41 Pediatric chest and trunk defects
Synopsis
 Pediatric trunk defects require multidisciplinary comprehensive care in order to maximize patient safety and successful outcome.
Pediatric trunk defects require multidisciplinary comprehensive care in order to maximize patient safety and successful outcome.
 Reconstructive surgery for the pediatric patient requires consideration for the paucity of tissue available in a small body habitus, the necessity for growth, and the tenuous physiology that may accompany children afflicted with congenital defects.
Reconstructive surgery for the pediatric patient requires consideration for the paucity of tissue available in a small body habitus, the necessity for growth, and the tenuous physiology that may accompany children afflicted with congenital defects.
 Closure of ventral body wall defects may pose significant challenges to the neonatal circulation whereas closure of dorsal body wall defects must address exposed neural elements.
Closure of ventral body wall defects may pose significant challenges to the neonatal circulation whereas closure of dorsal body wall defects must address exposed neural elements.
Embryology
Development of the body wall begins at the fourth week of gestation when the mesoderm organizes into the paraxial, intermediate, and lateral plate layers. The paraxial mesoderm, adjacent to the neural tube, differentiates into the skeletal support and surrounding soft tissue that characterize the dorsal body wall and encase the central nervous system. Intermediate mesoderm forms the urogenital structures. Lateral plate mesoderm differentiates into both the soft-tissue and skeletal components of the ventral body wall. The lateral plate mesoderm, with ectoderm covering, folds and fuses at the end of the fourth week of gestation.1,2 Congenital ventral body wall defects result from the lack of lateral plate fusion.
Thoracic wall defects
Pectus excavatum
Clinical presentation and evaluation
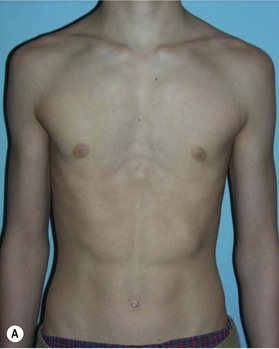
Patients with pectus excavatum exhibit a depressed sternum that is frequently greater on the right with sternal retraction on inspiration.3,4 Both the body of the sternum and the costal cartilages at the sternocostal junction have posterior angulation (Fig. 41.1). Rounded sloping shoulders, mild dorsal kyphosis, and a protuberant abdomen are associated findings but may be related to postural changes that patients exhibit secondary to a conscious or subconscious attempt to hide their deformity.
Proper identification of the extent of structural irregularity, physiologic limitations, and psychological responses to the deformity are crucial in treatment decision-making. Basic workup should include chest radiographs, pulmonary function tests, electrocardiogram, and chest computed tomography (CT) scan (Fig. 41.2). Haller and others stratified anatomic severity of pectus excavatum by defining the pectus severity index (PSI) using measurements obtained from CT scans.5,6 The PSI is calculated by dividing the internal transverse thoracic width by the smallest anterior–posterior distance between the vertebrae and the most depressed portion of the chest wall. Normal values range between 2.5 and 3.25. Operative intervention usually occurs with PSI values greater than 4.8.7
Surgical indications
Most patients are asymptomatic and seek elective intervention for the correction of contour deformities, especially when the features become more prominent during the pubertal growth spurt. Although cardiopulmonary compromise is controversial, anatomically severe versions of pectus excavatum are thought to benefit from surgical intervention.8,9 Kelly suggests that surgery is indicated when two or more of the following occur: a severe, symptomatic deformity; progression of deformity; paradoxical respiratory chest wall motion; CT scan with a PSI greater than 3.25; cardiac or pulmonary compression or pathology; significant body image disturbance; or failed repairs.10 Surgical correction is considered safe in children older than 7 years of age; however, timing has been a subject of controversy.
Treatment
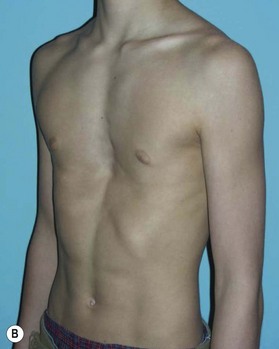
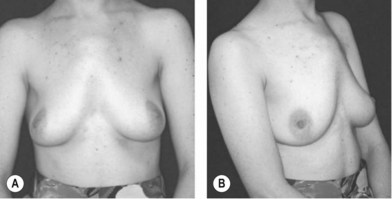
Some patients with mild deformities can be satisfactorily treated with physical therapy to improve their posture and increase the bulk of their pectoralis muscles. Surgical correction of pectus excavatum can be categorized into contour camouflage and contour repair procedures. Camouflage of the contour deformities has been successfully accomplished with autologous tissue or custom prosthetics. The disadvantage of autologous tissue is the donor site scar and potential morbidity. Flaps containing muscle should not be relied on for volume correction only unless innervated and able to contract, as the muscle will invariably atrophy if not innervated and contracting. The most common contour camouflage technique is placement of customized silicone implants11–14 (Fig. 41.3). Satisfactory results are obtained with silicone implants with few short-term complications other than seroma formation. Additional problems with prosthetics are displacement and visualization of edges, especially in thin patients. Autologous reconstruction has been used as an alternative to prosthetics in selected patients.15–18 Recently, Sinna et al. described a combination of approaches covering a custom implant with bilateral de-epithelialized thoracodorsal artery perforator flaps.19 Injection of autologous fat or prosthetic soft-tissue fillers has also been described.20,21
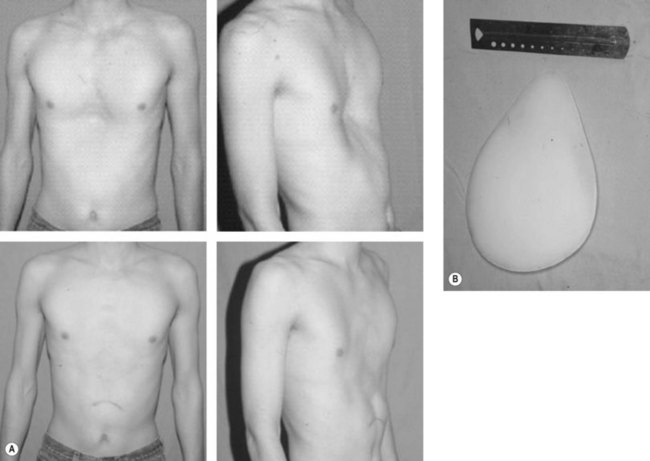
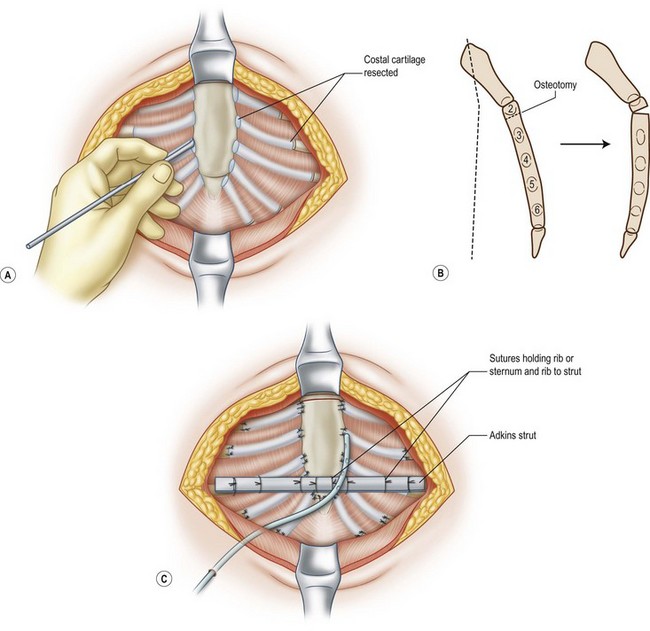
Whereas contour camouflage techniques are most appropriate for patients with mild deformities, patients with moderate to severe deformities are better suited for contour repair techniques. Ravitch described an open repair technique of elevating bilateral pectoralis muscle flaps with resection of abnormal costal cartilages followed by transverse osteotomy of the sternum and fixation in a corrected position4 (Fig. 41.4). Since his report, the Ravitch procedure has been modified in many ways: from preserving the perichondrium to minimal cartilage resection and varying technique to support the sternum.22,23 Haller and colleagues describe supporting the elevated sternum by overlapping the sternal ends of the costal cartilages over the costal ends in a tripod fixation.24,25 Almost all open techniques utilize a transverse inframammary crease or a short chevron incision, except for older patients or Marfan patients where a vertical midline incision is usually used. Bilateral pectoralis major and upper rectus abdominis muscles are disinserted from the sternum and ribs bilaterally and raised to expose the costal cartilages. With or without sacrifice of the perichondrium, the costal cartilages are resected to a greater or lesser degree. Since Ravitch’s initial experience, it has become clear that the most medial and most lateral portions of the costal cartilages should be preserved in young children to minimize secondary growth disturbances. The sternal angulation is corrected with a transverse wedge osteotomy that is done at the level of the third or fourth intercostal space corresponding to the upper edge of the sternal depression. The osteotomy can then be secured with sutures, wire, or rigid fixation plates.26,27 The xiphoid process is detached from the sternum and allowed to retract down.
Horizontal sternal fixation techniques are not universally used but are considered by many to be important for sternal support. Many surgeons have supported the sternum with a metallic strut developed by Adkins and Blades.28 Fonkalsrud and colleagues report on a modified open technique with minimal cartilage resection and use of the Adkins strut in 450 patients.29 Most of these patients had retrosternal placement but more recently they have converted to a suprasternal strut to facilitate removal (at 6 months) and minimize the need to enter the pleural cavity. Hayashi and Maruyama describe the use of a vascularized rib strut based on the anterior intercostal branch of the internal mammary artery instead of a metallic strut.30 Robicsek et al. have extensive experience reporting on over 600 patients treated with a retrosternal Marlex mesh “hammock” technique with excellent long-term results.31 Recently, bioabsorbable mesh placed for retrosternal support in the Robicsek technique has been reported and found to be associated with decreased inflammatory reaction, decreased postoperative pain, and elimination of the risk of retrosternal metal support device dislodgment.32
A radical method to repair contour deformities of the sternum uses a sternal turnover bone graft.33 This technique has been met with problems of sternal avascular necrosis due to the interruption of blood supply. Vascularized sternal turnover bone flaps with microvascular anastomoses of the internal mammary vessels were later developed to prevent such complications and have been successful in several reports.34–36
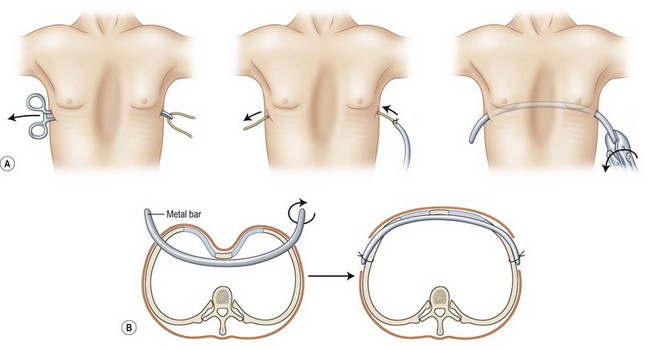
With the development and advances in thoracoscopy, minimally invasive repair of pectus excavatum (MIRPE) has emerged as a viable option.37,38 MIRPE, also called the Nuss procedure, involves a thoracoscopic exposure of the sternum and the placement of a bent bar (Fig. 41.5). Unlike the Ravitch and modified Ravitch procedures, skeletal resection is avoided and the operative time is significantly shorter. However, complications such as bar dislocation, bar extrusion, and costal erosion have been reported.39 In addition, a second procedure to remove the bar is required. Absorbable transsternal bars have been used in the Nuss procedure but they are associated with higher breakage rates.40
The immediate complications of pectus excavatum contour repair are rare beyond pneumothorax and wound infection. Especially in the Ravitch procedure without rigid fixation, recurrence can occur as a late complication. Secondary thoracic deformity is a serious late complication that has been observed in patients who undergo correction at an early age. Thought to be due to the interruption of growth centers and intrathoracic scar formation, the patients develop narrowed thoraces and severe pulmonary impairment. Haller et al. coined this phenomenon as acquired Jeune’s syndrome.41
Pectus carinatum
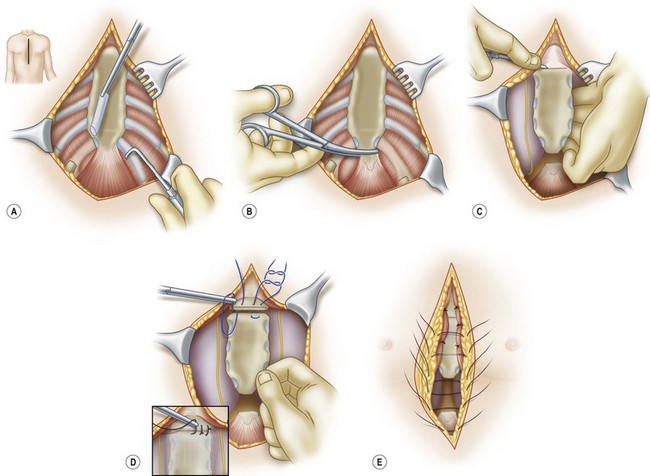
Pectus carinatum, although less common in presentation compared to pectus excavatum, is considered to be in the same spectrum of deformities. It is characterized as a protrusion deformity of the anterior thoracic wall (Fig. 41.6). Similar to pectus excavatum, pectus carinatum does not have a defined etiology. The incidence is between 1 in 10 000 and 1 in 1000 live births and is six times more common in males.
Clinical presentation and surgical indications
Three types of anterior thoracic protrusion deformities have been described in the pectus carinatum spectrum.42 The chondrogladiolar type is the most common version and is characterized by anterior displacement of the body of the sternum with costal cartilage concavity. Asymmetric mixed deformities can also occur with displacement of the costal cartilages on one side with normal positioning of the sternum. Prominence of the chondromanubrial junction with a depressed sternum represents the third and least common type. Unlike pectus excavatum, younger patients do not have cardiopulmonary compromise and tend to display subtle findings on clinical exam. Patients tend to be diagnosed at a later age and seek surgical correction for their contour irregularities. Pectus carinatum can also be an acquired defect secondary to pectus excavatum repair.43
Treatment
Skin incisions for pectus carinatum reconstruction are usually transverse inframammary fold incisions. Classically, the pectoralis and rectus muscles are elevated to expose the costal cartilages and the sternum. For the chondrogladiolar deformity, subperichondrial resection of the costal cartilages is combined with a single or double osteotomy to return the sternum to the correct alignment42 (Fig. 41.7). For the asymmetric deformities, sternal positioning is corrected after costal cartilage resection with a wedge osteotomy. Recent refinements in this procedure include a method in which costal cartilages are resected through splitting the muscle along its fibers rather than elevating the entire muscle.44 Nonsurgical means of correction using orthotics have been described in small case series with subjective improvement of carinatum.45 However, the results do not have long-term follow-up and it is not clear that young patients can tolerate wearing a brace for extended periods of time.
Jeune’s syndrome
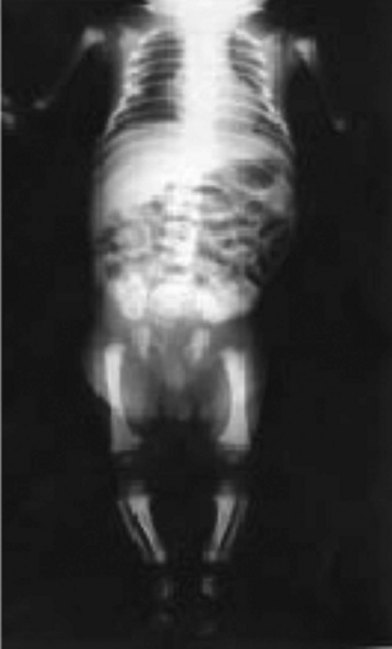
Asphyxiating thoracic dystrophy, Jeune’s syndrome, is a rare familial autosomal-recessive osteochondrodystrophy characterized by a narrow, immobile thorax and a protuberant abdomen46 (Fig. 41.8). Though the early descriptions were in neonates who succumbed to respiratory insufficiency, subsequent reports have demonstrated that Jeune’s syndrome has a variable expression and may result in viability.47 In patients who have less severe versions of Jeune’s syndrome, renal failure occurs in adulthood.
Clinical presentation and surgical indications
Jeune’s syndrome can be variably expressed.48 The neonate with severe Jeune’s syndrome is generally described as having a narrow, bell-shaped thorax that is narrowed in both the transverse and sagittal dimensions with mild brachydactyly. The ribs are short, wide, and barely reach the anterior axillary line. Histologic examination of the costochondral junction reveals disordered endochondral ossification. These patients have severe restrictive lung disease and frequently require mechanical ventilation. In contrast, patients who have a moderate expression of Jeune’s syndrome tend to have a narrow thorax without respiratory compromise, severe brachydactyly, and renal failure at a later age. These patients are usually identified upon presentation for renal transplantation or renal replacement therapy. Finally, the mildest form of Jeune’s syndrome may be manifested with only polydactyly and severe brachydactyly. Surgical correction is indicated in those patients undergoing respiratory compromise.
Treatment
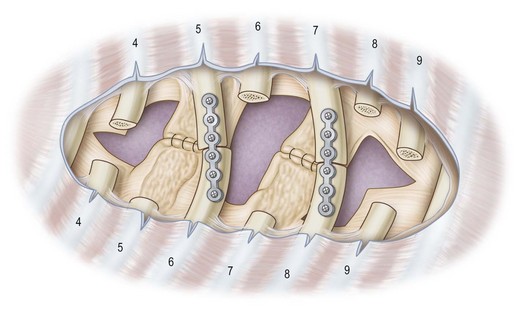
Operative intervention in Jeune’s syndrome is focused on expansion of the thoracic cavity. Two methods have emerged as successful options: median sternotomy and lateral thoracic expansion thoracoplasty. The median sternotomy technique usually requires addition of bone graft, stainless steel struts, or prosthetic spacers.49–52 Alternatively, Davis and colleagues described a lateral thoracic expansion technique (Fig. 41.9). In this procedure, ribs 4 through 9 are differentially transected, separated from periosteum, and different ribs are secured together in an expanded fashion with titanium plates.53–55 The authors noted excellent results in patients over 1 year of age and new bone formation with this method. Waldhausen and colleagues report success with a technique using a vertical expandable prosthetic titanium rib thoracoplasty for the treatment of children with thoracic insufficiency syndrome. Two patients in their series had Jeune’s syndrome.56
Ectopia cordis
Ectopia cordis represents a spectrum of four rare congenital deformities uniformly characterized by a midline sternal defect. The incidence of ectopia cordis is 0.8 per 100 000 live births and can vary from asymptomatic benign clefts to severe conditions with high mortality rates. Many cases can be diagnosed by prenatal ultrasound (Fig. 41.10).
Clinical presentation and surgical indications
Multiple investigators have provided anatomic classifications of ectopia cordis. Cervical ectopia cordis is the most severe version with superior displacement of the heart and craniofacial deformities. Thoracic ectopia cordis describes the classic extrathoracic heart without soft tissue or bony covering. Thoracoabdominal ectopia cordis is a combination of both thoracic wall and abdominal wall defects (Fig. 41.11). These defects are associated with Cantrell’s pentalogy, which includes a midline supraumbilical defect, low sternal defect, anterior diaphragmatic defect, pericardial defect, and intracardiac anomalies.57 Finally, bifid sternum is a relatively benign finding with a cleft upper sternum that rarely causes significant physiologic disturbance (Fig. 41.12). Surgical correction is necessary in thoracic, thoracoabdominal, and cervical ectopia cordis with the initial goal of coverage of the heart followed by ultimately returning the heart to the thoracic cavity when patients have developed sufficient reserve. Coordinated multidisciplinary care involving obstetricians, neonatologists, critical care anesthesiologists, cardiothoracic surgeons, and plastic surgeons is critical to reduce mortality in these high-risk neonates.

Fig. 41.11 Thoracoabdominal ectopia cordis. Same patient as Figure 41.10 with ectopia cordis, midline supraumbilical defect, and low sternal defect.
Treatment
Thoracic and thoracoabdominal ectopia cordis repair is most successful when performed in a staged manner. The first step is performed within the first several hours of life and involves coverage of the exposed heart with bilateral pectoral skin flaps, split-thickness skin grafts, or synthetic or biologic mesh. There should be no attempt at returning the heart to the thoracic cavity at this point due to the cardiopulmonary compromise that will occur with compression.58 At several months to 2 years of age, the patient receives chest wall reconstruction and repositioning of the heart. Chest wall reconstruction can take the form of musculocutaneous flaps over autologous rib grafts as well as alloplastic custom-made struts.59,60 Hochberg and colleagues59 described a method of elevating the pectoral and rectus muscles as a unit and transposing bipedicled musculocutaneous flaps medially with relaxing incisions laterally. The resulting donor sites were skin-grafted on the lateral aspects of the patient. Outcomes for cervical, thoracic, and thoracoabdominal ectopia cordis are poor. Most patients do not survive beyond the perioperative period.
Sternal clefts without an exposed heart are significantly less complicated. Surgical repair is usually performed within the first month of life. Bilateral pectoralis major muscle advancement flaps over rib grafts have yielded good cosmetic results.61 Rigid fixation with titanium plates also has been reported.62
Poland’s syndrome
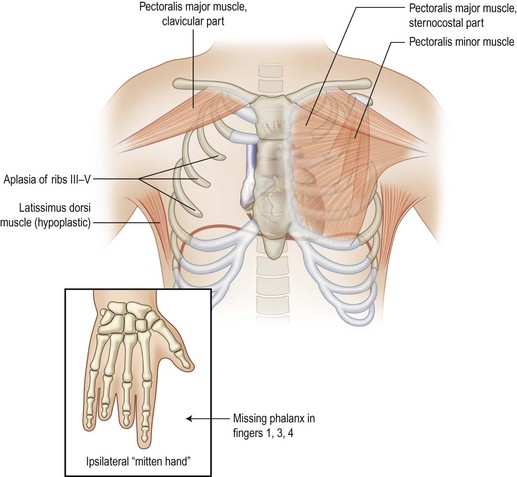
Poland’s syndrome is a rare disorder that is characterized by the unilateral absence of the sternal head of the pectoralis major muscle, breast hypoplasia or aplasia, absent or deformed ribs, axillary alopecia, and ipsilateral upper extremity shortening and brachysyndactyly.63,64 Poland’s syndrome has been reported to have an incidence around 1 to 30 000 live births, with males outnumbering females.65 The etiology is unknown. One suggested mechanism for Poland’s syndrome is subclavian artery insufficiency occurring around the sixth week of gestation with the right side affected twice as often as the left. Alternatively, unilateral developmental failure of the lateral plate mesoderm has also been proposed.
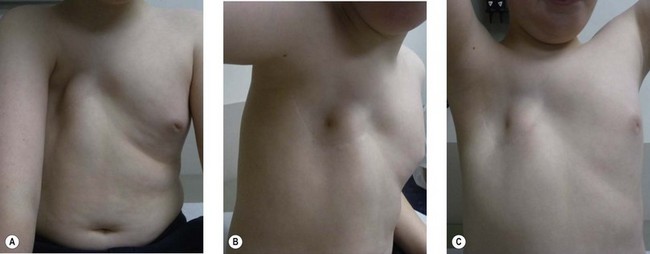
Clinical presentation and surgical indications
Pediatric patients with Poland’s syndrome are heterogeneous. The pathognomonic feature is the absence of the sternal head of the pectoralis major muscle with anterior axillary fold deficiency (Fig. 41.13). Varying degrees of chest wall and hand involvement may occur (Fig. 41.14). In rare severe circumstances, depression deformities can occur with attenuation of ribs 2–5 with absence of anterior cartilage leading to paradoxical motion of the chest wall or lung herniation Some patients have a carinate deformity on the contralateral side. In one-third of patients, the breast is affected and can range from hypoplasia to complete absence. The latissimus dorsi muscle may be attenuated. Diagnosis of Poland’s syndrome is possible by prenatal ultrasound but is usually best evaluated with postnatal physical exam.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree