27 Orthodontics in cleft lip and palate management
Synopsis
 Patients with oro-facial clefts are best treated through a team approach.
Patients with oro-facial clefts are best treated through a team approach.
 Close collaboration between the orthodontist and surgeon is critical during the care of patients with oro-facial clefts.
Close collaboration between the orthodontist and surgeon is critical during the care of patients with oro-facial clefts.
 A developmental approach needs to be undertaken by orthodontists treating patients with oro-facial clefts.
A developmental approach needs to be undertaken by orthodontists treating patients with oro-facial clefts.
 In infancy the orthodontist can support the surgeon with nasoalveolar molding and maxillary orthopedics.
In infancy the orthodontist can support the surgeon with nasoalveolar molding and maxillary orthopedics.
 In the primary dentition stage the orthodontist can correct mild to moderate posterior and anterior crossbites.
In the primary dentition stage the orthodontist can correct mild to moderate posterior and anterior crossbites.
 In the transitional dentition the orthodontist prepares the maxillary arch prior to bone grafting and premaxillary repositioning.
In the transitional dentition the orthodontist prepares the maxillary arch prior to bone grafting and premaxillary repositioning.
 In the full permanent dentition the orthodontists finalizes arch alignment and coordination.
In the full permanent dentition the orthodontists finalizes arch alignment and coordination.
 The orthodontists supports the surgeon during planning, preparation of appliances and follow up of patients requiring orthognathic surgery and/or distraction osteogenesis during adolescence.
The orthodontists supports the surgeon during planning, preparation of appliances and follow up of patients requiring orthognathic surgery and/or distraction osteogenesis during adolescence.
 The orthodontist works closely with other specialists in pediatric dentistry, prosthodontics, oral and plastic surgery to rehabilitate the dental, oral and facial conditions of patients with oro-facial clefts.
The orthodontist works closely with other specialists in pediatric dentistry, prosthodontics, oral and plastic surgery to rehabilitate the dental, oral and facial conditions of patients with oro-facial clefts.
 The application of new orthodontic diagnostic and treatment modalities to patients with oro-facial clefts is likely to improve treatment outcomes.
The application of new orthodontic diagnostic and treatment modalities to patients with oro-facial clefts is likely to improve treatment outcomes.
Introduction
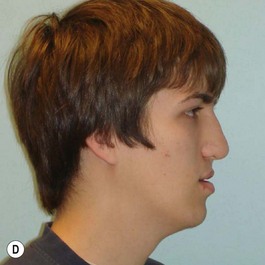
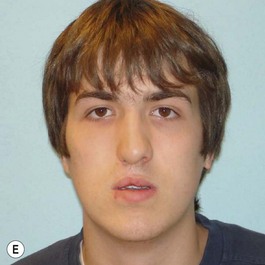
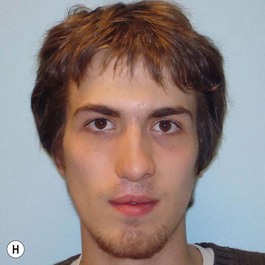
It is our experience that patients treated within the context of the multidisciplinary approach can obtain excellent outcomes related to speech, ideal occlusion, satisfactory lip aesthetics, and skeletal balance (Fig. 27.1). However, it is the secondary cleft nasal deformity that still gives the patient the “cleft stigmata.”
In this chapter, some of the new orthodontic and surgical strategies that are of benefit to cleft patients will be presented. The reader is directed to previous publications that deal with the role of the orthodontist in the management of the cleft patient to complement the information presented in this chapter.1–4
Infancy
On many occasions, the surgeon is faced with an infant who has a severe cleft with marked distortions of not only the maxillary segments but also the cartilages of the nose. This situation can occur in both the unilateral and bilateral cleft lip and palate patient. Since 1995 we have introduced the use of nasoalveolar molding in the treatment protocol of those patients presenting with unilateral and bilateral clefts with premaxillary protrusion and hypoplastic columella with moderate to severe nasal distortions, following the general principles reported by Grayson and associates.5–10 They utilize premaxillary and maxillary orthopedics with the additional purposes of not only aligning the maxillary and premaxillary segments, but also to reposition the nasal cartilages prior to lip repair.
Unilateral cleft lip
Evaluation of the cleft nose demonstrates the presence of severely distorted nasal cartilage with deviation of the nasal tip towards the noncleft side and severe angulation of the columella also to the noncleft side. In addition, we have observed that the soft tissues caudal to the lateral nasal cartilage may be hyperplastic and prominent. Repair of the lip under these conditions, even with surgical repositioning of the nasal cartilages, results in a suboptimal nasal morphology outcome, even though the lip repair is satisfactory. It is for this reason that we have now embarked on the process of orthopedic repositioning of the nasal cartilages, columella, nasal tip, and lateral wall of the vestibule in order to provide these patients with the best possible primary nasal reconstruction with minimally invasive surgical techniques. The procedure of presurgical infant nasal remodeling utilizing a modified intraoral plate was first described by Bennun and co-workers in Argentina.11,12 Since then, it has been popularized in the US as nasoalveolar molding by Grayson et al.5–10 The authors have used this technique since 1995 and have made some modifications.13
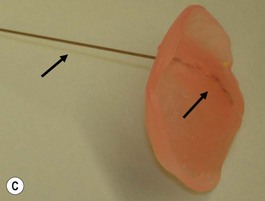
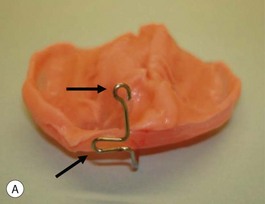
Our technique is as follows: the nasoalveolar molding plate is made utilizing a light cure orthodontic resin. A loop wire is incorporated to support the nasal conformer (nasal stent), made of light cured acrylic, to reposition the nasal structures. The nasal stent is covered with soft acrylic to avoid irritation of the delicate tissues of the nasal mucosa. The palatal aspect of the plate is covered with soft-tissue liner in order to obtain perfect adaptation to the maxillary palatal shelves and undercuts created by the cleft (Figs 27.2 and 27.3). An exact fit of the plate is required for adequate retention, especially since we do not rely on external adhesive tape to maintain the plate in position. We utilize denture adhesive cream, after drying the plate and the oral mucosa prior to insertion. The parents are instructed to clean and replace the denture adhesive one to two times per day. Patients return on a weekly basis for adjustments to increase the length of the supporting wire and reshape the nasal stent. While the nasal molding is taking place, selectively grinding acrylic medial to the palatal shelves and adding acrylic lateral to the alveolar processes narrows the distance between the maxillary segments (Fig. 27.4). In addition, facial taping can be utilized to apply transverse pressure to the cleft segments and help with the cleft narrowing and nasal molding process (Fig. 27.5).
The results expected from this technique include repositioning of the nasal tip towards the noncleft side with straightening of the columella and equalizing the height on the nasal domes as much as possible. In addition, the nasal stent is adjusted in such a way as to exert lateral pressure on the lateral nasal wall against the hyperplastic soft tissues caudal to the lateral nasal cartilage (Fig. 27.5). This results in a straighter nose with convex nasal cartilages and flattened hyperplastic lateral wall vestibular tissues.
In cases that start with severe nasal distortion, we support the nasal molding with postsurgical nasal stents utilizing commercially available removable nasal stents.13–15 The stent is usually kept in place using facial taping (Fig. 27.6) and is maintained for at least 2–3 months or for as long as the patient can deal with it comfortably.
Bilateral cleft lip
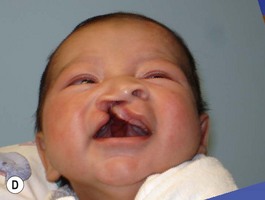
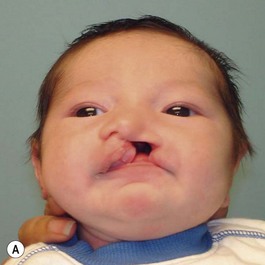
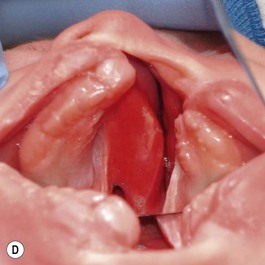
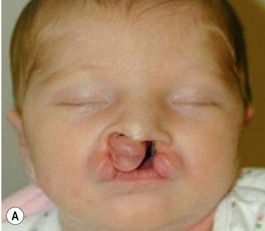
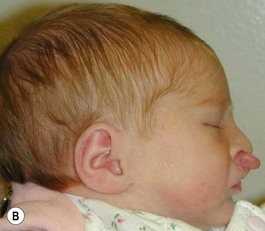
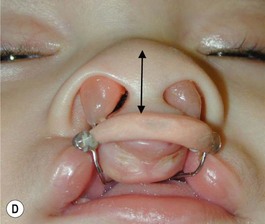
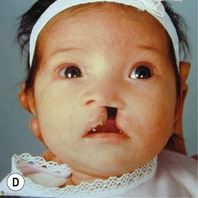
The patient with bilateral cleft lip and palate represents the most challenging condition for the reconstructive team. The premaxilla is extremely protrusive, the premaxilla and prolabium can be of variable size, the columella is deficient or almost nonexistent, the palatal clefts are wider than usual, and occasionally, the maxillary palatal shelves are collapsed. In addition, the nasal domes are wide apart and the tip projection is decreased (Fig. 27.7). It has been our experience that, in patients with bilateral cleft lip and palate, with a protrusive premaxilla, it becomes imperative that the premaxilla is repositioned into a more favorable relation with the maxillary segments in order to achieve definitive lip closure with minimal tension. If this is not done, a poor repair or failure with unfavorable consequences may occur. For this purpose, we have successfully utilized premaxillary orthopedics with an intraoral appliance that is retained with denture adhesive and has an elastic strap for premaxillary retraction.16,17 This approach has allowed the surgeon to close the lip satisfactorily (Figs 27.8 and 27.9).
In the bilateral cleft lip and palate patient the approach requires repositioning of the premaxilla prior to the nasal molding technique. For the last 20 years we have used a self-retaining intraoral plate17 that has been modified from the original design.16 This modification allows for easy adjustments and fewer frequent patient visits.
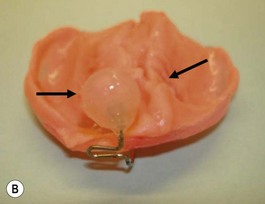
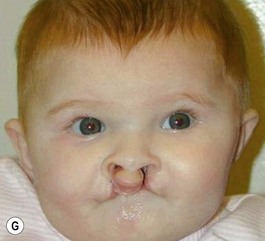
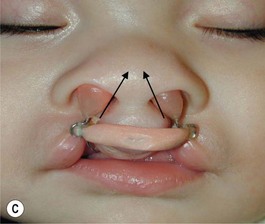
Grayson and coworkers6–8,10 have utilized nasoalveolar molding for bilateral clefts. The appliance was intended to retract the premaxilla as well as molding the nasal cartilage and elongating the columella. Their plate design included retention through extraoral taping and elastics. We have modified the design utilizing our principles of a self-retained appliance13,16,17 to avoid using facial taping to support the prosthesis. A light-cured resin plate is constructed to which orthodontic buttons or custom-formed wires are attached for retraction of the premaxilla with the elastomeric band. In addition the plate is relined with soft-tissue conditioner for close adaptation to the palatal tissues. After premaxillary retraction and repositioning are completed, the plate is modified by adding two wires that go into each nasal vestibule. The ends of the wires are bent in a loop and are covered with a light-cured acrylic covered with soft denture lining material (nasal stents). In addition, loops are bent about the level of the superior aspect of the prolabium for attachment of an elastomeric chain that has been covered with a soft-tissue denture liner. The purpose of the elastomeric chain across the prolabium is to hold it down, while the nasal prongs at the end of the wires are gradually elevated, lifting and medially repositioning the nasal domes and, at the same time, elongating the hypoplastic columella (Fig. 27.8). The plate is used 24 hours a day, is removed daily for cleaning, and is held in position with the aid of a denture adhesive cream. In addition, the palatal aspect of the plate can be modified by adding material on the lateral aspects of the plate and removing acrylic on the medial aspects. This will allow for gentle and gradual repositioning of the maxillary segments, resulting in narrowing of the cleft. This technique has given the surgeon an improved situation for not only obtaining adequate lip repair but also providing a better situation for primary nasal reconstruction with remodeling of the nasal domes and nasal tip and elongation of the hypoplastic columella. The main advantage of this procedure is that it eliminates the need for secondary procedures for columella elongation in the early childhood years. All of the patients in whom this technique has been used have adjusted extremely well to the use of the appliance and the families have been extremely pleased with the results (Fig. 28.9), as well as with the ease in which the orthopedic phase is carried out.
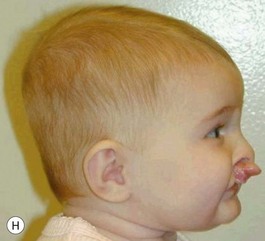
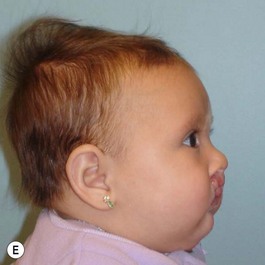
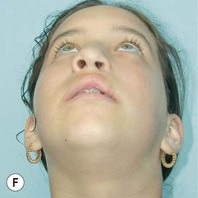
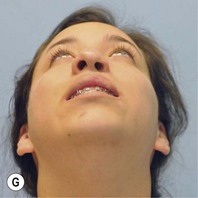
The described protocol has been well tolerated by patients and readily accepted by parents. This treatment protocol has been used for a few years and there are not enough long-term data to demonstrate the effects of the technique on the fully developed nasal structures. However, some patients are in the midteen years and the clinical impression at this time is that they will require less extensive nasal revision procedures at the completion of facial growth (Fig. 27.10).
Primary dentition
Posterior crossbite
In the cleft patient, posterior crossbites are of both skeletal and dental origin. They are skeletal because the maxillary segments are usually collapsed after cleft palate surgery, especially in the canine region. In most instances, this change in arch form occurs prior to the eruption of the primary canines; therefore, at the time of eruption of these teeth, the maxillary cleft-side primary canine erupts medially to the lower one. In addition, this early relationship causes minor palatal displacement of the maxillary primary canine and labial displacement of the mandibular one.3 This is an important observation, as this is the reason why cleft patients in the primary dentition rarely have occlusal or functional shifts. Patients in whom an occlusal shift is detected are those who are candidates for either selective tooth grinding or expansion procedures. Expansion can readily be accomplished but it should be noted that, after it is completed, unless a bone graft is placed, it has to be retained until the time of alveolar reconstruction with a bone graft. For this reason, we prefer to delay transverse expansion in the primary dentition until the patient is older and just prior to secondary alveolar bone-grafting procedures usually undertaken in the transitional dentition.
Anterior crossbite
Anterior crossbite of mild to moderate degree can be managed in the primary and transitional dentition stages utilizing elastic protraction forces delivered through a facial mask.18–20 However, if it is noted that this crossbite is related to a moderate to severe skeletal maxillary hypoplasia, the patient is best managed with a surgical approach. If it is felt that the maxillary advancement is important at an early age due to its severity, it can be instituted by means of distraction osteogenesis.
Liou and Tsai21 have introduced an intraoral technique for orthopedic advancement of the maxilla. They used a spring system with highly flexible wires to apply constant anterior pressure to the maxilla. Simultaneously they used a screw-type expander, which is regularly activated. After the screw reaches its limit, it is then turned backwards (contraction). This constant action results in activation of the circummaxillary suture complex and in this way maxillary protraction is obtained.22 The technique has been applied to both cleft and noncleft patients with impressive outcomes and superior to conventional face mask therapy.21
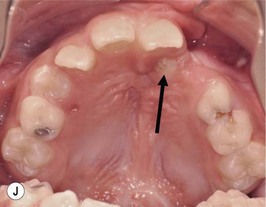
Transitional dentition
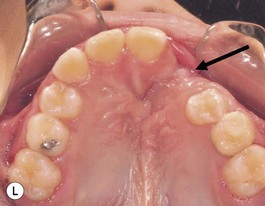
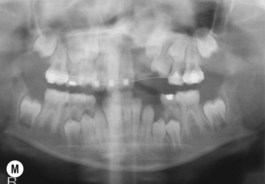
This is the developmental stage in which a cleft patient, involving the alveolus, will receive the next surgical procedure after lip and secondary palate repair. In most instances, the dentition around the cleft presents severe malposition, limiting surgical access to the alveolar site (Fig. 27.11). For this purpose, the dentition adjacent to the cleft has to be repositioned, preparing the cleft site for the secondary alveolar bone graft. Reconstruction of the cleft alveolus and anterior aspect of the maxilla is deferred until this stage, in an attempt to minimize the growth restriction resulting from surgical trauma and scarring.23–25