and are later important for volumetric analysis in the aging face.
The subcutaneous layer also functions as a buffer for skin trauma, as areas with abundant subcutaneous tissue often heal faster and with less scaring than areas with thin or no subcutaneous tissue. Therefore, deep dermal penetration in areas of the face with almost no subcutaneous tissue, such as the lips, jawline, and neck, should be carefully approached. Dermal thickness in the nasolabial fold is approximately 1.32–1.55 mm. The diameter of the needle used to inject dermal fillers ranges between 0.3 and 0.4 mm with the length of the bevel being approximately 0.75–0.95 mm [10, 11]. Although the technique of using different angles for introduction of the needle into the superficial, mid, or deep dermis is still recommended, these variations with millimetric precision should be observed. The epidermal and dermal layers are thicker in the forehead area than the lower part of the face; thus, large volumes of fillers in the forehead area do not typically yield satisfactory results. In the temporal region where the skin is thin with visible superficial temporal vessels, meticulous injection of dermal fillers with delicate massage may avoid the Tyndall effect (Fig. 1.3) [12, 13].
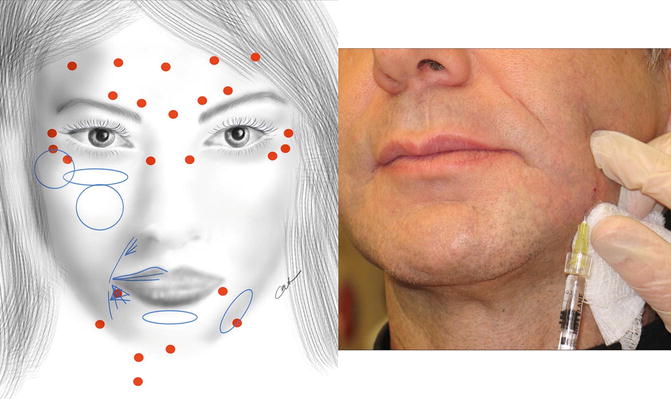
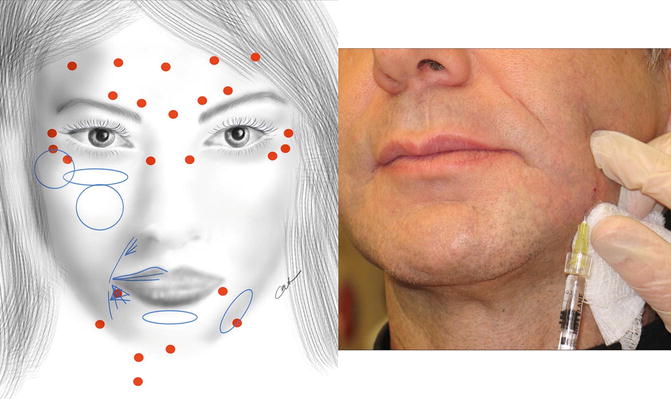
Fig. 1.3
Common sites for facial botox (red) and dermal filler (blue) injections, based on underlying anatomy
Facial Musculature and Soft Tissues
The face comprises the forehead, eyebrows, eyelids, cheek, and lower face subunits that are all closely interrelated. The face is enveloped by the superficial musculoaponeurotic system (SMAS), first described by Mitz and Peyronie [14]. The SMAS is a fibrous fascial tissue, extending from the temporalis and frontalis muscles superiorly to the platysma inferiorly, that interconnects the facial muscles. Intraoperatively, it can be identified as a shiny fibrous layer located between the dermis and deep fascial muscles. Superiorly the SMAS is densely adherent to the zygomatic arch and the temporalis fascia and inferiorly interdigitates with the dermis in the cheek, platysma over the mandible, and the sternomastoid muscle fascia in the neck. The motor branches of the facial nerve lie deep to the SMAS. Because of its bony and soft tissue attachments, the SMAS acts as an important distributor of facial muscular contractions to the skin.
The soft tissues of the face can be considered as layers similar to the scalp—skin, subcutaneous connective tissue, musculoaponeurotic (SMAS), loose areolar tissue and space, and periosteum. The musculoaponeurotic layer, or SMAS, is attached to the dermis of the skin via fine reticular fibers from the subcutaneous tissues and invests the intrinsic muscles of the face. The areolar tissue contains the facial ligaments that are the pillars of attachment between the soft tissue and the bony skeleton. The main ligaments in the cheek region are the orbicularis retaining (orbitomalar), zygomatic, and masseteric ligaments. Free spaces can be found between the ligaments where there is no attachment of the soft tissue to underlying bone, thus creating glide planes that become prominent with aging. The midcheek has compact ligament attachments bonding the large soft tissue area to the underlying bony surface.
It is also important to understand that the lamellar arrangement of facial muscles is crucial to providing firm facial tissue support, as well as influencing the contour and expressions of the face. The most superficial layer consists of the frontalis, orbicularis oculi, zygomaticus minor, and the depressor anguli oris; the second layer comprises the depressor supercilii, zygomaticus major, levator labii superioris, alaeque nasi, depressor labii inferioris, and platysma; and the third layer consists of the levator labii superioris and orbicularis oris. The deepest layer includes the corrugator supercilii, mentalis, levator anguli oris, and buccinator muscles.
In recent years, there has also been more interest in the aesthetic implications of various facial and periocular fat pads. It is understood that the fat structures of the face are crucial in recreating the youthful appearance of the face and need to be restored carefully in specific regions. The topography of these fat structures forms the basis of facial contouring with harvested fat or soft tissue fillers.
The two upper and three lower eyelid fat pads are located posterior to the septum and ideally should not be debulked posteriorly past the orbital rim border in order to avoid the hollow socket appearance (Fig. 1.4). A fat pad posterior to the eyebrow, known as the retroorbicularis oculi fat (ROOF), provides structural support for the eyebrow. When correcting brow ptosis in women, the ROOF should be secured to the periosteum approximately one to two centimeters above the supraorbital rim.
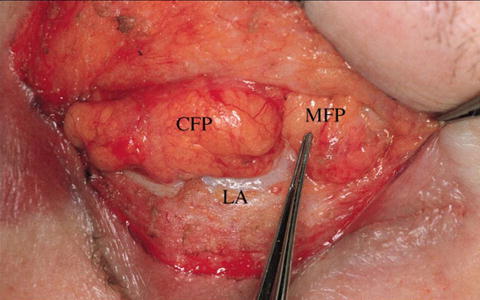
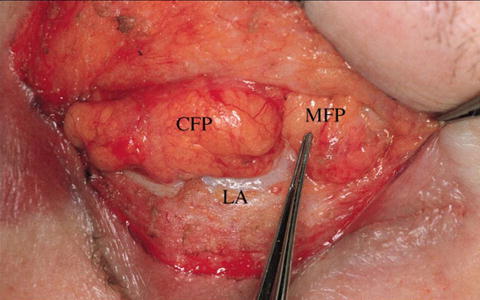
Fig. 1.4
Intraoperative photo of the upper lid fat pads demonstrates a central and medial fat pad (CFP, MFP). There is no lateral fat pad in the upper lid, and lateral fullness would indicate lacrimal gland prolapse
The midface or malar fat lies typically over and medial to the malar eminence of the upper cheek. The location of these structures along with the shape of the face should be considered when planning the injection of fillers aimed at lifting the malar and medial cheek regions (Fig. 1.5). The suborbicularis oculi fat (SOOF) [15] is located beneath the orbicularis oculi plane of the lower lid and is separated from the periorbital fat by the thin orbital and malar septum. Malar fat pads, located below the orbital margin level, can descend with ptosis of the SOOF. The sub-SMAS fat in the malar region is continuous with the submuscular fat in the eyebrow region. The buccal fat lies deep in the face and comprises buccal, temporal, and pterygoid extensions [16].
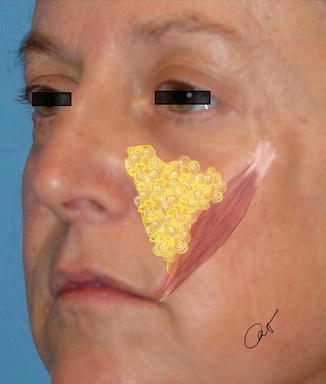
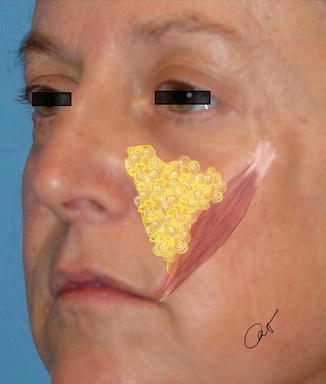
Fig. 1.5
Deep medial cheek fat along the medial border of the zygomaticus major muscle. This is an important anatomical space while injecting dermal fillers and should be augmented properly in order to recreate a youthful anterior projection to the midface and tear trough
Forehead and Glabella
The upper face can be considered as a cosmetic unit that comprises the forehead, glabella, and eyebrows. The forehead runs superiorly from the anterior hairline to the zygoma laterally and the brows inferiorly [17]. The intersection of the forehead frontal bone with the nasal bones caudally on each side of the midline is referred to as the nation. The forehead can also be divided into midline forehead, paramedian forehead, lateral forehead, temporal, and brow regions (Fig. 1.6). There is a gentle smooth rounded convex contour from the midline to the midbrow area that becomes flatter laterally towards the more concave temporal region. The forehead is a multilayered structure that comprises, from anterior to posterior, the skin, subcutaneous connective tissue, muscle, galea aponeurotica, loose areolar tissue and glide space, and periosteum (Fig. 1.7).
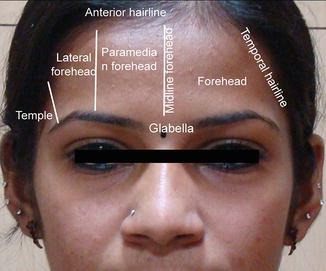
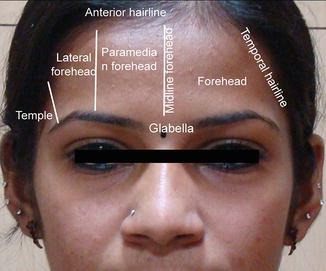
Fig. 1.6
Anatomical divisions of the forehead
Fig. 1.7
Tissue layers of the scalp and face consist of, from anterior to posterior, the skin, cutaneous connective tissue, aponeurosis (including frontalis and SMAS of the face), loose areolar space and glide planes, and periosteum
Facial skin is thickest on the forehead and is relatively inelastic and immobile centrally, although increases in mobility laterally. The galea aponeurotica is a broad musculoaponeurotic layer that is firmly attached to the occipital protuberance posteriorly and fuses with the superficial temporalis fascia laterally which continues with the SMAS in the cheek and neck. The loose areolar tissue posterior to the forehead muscles and galea permit movement of the scalp over the periosteum. The galea aponeurotica divides into a superficial and deep layer to envelope the paired frontalis muscles. The superficial layer covers the anterior frontalis muscle surface, and the deep layer traverses posteriorly to merge along the supraorbital rim into the arcus marginalis and postorbicular fascial plane of the eyelids [18].
The forehead musculature comprises mainly the frontalis muscle. The glabellar muscle complex includes the corrugator supercilii (CSM), depressor supercilii (DSM), and procerus muscles (Fig. 1.8). The superficial group of muscles involved in the formation of glabellar rhytids includes the frontalis, procerus, and orbicularis oculi muscles; the intermediate group includes the depressor supercilii muscles; and the deep group is composed of the corrugator supercilii muscles. Vertical lines of the glabella are caused primarily by the transverse head of the corrugator supercilii muscle. Horizontal rhytids are a result of hyperactive procerus, oblique head of the corrugator, and depressor supercilii muscles; and oblique lines are caused by the transverse head of the corrugator supercilii and the medial orbicularis oculi fibers [19, 20].
Fig. 1.8
Schematic diagram of the anatomical locations and relations of the glabellar and brow musculature (CSM-O corrugator supercilii muscle oblique head, CSM-T corrugator supercilii muscle transverse head, DSM depressor supercilii muscle, F frontalis, OOM orbital orbicularis oculi, P procerus, ZA zygomatic arch)
Frontalis Muscle
The frontalis muscle is the main muscle mass of the forehead and lies beneath the subcutaneous tissue plane. It is the primary elevator of the forehead and eyebrows and is an accessory elevator of the eyelids. Its antagonist muscles are the eyebrow depressor group (Fig. 1.9).


Fig. 1.9
Anatomical overlay of frontalis muscle action. The frontalis muscle is the primary elevator of the forehead and brows (arrows). Muscle contraction leads to formation of deep transverse forehead lines (lines)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








