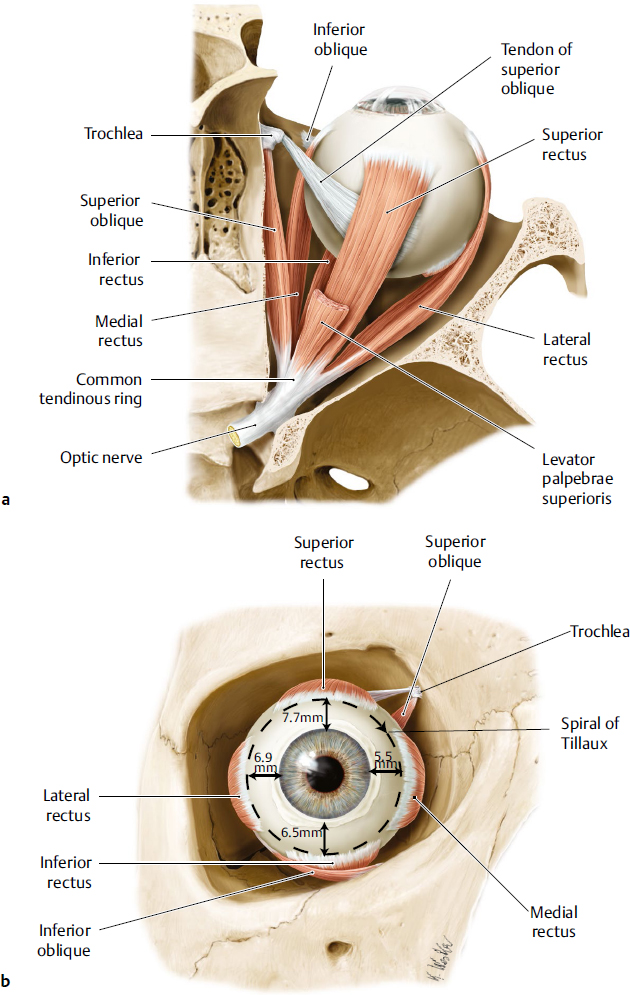
Extraocular Muscles and Innervation
The six extraocular muscles (medial, lateral, superior and inferior recti, and superior and inferior oblique muscles) move the globe. With the exception of the inferior oblique muscle, which originates on the anteromedial orbital floor, all the extraocular muscles originate at the orbital apex (Fig. 14.1a). The rectus muscles originate at the fibrous annulus of Zinn. These muscles course anteriorly, penetrate Tenon’s capsule, and insert onto the anterior aspect of the globe, forming the spiral of Tillaux (Fig. 14.1b). The rectus muscles form the muscle cone and delineate the intraconal and extraconal spaces.
The levator palpebrae superioris muscle originates on the lesser wing of sphenoid superior to the annulus. The superior oblique muscle also originates on the lesser wing of sphenoid medial to the levator muscle origin, continues anteriorly through the trochlea, then courses posterolaterally under the superior rectus muscle to insert onto the globe. The inferior oblique originates on the maxillary bone lateral to the lacrimal sac fossa, continues posterolaterally under the inferior rectus, and inserts onto the globe posterior to the macula.
The extraocular muscles are innervated by cranial nerves (CN) III (oculomotor), IV (trochlear), and VI (abducens). CN III divides into superior and inferior branches in the cavernous sinus before entering the orbit. The superior branch innervates the levator and superior rectus muscles. The inferior branch innervates the medial rectus, inferior rectus, and inferior oblique muscles. CN IV innervates the superior oblique muscle. CN VI innervates the lateral rectus muscle. Cranial nerves III and VI enter the orbit through the superior orbital fissure, travel through the intraconal space, and innervate the rectus muscles at the posterior one-third and anterior two-thirds junction. The blood supply for the rectus muscles arises from muscular anterior ciliary artery branches of the ophthalmic artery, lacrimal artery, and infraorbital artery. The inferior division of CN III to the inferior oblique travels lateral to the inferior rectus to innervate the muscle on the posterior surface. A parasympathetic branch to the ciliary ganglion travels with this inferior oblique muscle branch. CN IV travels extraconally to innervate the superior oblique on the superior surface at the posterior third of the muscle.
Optic Nerve
The optic nerve (CN II) can be divided into intraocular, intraorbital, intracanalicular, and intracranial segments measuring approximately 1 mm, 25 to 30 mm, 10 mm, and 10 mm long, respectively. The intraorbital optic nerve exits the posterior aspect of the globe and increases in diameter as it extends posteriorly through the orbit. Its intraorbital length is greater than the distance from the posterior globe to the optic canal (18 mm), allowing for eye movement and a safety margin in the event of proptosis. The optic nerve, with a 4-mm diameter and surrounded by the meninges (pia, arachnoid, and dura mater), then enters the optic foramen, which is 6.5 mm in diameter. Dura fuses with the annulus of Zinn and the optic canal periosteum, resulting in immobilization of the optic nerve. The optic nerve courses through the optic canal, which is about 10 mm long, and continues intracranially until it reaches the optic chiasm. Surgical management of intraconal pathology requires a keen understanding of the optic nerve course.
Orbital Nerves
In addition to the cranial nerves previously described, sensory, motor, and autonomic nerves supply the orbit.
Sensory Innervation
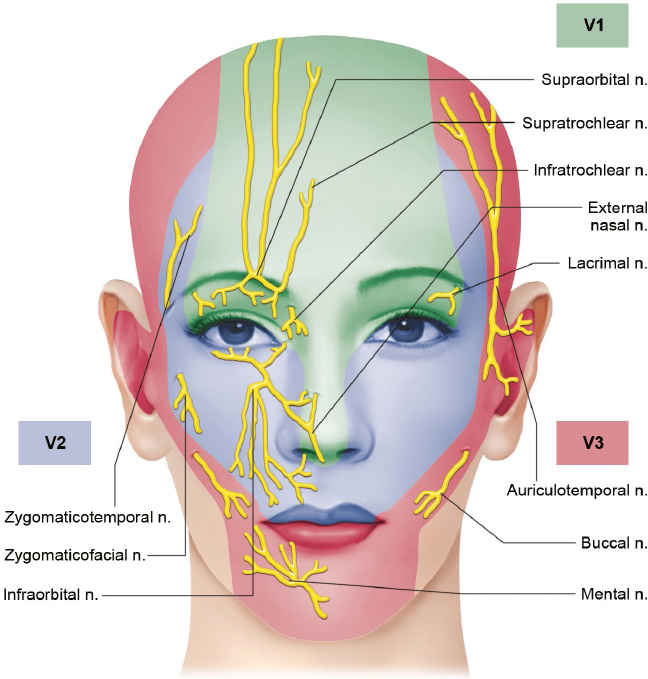
The ophthalmic (V1) and maxillary (V2) divisions of the trigeminal nerve (CN V) provide sensory innervation to the orbital and periorbital regions (Fig. 14.2).
Ophthalmic Nerve
The ophthalmic nerve (CN V1) divides into the frontal and lacrimal nerves, which enter the orbit above the annulus of Zinn, and the nasociliary nerve, which enters through the annulus. The frontal nerve divides further; the supratrochlear nerve innervates the medial upper lid, glabellar region, and medial conjunctiva, and the supraorbital nerve innervates the medial forehead. The lacrimal nerve innervates the lateral upper lid, lacrimal gland, and lateral conjunctiva. The nasociliary nerve crosses the optic nerve superiorly from lateral to medial and courses between the superior oblique and medial rectus muscles before further dividing. Anterior and posterior ethmoidal nerves innervate the middle and inferior turbinates, nasal septum, lateral nasal wall, and tip of the nose (terminal infratrochlear nerve). Ciliary nerves provide sensory innervation to the ciliary body, iris, and cornea along with sympathetic innervation to the dilator pupillae muscle.
Ciliary Ganglion
The ciliary ganglion, which is located lateral to the optic nerve and medial to the lateral rectus muscle, is about 1.5 cm posterior to the globe. Sensory (V1) and sympathetic fibers pass through without synapsing, whereas parasympathetic fibers synapse in the ganglion. The ganglion can be encountered during lateral orbital intraconal surgery.
Fig. 14.1 Extraocular muscles, right eye. (a) Superior view. (b) Anterior view. Muscle insertions onto the anterior aspect of the globe beginning with the medial rectus and ending with the superior rectus create the spiral of Tillaux. The distance between the muscle insertion and limbus are indicated. (Modified from THIEME Atlas of Anatomy, Head and Neuroanatomy. © Thieme 2010, Illustrations by Karl Wesker.)
Maxillary Nerve
The maxillary nerve (CN V2) divides into the infraorbital, zygomatic, nasal branches, palatine, superior alveolar, and pharyngeal nerves. After leaving the trigeminal ganglion, the maxillary nerve enters the foramen rotundum into the pterygopalatine fossa. The nerve enters the inferior orbital fissure to continue through the infraorbital groove and canal to exit anteriorly through the infraorbital foramen as the infraorbital nerve. The infraorbital nerve divides into the inferior palpebral branch, nasal branch, and superior labial branch to supply the inferior eyelid, lateral nose, and upper lip, respectively. The zygomatic nerve divides in the inferior orbital fissure into the zygomaticofacial and zygomaticotemporal nerves to exit through the respective foramina and innervate the cheek and lateral forehead, respectively.
The infraorbital, zygomaticofacial, and zygomaticotemporal may be encountered during surgery of the midface. Care should be taken to preserve these sensory nerves; however, compromise to the zygomaticofacial and zygomaticotemporal nerves may be less consequential than infraorbital nerve damage that may result in symptomatic hypoesthesia.
Motor Innervation
Motor innervation to the facial muscles is supplied by the facial nerve (CN VII), which is described in further detail along with facial anatomy in other chapters. In the periorbital region, the facial nerve lies in a deep plane as it emerges from the parotid gland (Fig. 14.3). The temporal branch courses superiorly and crosses over the zygomatic arch about midway between the lateral canthus and tragus. Dissection in the subperiosteal plane is safe in this region. Superior to the arch, the facial nerve lies beneath the superficial temporalis fascia, which is an extension of the superficial musculoaponeurotic system (SMAS). To avoid damaging the facial nerve in this region, dissection should be performed deep to SMAS, just anterior to the deep temporalis fascia. In addition, a branch can be found along a line from approximately 1 cm inferior to the tragus to 1.5 cm superior to the lateral brow. Inferior to the arch, dissection superficial to SMAS and the parotid gland avoids the facial nerve.
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree