Pediatric Portal Vein Reconstruction
Shant Shekherdimian
Annie Fecteau
DEFINITION
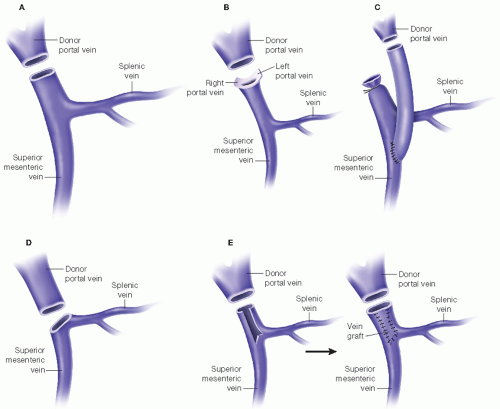
Portal vein (PV) reconstruction is defined as the restoration of blood flow from the recipient portal venous system to the transplanted liver. It is performed after the caval anastomoses and before hepatic arterial and biliary reconstruction. In adults undergoing initial transplantation, this is most often completed using an end-recipient PV to end-donor PV anastomosis. In the pediatric population, significant size discrepancy between the native and donor portal venous system often precludes the use of a primary end-to-end anastomosis. Instead, reconstruction is usually done using one of two methods: the “interposition vein graft” or “branch patch” techniques, with the latter being preferred for smaller recipient PVs. Less common techniques such as portoplasty and primary end-to-end anastomosis (in older children or in size-matched deceased donor transplantations) have also been described (FIG 1).1
IMAGING AND OTHER DIAGNOSTIC STUDIES
Preoperative ultrasonography is sufficient imaging for the purposes of PV reconstruction planning. Specifically, patency of the PV must be confirmed prior to proceeding with a
living related donor transplantation. If there is no flow in the recipient’s PV prior to transplant, an adequate conduit to connect the recipient’s superior mesenteric vein (SMV) to donor’s left PV must be obtained. Furthermore, because recipient PV size is a strong risk factor for PV complications,2,3 some centers use information from preoperative ultrasonography to assist with deciding on the type of reconstruction. Specific sonographic parameters that may facilitate decision making with respect to PV reconstruction include PV diameter, portal flow direction, and hepatic arterial resistance index.4 Computed tomography (CT) scan or magnetic resonance imaging (MRI) can also inform this preoperative planning and are critical in the setting of mesenteric venous occlusive disease.
SURGICAL MANAGEMENT
Assess the diameter and the length of recipient PV, the presence and degree of sclerosis, and the donor PV. Decide to use a branch patch or interposition vein graft (also referred to as a “jump graft”) based on these intraoperative findings. Table 1 lists the common indications for using an interposition vein graft.
Use the branch patch technique in primary transplant patients with small PV size and good length receiving a large donor liver PV. This technique takes advantage of the wide diameter of the recipient PV at the level of left and right PV confluence to create an anastomosis with the larger donor PV. Less frequently, fashion an anastomosis between the SMV-splenic vein confluence and the donor PV.
Table 1: Indications for Use of Interposition Vein Graft
Indication
Example
Small, <5 mm recipient PV with low flow
Patients under 5 kg
Inadequate recipient PV length
Redo transplantation
Sclerotic/hypoplastic PV with low flow
Biliary atresia
Large PV size mismatch
Living donor
PV, portal vein.
In the interposition vein graft technique, fashion an extraanatomic vein segment to restore portal blood flow to the donor PV. Sew the proximal vein segment of the vein graft to the SMV in an end-to-side fashion. The vein graft can also be sewn to the proximal PV or the confluence of the SMV-splenic vein. In deceased donor transplants, donor iliac vein may be used, whereas with living donor transplants, inferior mesenteric vein, gonadal vein, and internal jugular vein interposition grafts may be procured from the donor.
TECHNIQUES
PREPARATION OF RECIPIENT PORTAL VEIN
Mobilize the PV and decide on the type of PV reconstruction (branch patch, primary, or interposition graft). If an interposition graft is to be used, a suitable segment of infracolic SMV is identified and isolated. Immediately prior to beginning the anastomosis, remove the proximal clamp and confirm flow. Instill the vessel with heparinized saline to maintain patency.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree