Chapter 30 Outcomes of the Modified Paneva-Holevich Procedures and Early Postoperative Mobilization
Outline
In 1965, Paneva-Holevich suggested the use of pedicled flexor digitorum superficialis (FDS) tendon as a graft by creating a loop of the flexor digitorum profundus (FDP) and flexor digitorum superficialis (FDS) then reflecting the latter in the second stage as a pedicled tendon graft.1,2 In 1971, Hunter and Salisbury introduced the concept of using a silicone-Dacron reinforced tendon rod to stimulate formation of a new tendon sheath before tendon grafting.3 This transforms the scarred tendon bed into a gliding pliable functional system. In 1972, Kessler reported on the combined use of Hunter rod and pedicled FDS for staged flexor tendon reconstruction.4 Since then, several reports of the combined method have been published.5–9
We started performing this procedure in 1983. In 1997, we published our experience with the use of this technique in 33 patients.8 Up to 2009, we applied this technique in 116 patients. Candidates for this type of tendon reconstruction included patients who did not have their flexor tendon repaired or those who had their repairs failed secondary to rupture or adhesions (Figure 30-1). Most of these procedures are performed in patients with zone 2 flexor tendon injuries. However, zone 1 injuries are also amenable to this type of reconstruction. Zone 3 and 4 injures can usually be treated with conventional single-stage interposition tendon grafts unless there is a concomitant damage to the flexor tendon sheath in zone 2. This procedure is particularly useful in tendon injuries associated with severe crushing injuries when there are associated fractures, nerve injuries, and skin defects.5,7,8
This technique has become our standard technique for flexor tendon reconstruction when the tendon bed does not allow one-stage flexor tendon grafting. A distinct advantage of this procedure is to allow earlier active range of motion (AROM), since the proximal repair should be completely healed by the time the second stage is performed if a tendon graft, instead of tendon transfer, is used. A strong distal repair, preferably attaching the tendon to the bony distal phalanx, would allow the graft to withstand the forces of early AROM without fears of rupture. Actually, Paneva-Holevich recommended starting active motion of the involved digit in the first postoperative week and reported no increase in the incidence of rupture in her early report of secondary reconstruction of the FDP tendon by FDS transfer from the same finger.7
Surgical Technique
Stage 1
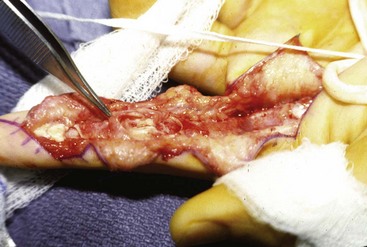
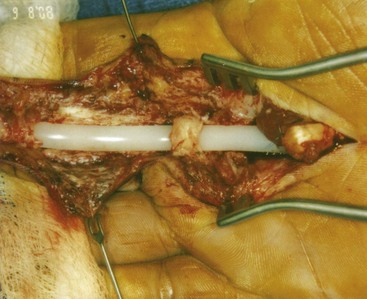
Through a Bruner zigzag incision, the flexor tendon sheath is exposed. The remnants of the flexor tendons are excised (Figures 30-2 to 30-4). Special care should be taken to preserve all the normal pulleys as much as possible. If the important pulleys or majority of the flexor pulley system are destroyed, pulley reconstruction should be performed at this stage utilizing pieces of the excised flexor tendons. Any nerve grafting or flexion contracture release can be done at this stage. The largest possible Hunter rod is then inserted. The Hunter rod should not touch the gloves as this may produce inflammatory reaction secondary to the contact with the talc powder. The distal end of the rod is sutured to the distal stump of the FDP with horizontal mattress sutures of 4-0 Prolene or 4-0 fiberwire. It is important to be sure that the sutures include the Dacron tape within the Hunter rod since the silicone alone has very little holding power. The proximal stump of the rod is left free in the palm. The FDS and FDP tendons of the injured finger are exposed at the mid palm level. Their ends are freshened to healthy margins and then sutured to each other with an end-to-end method (Figures 30-5 and 30-6).

Figure 30-3 The FDS and FDP tendons are seen at the base of the finger. Note the scarring of the flexor tendon sheath.
Patients are started on passive range of motion (PROM) of the operated digits 3 to 5 days postoperatively, which lasts as long as required to ensure adequate passive range of finger motion. PROM is performed to keep the joints flexible. The patient is instructed to perform PROM of each joint of the involved digit for 10 repetitions 6 to 8 times a day. Unrestricted active motion exercises of the uninvolved digits are emphasized as well (Box 30-1).
Box 30-1 Clinical Pearls—Stage 1
 Flexor tendon remnants are excised.
Flexor tendon remnants are excised.
 Pulleys are preserved or reconstructed using the excised flexor tendons.
Pulleys are preserved or reconstructed using the excised flexor tendons.
 The proximal ends of the FDS and FDP are repaired end-to-end in the palm.
The proximal ends of the FDS and FDP are repaired end-to-end in the palm.
 Leave the Prolene suture long to facilitate identification in stage 2.
Leave the Prolene suture long to facilitate identification in stage 2.
 The largest possible Hunter rod is inserted. The distal end is repaired to the FDP stump and the proximal end is left free in the palm.
The largest possible Hunter rod is inserted. The distal end is repaired to the FDP stump and the proximal end is left free in the palm.
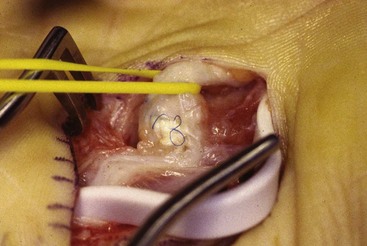
Stage 2
We recommend allowing at least 12 weeks before proceeding with the second stage. The scar should be supple. Excellent PROM is a prerequisite before proceeding to stage 2. Through a zigzag incision in the palm, the site of FDS-to-FDP tenorrhaphy in the palm is exposed and freed of the scar tissue (Figure 30-7). A zigzag incision is made over the distal forearm and the FDS tendon of the involved digit is isolated. The tendon is divided at the musculotendinous junction and then retrieved in the palm incision as a pedicled graft (Figures 30-8 and 30-9). The Hunter rod is exposed and the new sheath is opened at its proximal end in the palm.